Marfan Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Blueprint Genetics Comprehensive Growth Disorders / Skeletal
Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders Panel Test code: MA4301 Is a 374 gene panel that includes assessment of non-coding variants. This panel covers the majority of the genes listed in the Nosology 2015 (PMID: 26394607) and all genes in our Malformation category that cause growth retardation, short stature or skeletal dysplasia and is therefore a powerful diagnostic tool. It is ideal for patients suspected to have a syndromic or an isolated growth disorder or a skeletal dysplasia. About Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders This panel covers a broad spectrum of diseases associated with growth retardation, short stature or skeletal dysplasia. Many of these conditions have overlapping features which can make clinical diagnosis a challenge. Genetic diagnostics is therefore the most efficient way to subtype the diseases and enable individualized treatment and management decisions. Moreover, detection of causative mutations establishes the mode of inheritance in the family which is essential for informed genetic counseling. For additional information regarding the conditions tested on this panel, please refer to the National Organization for Rare Disorders and / or GeneReviews. Availability 4 weeks Gene Set Description Genes in the Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ACAN# Spondyloepimetaphyseal dysplasia, aggrecan type, AD/AR 20 56 Spondyloepiphyseal dysplasia, Kimberley -

Prenatalscreen® Standard Technical Report
About PrenatalScreen® Prenatal Test PrenatalScreen® Prenatal Test is a genetic test that analyses fetal DNA, obtained from CVS or amniotic fluid following an invasive prenatal diagnosis, to screen for monogenic disorders in the fetus. Using the latest technologies, including Next Generation Sequencing (NGS), PrenatalScreen® Prenatal Test screen 744 genes for mutations causing over 1.000 severe genetic disorders in the fetus. PrenatalScreen® Prenatal Test allows for a comprehensive care and enables patients to make more informed reproductive decisions. Offering PrenatalScreen® Prenatal Test to a patient during pregnancy allows her to gain more knowledge about the potential to pass along a condition to the fetus. Aim of the test PrenatalScreen® Prenatal Test analyses DNA extracted from fetal cells in the amniotic fluid, collected through amniocentesis, or in the chorionic villi through villocentesis (CVS). The aim of this diagnositc test is to assess severe genetic diseases in the fetus, including the most common diseases in the European population. Genes listed in Table 1 were selected according to the incidence in the population of the disease caused by mutations in such genes, the severity of the clinical phenotype at birth and the importance of the related pathogenetic picture, in accordance with the indications of the American College of Medical Genetics (ACMG)(Grody et al., Genet Med 2013:15:482–483). PrenatalScreen®: Indication for testing PrenatalScreen® Prenatal Test is intended for patients who meet any of the following criteria: • Personal/familial anamnesis of hereditary genetic diseases; • For expectant mothers wishing to reduce the risk of a genetic diseases in the fetus; • For natural or in vitro fertilization (IVF)-derived pregnancies: • For couples using heterologus IVF procedures (egg/sperm donors). -

Blueprint Genetics Comprehensive Skeletal Dysplasias and Disorders
Comprehensive Skeletal Dysplasias and Disorders Panel Test code: MA3301 Is a 251 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of disorders involving the skeletal system. About Comprehensive Skeletal Dysplasias and Disorders This panel covers a broad spectrum of skeletal disorders including common and rare skeletal dysplasias (eg. achondroplasia, COL2A1 related dysplasias, diastrophic dysplasia, various types of spondylo-metaphyseal dysplasias), various ciliopathies with skeletal involvement (eg. short rib-polydactylies, asphyxiating thoracic dysplasia dysplasias and Ellis-van Creveld syndrome), various subtypes of osteogenesis imperfecta, campomelic dysplasia, slender bone dysplasias, dysplasias with multiple joint dislocations, chondrodysplasia punctata group of disorders, neonatal osteosclerotic dysplasias, osteopetrosis and related disorders, abnormal mineralization group of disorders (eg hypopohosphatasia), osteolysis group of disorders, disorders with disorganized development of skeletal components, overgrowth syndromes with skeletal involvement, craniosynostosis syndromes, dysostoses with predominant craniofacial involvement, dysostoses with predominant vertebral involvement, patellar dysostoses, brachydactylies, some disorders with limb hypoplasia-reduction defects, ectrodactyly with and without other manifestations, polydactyly-syndactyly-triphalangism group of disorders, and disorders with defects in joint formation and synostoses. Availability 4 weeks Gene Set Description -

