Marfan Syndrome Diagnostics, Epidemiology, and Aortic Events
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Marfan Syndrome Precision Panel Overview Indications Clinical Utility
Marfan Syndrome Precision Panel Overview Marfan Syndrome (MFS) is a spectrum of disorders caused by a genetic defect of the connective tissue and it is inherited in an autosomal dominant pattern. Since the connective tissue is the tissue that helps body growth as well as serving as a scaffold for cells and organs, Marfan Syndrome is a pleiotropic syndrome affecting mainly musculoskeletal, cardiac and ocular systems. The most severe of these manifestations include aortic root dilation and dissection, which are responsible for early patient demise. Pregnancy is a time of increased cardiovascular risk for women with Marfan syndrome, so an early diagnosis is key in pregnancy management. The Igenomix Marfan Syndrome Precision Panel can be used to make an accurate and directed diagnosis as well as a differential diagnosis of connective tissue disorders due to their overlapping phenotypic features ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Marfan Syndrome Precision Panel is indicated for those patients with a clinical suspicion or diagnosis with or without the following manifestations: - Subluxation of lenses - Cardiovascular findings: mitral valve prolapse, aortic regurgitation, mitral regurgitation, aortic dilation, dissection or aneurysm - Tall and thin stature - Long fingers and toes - Pectus carinatum or excavatum - Scoliosis - Hypermobile joints - Severe hindfoot valgus Clinical Utility The clinical utility of this panel is: - The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient. Understanding global and molecular functions of fibrillin containing microfibrils for the development of a comprehensive theory of pathogenesis. -

Marfan Syndrome
Marfan Syndrome Marfan syndrome (MFS) is a connective tissue disorder that exhibits a high degree of clinical variability. Clinical symptoms typically involve the cardiovascular, ocular, and skeletal systems. Early diagnosis is crucial for treatment of skeletal, orthopedic, and Tests to Consider cardiovascular abnormalities. The diagnosis of MFS can be made or suspected based on established clinical criteria (see below). MFS is caused by pathogenic variants in the FBN1 Marfan Syndrome (FBN1) Sequencing and gene; however, there is signicant overlap of the clinical features with syndromes caused by Deletion/Duplication 2005584 pathogenic variants in other genes. Method: Polymerase Chain Reaction/Sequencing/Multiplex Ligation-dependent Probe Amplication Preferred test to conrm diagnosis when MFS is Disease Overview strongly suspected by consensus criteria Marfan Syndrome, FBN1 Sequencing Prevalence 2005589 Method: Polymerase Chain Reaction/Sequencing 1/5,000-10,000 Acceptable test to conrm diagnosis for individuals with clinical phenotype of MFS Symptoms Related Tests A clinical diagnosis of MFS in an individual without a family history of MFS (when Shprintzen-Goldberg syndrome [SGS], Loeys-Dietz syndrome [LDS], and Ehlers-Danlos Aortopathy Panel, Sequencing and Deletion/Duplication 2006540 syndrome type IV [EDS IV] have been excluded) is based on the presence of any of the Method: Massively Parallel Sequencing/Exonic following: Oligonucleotide-based CGH Microarray Aortic root dilatation or dissection and ectopia lentis Aortic root dilatation -
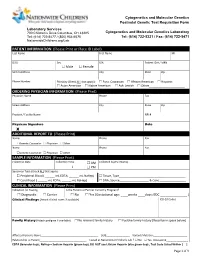
PATIENT INFORMATION (Please Print Or Place ID Label) Last Name First Name MI
Cytogenetics and Molecular Genetics Postnatal Genetic Test Requisition Form Laboratory Services 700 Children’s Drive Columbus, OH 43205 Cytogenetics and Molecular Genetics Laboratory Tel: (614) 722-5477 / (800) 934-6575 Tel: (614) 722-5321 / Fax: (614) 722-5471 NationwideChildrens.org/Lab PATIENT INFORMATION (Please Print or Place ID Label) Last Name First Name MI DOB Sex SSN Patient ID # / MRN Male Female Street Address City State Zip Phone Number Ethnicity (Check ALL that apply): Euro. Caucasian African American Hispanic Asian American Native American Ash. Jewish Other______________________ ORDERING PHYSICIAN INFORMATION (Please Print) Physician Name Phone Fax Street Address City State Zip Practice / Facility Name NPI # Physican Signature Date X ADDITIONAL REPORT TO (Please Print) Name Phone Fax Genetic Counselor Physician Other Name Phone Fax Genetic Counselor Physician Other SAMPLE INFORMATION (Please Print) Collection Date Collection Time AM Collected by (Full Name) : PM Specimen Type (Check ALL that apply): Peripheral Blood ( ______ mL EDTA; ______ mL NaHep) Tissue, Type_________________________________________ Cord Blood ( ______ mL EDTA; ______ mL NaHep) DNA, Source__________________ & Conc.________________ CLINICAL INFORMATION (Please Print) Indication for Testing Is the Patient or Partner Currently Pregnant? Diagnostic Carrier No Yes (Gestational age: ____weeks ____days; EDC _______________ ) Clinical Findings (Attach clinical notes if available) ICD-10 Codes Family History (Attach pedigree if available) -