Sema4 Cardiac Information Sheet
CARDIAC NEXT-GENERATION SEQUENCING PANELS Mail: One Gustave L. Levy Place, Box 1497 1 CLIA #: 33D2097541 Specimens: 1428 Madison Ave, Atran Bldg, Rm 2-25 T: 800-298-6470 New York, NY 10029 F: 212-241-0139 www.sema4.com 0 3 8 Mail: One Gustave L. Levy Place, Box 1497 2 CLIA #: 33D2097541 Specimens: 1428 Madison Ave, Atran Bldg, Rm 2-25 T: 800-298-6470 New York, NY 10029 F: 212-241-0139 www.sema4.com Mail: One Gustave L. Levy Place, Box 1497 3 CLIA #: 33D2097541 Specimens: 1428 Madison Ave, Atran Bldg, Rm 2-25 T: 800-298-6470 New York, NY 10029 F: 212-241-0139 www.sema4.com Mail: One Gustave L. Levy Place, Box 1497 4 CLIA #: 33D2097541 Specimens: 1428 Madison Ave, Atran Bldg, Rm 2-25 T: 800-298-6470 New York, NY 10029 F: 212-241-0139 www.sema4.com TABLE OF CONTENTS GENETIC TESTING FOR INHERITED CARDIOVASCULAR CONDITIONS 6 GENETICS AND INDICATIONS 6 TESTING METHODS, SENSITIVITY, AND LIMITATIONS 7 TURNAROUND TIME 9 SPECIMEN AND SHIPPING REQUIREMENTS 9 CUSTOMER SERVICES AND GENETIC COUNSELING 10 THE COMPREHENSIVE CARDIOMYOPATHY PANEL 11 DILATED CARDIOMYOPATHY (DCM) SUBPANEL 23 ARRHYTHMOGENIC RIGHT VENTRICULAR CARDIOMYOPATHY (ARVC) SUBPANEL 28 HYPERTROPHIC CARDIOMYOPATHY (HCM) SUBPANEL 30 LEFT VENTRICULAR NON-COMPACTION CARDIOMYOPATHY (LVNC) SUBPANEL 33 THE COMPREHENSIVE ARRHYTHMIAS PANEL 35 BRUGADA SYNDROME (BRS) SUBPANEL 40 CATECHOLAMINERGIC POLYMORPHIC VENTRICULAR TACHYCARDIA (CPVT) SUBPANEL 42 LONG / SHORT QT SYNDROME (LQTS / SQTS) SUBPANEL 44 AORTOPATHIES PANEL 46 CONGENITAL HEART DISEASE (CHD) PANEL 49 FAMILIAL HYPERCHOLESTEROLEMIA (FH) PANEL 52 PULMONARY HYPERTENSION (PAH) PANEL 54 METABOLIC CARDIOMYOPATHY PANEL 55 NOONAN SPECTRUM DISORDERS PANEL 57 HEREDITARY HEMORRHAGIC TELANGIECTASIA PANEL 59 REFERENCES 60 DISCLAIMER 69 Mail: One Gustave L. -