Skeletal Manifestations of Marfan Syndrome Associated to Heterozygous R2726W FBN1 Variant: Sibling Case Report and Literature Review Octavio D
Reyes-Hernández et al. BMC Musculoskeletal Disorders (2016) 17:79 DOI 10.1186/s12891-016-0935-9 CASE REPORT Open Access Skeletal manifestations of Marfan syndrome associated to heterozygous R2726W FBN1 variant: sibling case report and literature review Octavio D. Reyes-Hernández1†, Carmen Palacios-Reyes1†, Sonia Chávez-Ocaña1, Enoc M. Cortés-Malagón1, Patricia Garcia Alonso-Themann2, Víctor Ramos-Cano3, Julián Ramírez-Bello4 and Mónica Sierra-Martínez1* Abstract Background: FBN1 (15q21.1) encodes fibrillin-1, a large glycoprotein which is a major component of microfibrils that are widely distributed in structural elements of elastic and non-elastic tissues. FBN1 variants are responsible for the related connective tissue disorders, grouped under the generic term of type-1 fibrillinopathies, which include Marfan syndrome (MFS), MASS syndrome (Mitral valve prolapse, Aortic enlargement, Skin and Skeletal findings, Acromicric dysplasia, Familial ectopia lentis, Geleophysic dysplasia 2, Stiff skin syndrome, and dominant Weill-Marchesani syndrome. Case presentation: Two siblings presented with isolated skeletal manifestations of MFS, including severe pectus excavatum, elongated face, scoliosis in one case, and absence of other clinical features according to Ghent criteria diagnosis, were screened for detection of variants in whole FBN1 gene (65 exons). Both individuals were heterozygous for the R2726W variant. This variant has been previously reported in association with some skeletal features of Marfan syndrome in the absence of both tall stature and non-skeletal features. These features are consistent with the presentation of the siblings reported here. Conclusion: The presented cases confirm that the R2726W FBN1 variant is associated with skeletal features of MFS in the absence of cardiac or ocular findings. -

Molecular Genetics of the Fibrillinopathies Mélodie Aubart, Louise Benarroch, Pauline Arnaud, Gwenaelle Collod-Beroud, Guillaume Jondeau, Catherine Boileau
Molecular Genetics of the Fibrillinopathies Mélodie Aubart, Louise Benarroch, Pauline Arnaud, Gwenaelle Collod-Beroud, Guillaume Jondeau, Catherine Boileau To cite this version: Mélodie Aubart, Louise Benarroch, Pauline Arnaud, Gwenaelle Collod-Beroud, Guillaume Jon- deau, et al.. Molecular Genetics of the Fibrillinopathies. eLS, John Wiley & Sons, 2016, 10.1002/9780470015902.a0025314. hal-01682320 HAL Id: hal-01682320 https://hal-amu.archives-ouvertes.fr/hal-01682320 Submitted on 12 Jan 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Molecular Genetics of Advanced article Article Contents the Fibrillinopathies • Introduction ⋆ • Fibrillins Mélodie Aubart , Laboratory for Vascular Translational Science, INSERM • FBN1 Mutation-Associated Disorders U1148, Paris, France • FBN2-Mutation-Associated Disorders: Congenital Contractural Arachnodactyly (CCA) or Beals Louise Benarroch, Laboratory for Vascular Translational Science, INSERM Syndromes U1148, Paris, France • Animal Models • Pauline Arnaud, Laboratory for Vascular Translational Science, INSERM -