The Phenotype/Genotype Relation and the Current QT
110 Heart 1997;78:1 10-116 REVIEW The phenotype/genotype relation and the current status of genetic screening in hypertrophic cardiomyopathy, Marfan syndrome, and the long QT syndrome J Burn, J Camm, M J Davies, L Peltonen, P J Schwartz, H Watkins Hypertrophic cardiomyopathy, Marfan syn- encode amino acids, but within the gene there drome, and the long QT syndrome are all are also non-functional sequences (introns). autosomal disorders inherited in a dominant The simplest single gene abnormality is a manner; affected individuals are heterozygous, point mutation in which one base pair is that is they have one normal and one mutant replaced by another. Because of the redun- copy of the gene but not all the gene carriers dancy in the genetic code, point mutations are symptomatic. This failure to express fully may be silent polymorphisms that do not the expected phenotype is traditionally known change the amino acid or they may be mis- as incomplete penetrance. sense mutations that change a single amino acid. Missense mutations can be regarded as analogous to simple spelling errors in one let- Vocabulary and technology ter of a word. For example "the fish is on the In the human genome (consisting of 22 pairs dish" becomes "the fish is on the fish". of autosomes and the X and Y chromosomes) Because each gene exists in a maternal and a there are between 50 000 and 100 000 indi- paternal copy the ultimate product of the gene vidual genes coding for a wide range of prod- is a combination of normal (wild type) and ucts including enzymes and structural abnormal (mutant type). -

Marfan Syndrome Precision Panel Overview Indications Clinical Utility
Marfan Syndrome Precision Panel Overview Marfan Syndrome (MFS) is a spectrum of disorders caused by a genetic defect of the connective tissue and it is inherited in an autosomal dominant pattern. Since the connective tissue is the tissue that helps body growth as well as serving as a scaffold for cells and organs, Marfan Syndrome is a pleiotropic syndrome affecting mainly musculoskeletal, cardiac and ocular systems. The most severe of these manifestations include aortic root dilation and dissection, which are responsible for early patient demise. Pregnancy is a time of increased cardiovascular risk for women with Marfan syndrome, so an early diagnosis is key in pregnancy management. The Igenomix Marfan Syndrome Precision Panel can be used to make an accurate and directed diagnosis as well as a differential diagnosis of connective tissue disorders due to their overlapping phenotypic features ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Marfan Syndrome Precision Panel is indicated for those patients with a clinical suspicion or diagnosis with or without the following manifestations: - Subluxation of lenses - Cardiovascular findings: mitral valve prolapse, aortic regurgitation, mitral regurgitation, aortic dilation, dissection or aneurysm - Tall and thin stature - Long fingers and toes - Pectus carinatum or excavatum - Scoliosis - Hypermobile joints - Severe hindfoot valgus Clinical Utility The clinical utility of this panel is: - The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient. Understanding global and molecular functions of fibrillin containing microfibrils for the development of a comprehensive theory of pathogenesis. -

Whole Exome Sequencing Gene Package Skeletal Dysplasia, Version 2.1, 31-1-2020
Whole Exome Sequencing Gene package Skeletal Dysplasia, Version 2.1, 31-1-2020 Technical information DNA was enriched using Agilent SureSelect DNA + SureSelect OneSeq 300kb CNV Backbone + Human All Exon V7 capture and paired-end sequenced on the Illumina platform (outsourced). The aim is to obtain 10 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate and non-unique reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA-MEM algorithm (reference: http://bio-bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x ABCC9 Atrial fibrillation, familial, 12, 614050 601439 65 100 100 95 Cardiomyopathy, dilated, 1O, 608569 Hypertrichotic osteochondrodysplasia, 239850 ACAN Short stature and advanced bone age, with or without early-onset osteoarthritis -
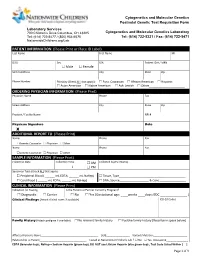
PATIENT INFORMATION (Please Print Or Place ID Label) Last Name First Name MI
Cytogenetics and Molecular Genetics Postnatal Genetic Test Requisition Form Laboratory Services 700 Children’s Drive Columbus, OH 43205 Cytogenetics and Molecular Genetics Laboratory Tel: (614) 722-5477 / (800) 934-6575 Tel: (614) 722-5321 / Fax: (614) 722-5471 NationwideChildrens.org/Lab PATIENT INFORMATION (Please Print or Place ID Label) Last Name First Name MI DOB Sex SSN Patient ID # / MRN Male Female Street Address City State Zip Phone Number Ethnicity (Check ALL that apply): Euro. Caucasian African American Hispanic Asian American Native American Ash. Jewish Other______________________ ORDERING PHYSICIAN INFORMATION (Please Print) Physician Name Phone Fax Street Address City State Zip Practice / Facility Name NPI # Physican Signature Date X ADDITIONAL REPORT TO (Please Print) Name Phone Fax Genetic Counselor Physician Other Name Phone Fax Genetic Counselor Physician Other SAMPLE INFORMATION (Please Print) Collection Date Collection Time AM Collected by (Full Name) : PM Specimen Type (Check ALL that apply): Peripheral Blood ( ______ mL EDTA; ______ mL NaHep) Tissue, Type_________________________________________ Cord Blood ( ______ mL EDTA; ______ mL NaHep) DNA, Source__________________ & Conc.________________ CLINICAL INFORMATION (Please Print) Indication for Testing Is the Patient or Partner Currently Pregnant? Diagnostic Carrier No Yes (Gestational age: ____weeks ____days; EDC _______________ ) Clinical Findings (Attach clinical notes if available) ICD-10 Codes Family History (Attach pedigree if available) -

Mass Phenotype
MASS PHENOTYPE MASS Phenotype is a connective tissue disorder that is similar to Marfan syndrome in that people with the condition have the similar Mitral valve, Aorta, Skin, and Skeletal features. People with MASS phenotype do not have lens dislocation and do not show progressive and dangerous aortic root enlargement, hallmark features of Marfan syndrome. MASS phenotype is similar to Marfan syndrome, but does not have dangerous aortic root enlargement. What other names do people use for MASS phenotype? MASS phenotype is also known as MASS syndrome. How prevalent is MASS phenotype? There aren’t any good estimates regarding the prevalence of MASS phenotype. What are the characteristics of MASS phenotype? The features of MASS phenotype are: • Mitral valve prolapse (MVP), a condition in which the mitral valve of the heart closes properly, but then flops backward, which allows blood to leak into the chamber from which it came instead of moving forward. This leaking is called regurgitation • Aortic root diameter may be at the upper limits of normal for the person’s body size, but it does not worsen over time. In addition, it does not increase the risk of aortic dissection. MARFAN.ORG | 800-8-MARFAN EXT. 126 | [email protected] MASS PHENOTYPE page 2 • Skin stretch marks unrelated to weight change (striae). • Skeletal (bone and joint) features of Marfan syndrome (including scoliosis, chest wall deformities , and joint hypermobility). What causes MASS phenotype? MASS phenotype can be caused by a change in the FBN1 (fibrillin-1) gene, the same gene that causes Marfan syndrome. It can be inherited within families (passed down through generations). -

86A1bedb377096cf412d7e5f593
Contents Gray..................................................................................... Section: Introduction and Diagnosis 1 Introduction to Skin Biology ̈ 1 2 Dermatologic Diagnosis ̈ 16 3 Other Diagnostic Methods ̈ 39 .....................................................................................Blue Section: Dermatologic Diseases 4 Viral Diseases ̈ 53 5 Bacterial Diseases ̈ 73 6 Fungal Diseases ̈ 106 7 Other Infectious Diseases ̈ 122 8 Sexually Transmitted Diseases ̈ 134 9 HIV Infection and AIDS ̈ 155 10 Allergic Diseases ̈ 166 11 Drug Reactions ̈ 179 12 Dermatitis ̈ 190 13 Collagen–Vascular Disorders ̈ 203 14 Autoimmune Bullous Diseases ̈ 229 15 Purpura and Vasculitis ̈ 245 16 Papulosquamous Disorders ̈ 262 17 Granulomatous and Necrobiotic Disorders ̈ 290 18 Dermatoses Caused by Physical and Chemical Agents ̈ 295 19 Metabolic Diseases ̈ 310 20 Pruritus and Prurigo ̈ 328 21 Genodermatoses ̈ 332 22 Disorders of Pigmentation ̈ 371 23 Melanocytic Tumors ̈ 384 24 Cysts and Epidermal Tumors ̈ 407 25 Adnexal Tumors ̈ 424 26 Soft Tissue Tumors ̈ 438 27 Other Cutaneous Tumors ̈ 465 28 Cutaneous Lymphomas and Leukemia ̈ 471 29 Paraneoplastic Disorders ̈ 485 30 Diseases of the Lips and Oral Mucosa ̈ 489 31 Diseases of the Hairs and Scalp ̈ 495 32 Diseases of the Nails ̈ 518 33 Disorders of Sweat Glands ̈ 528 34 Diseases of Sebaceous Glands ̈ 530 35 Diseases of Subcutaneous Fat ̈ 538 36 Anogenital Diseases ̈ 543 37 Phlebology ̈ 552 38 Occupational Dermatoses ̈ 565 39 Skin Diseases in Different Age Groups ̈ 569 40 Psychodermatology -