A Review of the Type-1 Fibrillinopathies: Pathophysiology
ndrom Sy es tic & e G n e e n Journal of Genetic Syndrome and G e f T o h l e a Cale et al., J Genet Syndr Gene Ther 2018, 9:1 r n a r p u y o J Gene Therapy DOI: 10.4172/2157-7412.1000323 ISSN: 2157-7412 Research Article Open Access A Review of the Type-1 Fibrillinopathies: Pathophysiology, Diagnosis and Novel Therapeutic Strategies Jessica M Cale1,2, Sue Fletcher1,2 and Steve D Wilton1,2* 1Molecular Therapy Laboratory, Centre for Comparative Genomics, Murdoch University, Health Research Building, Discovery Way, Western Australia 2Perron Institute for Neurological and Translational Science, Sarich Neuroscience Institute, University of Western Australia, Verdun Street, Western Australia *Corresponding author: Steve D Wilton, Centre for Comparative Genomics, Murdoch University, 90 South Street, Murdoch, Western Australia, Tel: +61 8 9360 2305; E- mail: [email protected] Received date: December 6, 2017; Accepted date: January 12, 2018; Published date: January 20, 2018 Copyright: © 2018 Cale JM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Type-1 fibrillinopathies are a family of connective tissue disorders with major clinical manifestations in the skeletal, ocular and cardiovascular systems. The type-1 fibrillinopathies are caused by mutations in the fibrillin-1 gene (FBN1), which encodes fibrillin-1, a large glycoprotein and a major component of the extracellular matrix microfibrils, providing both structural and regulatory support to connective tissues. -

FBN1 Gene Fibrillin 1
FBN1 gene fibrillin 1 Normal Function The FBN1 gene provides instructions for making a large protein called fibrillin-1. This protein is transported out of cells into the extracellular matrix, which is an intricate lattice of proteins and other molecules that forms in the spaces between cells. In this matrix, molecules of fibrillin-1 attach (bind) to each other and to other proteins to form threadlike filaments called microfibrils. Microfibrils form elastic fibers, which enable the skin, ligaments, and blood vessels to stretch. Microfibrils also provide support to more rigid tissues such as bones and the tissues that support the nerves, muscles, and lenses of the eyes. Microfibrils store a protein called transforming growth factor beta (TGF-b ), a critical growth factor. TGF-b affects development by helping to control the growth and division ( proliferation) of cells, the process by which cells mature to carry out specific functions ( differentiation), cell movement (motility), and the self-destruction of cells (apoptosis). Microfibrils help regulate the availability of TGF-b , which is turned off (inactivated) when stored in microfibrils and turned on (activated) when released. Health Conditions Related to Genetic Changes Acromicric dysplasia At least nine FBN1 gene mutations have been identified in people with acromicric dysplasia. This condition is characterized by severely short stature, short limbs, stiff joints, and distinctive facial features. FBN1 gene mutations that cause acromicric dysplasia are located in an area of the gene called exons 41 and 42, and change single protein building blocks (amino acids) in a region of the fibrillin-1 protein called TGF-b binding-protein-like domain 5. -

Medical & Clinical Case Reports
Alina Draga Belengeanu et.al., Ann Case Rep 2018, Volume 3 DOI: 10.29011/2574-7754-C1-006 2nd Global Congress on Medical & Clinical Case Reports November 19–20, 2018 Dubai, UAE New born with progeroid facial features lipodystrophy and marfanoid features - Romanian case 1Alina Draga Belengeanu, 2Daniela Eugenia Popescu, 3Cristina Popescu, 3Silvia Vuculescu and 3Valerica Belengeanu 1"Victor Babes" University of Medicine and Pharmacy, Romania 2Premiere Clinical Hospital Timişoara, Romania 3West University "Vasile Goldis", Arad, Romania Fibrillinopathies are a large heterogeneous group of genetic disorders with distinct effects on differential allelic expression of mutations in the fibrillin-1 gene (FBN1). Different mutations in the gene have been associated with a variety of conditions including Marfan syndrome, MASS syndrome, isolated ectopia lentis syndrome, thoracic aortic aneurysms, WeilleMarchesani syndrome, geleophysic and acromicric dysplasia, and stiff skin syndrome, and Marfan-progeroid-lipodystrophy syndrome. Up to now, seven cases have been reported in the literature, all with a specific gene mutation, type mutation is a truncating mutation in the penultimate exon, i.e., exon 64, in the gene FBN1. Here, we report on a newborn with senile facial appearance with distinctive facial features, with additional manifestations of Marfan syndrome and severe congenital lipodystrophy. The newborn is first child and was born at 39 weeks of gestation to non-consanguineous Caucasian young parents, apparently healthy. The birth weight was 2,600 -