Scleroderma Mimics - Clinical Features and Management
Mimics of systemic sclerosis and inflammatory muscle disease Scleroderma mimics - clinical features and management Catherine H Orteu1 Voon H. Ong2 Christopher P. Denton2 1Department of Dermatology, Royal Free London NHS Foundation Trust, Pond Street, London NW3 2QG 2Centre for Rheumatology, Royal Free Campus, University College London, Rowland Hill Street, London NW3 2PF Correspondence Professor Christopher Denton Centre for Rheumatology, Royal Free Campus, University College London, Rowland Hill Street, London NW3 2PF [email protected] 1 Mimics of systemic sclerosis and inflammatory muscle disease Scleroderma is often used as a synonym for systemic sclerosis but is perhaps better seen as a collective term covering a range of autoimmune inflammatory conditions in which skin thickening or sclerosis is a hallmark feature. Consensus has emerged that includes localised and systemic forms of scleroderma in a classification that is highlighted in Figure 1. This is sometimes termed the scleroderma spectrum and provides a very useful operational framework for management of the conditions. The term morphoea has recently been applied more consistently to the localised forms of scleroderma and this helps to avoid confusion with patients and clinical staff. There are several other conditions which may be pathogenetically or clinically related to scleroderma that represent diagnostic mimics, and these “pseudo-sclerodermas” are the main focus of this chapter. Establishing the underlying cause and correct diagnosis in a patient with diffuse skin thickening is important because disease impact, prognosis and management vary widely between systemic sclerosis, morphoea and the scleroderma mimics. Practical approach When skin thickening or tightness is observed this should prompt further clinical and laboratory assessment and the tools available generally permit a reliable differentiation between scleroderma and each of the scleroderma mimics. -

Mallory Prelims 27/1/05 1:16 Pm Page I
Mallory Prelims 27/1/05 1:16 pm Page i Illustrated Manual of Pediatric Dermatology Mallory Prelims 27/1/05 1:16 pm Page ii Mallory Prelims 27/1/05 1:16 pm Page iii Illustrated Manual of Pediatric Dermatology Diagnosis and Management Susan Bayliss Mallory MD Professor of Internal Medicine/Division of Dermatology and Department of Pediatrics Washington University School of Medicine Director, Pediatric Dermatology St. Louis Children’s Hospital St. Louis, Missouri, USA Alanna Bree MD St. Louis University Director, Pediatric Dermatology Cardinal Glennon Children’s Hospital St. Louis, Missouri, USA Peggy Chern MD Department of Internal Medicine/Division of Dermatology and Department of Pediatrics Washington University School of Medicine St. Louis, Missouri, USA Mallory Prelims 27/1/05 1:16 pm Page iv © 2005 Taylor & Francis, an imprint of the Taylor & Francis Group First published in the United Kingdom in 2005 by Taylor & Francis, an imprint of the Taylor & Francis Group, 2 Park Square, Milton Park Abingdon, Oxon OX14 4RN, UK Tel: +44 (0) 20 7017 6000 Fax: +44 (0) 20 7017 6699 Website: www.tandf.co.uk All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior permission of the publisher or in accordance with the provisions of the Copyright, Designs and Patents Act 1988 or under the terms of any licence permitting limited copying issued by the Copyright Licensing Agency, 90 Tottenham Court Road, London W1P 0LP. Although every effort has been made to ensure that all owners of copyright material have been acknowledged in this publication, we would be glad to acknowledge in subsequent reprints or editions any omissions brought to our attention.