WES Gene Package Aneurysm.Xlsx
Whole Exome Sequencing Gene package Aneurysm, version 2, 8‐7‐2016 Technical information After DNA was enriched using Agilent Sureselect Clinical Research Exome (CRE) Capture, samples were run on the Illumina Hiseq platform. The aim is to obtain 50 million total reads per exome with a mapped fraction >0.98. The average coverage of the exome is ~50x. Data are demultiplexed by Illumina software bcl2fastq. Reads are mapped to the genome using BWA (reference: http://bio‐bwa.sourceforge.net/). Variant detection is performed by Genome Analysis Toolkit (reference: http://www.broadinstitute.org/gatk/). Analysis is performed in Cartagenia using The Variant Calling File (VCF) followed by filtering. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered gene symbol gene ID >10x >20x ACTA2 Aortic aneurysm, familial thoracic 6, 611788 102620 96 100 100 Multisystemic smooth muscle dysfunction syndrome, 613834 Moyamoya disease 5, 614042 BGN No OMIM phenotype 301870 63 100 100 COL3A1 Ehlers‐Danlos syndrome, type IV, 130050 120180 63 99 93 COL5A1 Ehlers‐Danlos syndrome, classic type, 130000 120215 77 99 97 EFEMP2 Cutis laxa, autosomal recessive, type IB, 614437 604633 82 100 100 ELN Supravalvar -

Characterization of Two Novel Intronic Variants Affecting Splicing in FBN1
G C A T T A C G G C A T genes Article Characterization of Two Novel Intronic Variants Affecting Splicing in FBN1-Related Disorders Carmela Fusco 1,*, Silvia Morlino 2, Lucia Micale 1, Alessandro Ferraris 2, Paola Grammatico 2 and Marco Castori 1 1 Division of Medical Genetics, Fondazione IRCCS-Casa Sollievo della Sofferenza, 71013 San Giovanni Rotondo FG, Italy; [email protected] (L.M.); [email protected] (M.C.) 2 Laboratory of Medical Genetics, Department of Molecular Medicine, Sapienza University, San Camillo-Forlaninin Hospital, 00152 Rome, Italy; [email protected] (S.M.); [email protected] (A.F.); [email protected] (P.G.) * Correspondence: [email protected]; Tel.: +39-0882-416350 Received: 19 April 2019; Accepted: 7 June 2019; Published: 10 June 2019 Abstract: FBN1 encodes fibrillin 1, a key structural component of the extracellular matrix, and its variants are associated with a wide range of hereditary connective tissues disorders, such as Marfan syndrome (MFS) and mitral valve–aorta–skeleton–skin (MASS) syndrome. Interpretations of the genomic data and possible genotype–phenotype correlations in FBN1 are complicated by the high rate of intronic variants of unknown significance. Here, we report two unrelated individuals with the FBN1 deep intronic variants c.6872-24T>A and c.7571-12T>A, clinically associated with MFS and MASS syndrome, respectively. The individual carrying the c.6872-24T>A variant is positive for aortic disease. Both individuals lacked ectopia lentis. In silico analysis and subsequent mRNA study by RT-PCR demonstrated the effect of the identified variant on the splicing process in both cases. -

Recessive Gene List V2.0
Gene Disease AAAS ACHALASIA-ADDISONIANISM-ALACRIMA SYNDROME; AAAS [AR] LEUKOENCEPHALOPATHY. PROGRESSIVE. WITH OVARIAN FAILURE; LKENP [AR] | COMBINED OXIDATIVE PHOSPHORYLATION AARS2 DEFICIENCY 8; COXPD8 [AR] AASS HYPERLYSINEMIA. TYPE I [AR] ABAT GABA-TRANSAMINASE DEFICIENCY [AR] ICHTHYOSIS. CONGENITAL. AUTOSOMAL RECESSIVE 4B; ARCI4B [AR] | ICHTHYOSIS. CONGENITAL. AUTOSOMAL RECESSIVE 4A; ARCI4A ABCA12 [AR] ABCA3 SURFACTANT METABOLISM DYSFUNCTION. PULMONARY. 3; SMDP3 [AR] MACULAR DEGENERATION. AGE-RELATED. 2; ARMD2 [AD] | STARGARDT DISEASE 1; STGD1 [AR] | RETINITIS PIGMENTOSA 19; RP19 ABCA4 [AR] ABCB11 CHOLESTASIS. BENIGN RECURRENT INTRAHEPATIC. 2; BRIC2 [AR] | CHOLESTASIS. PROGRESSIVE FAMILIAL INTRAHEPATIC. 2; PFIC2 [AR] GALLBLADDER DISEASE 1; GBD1 [AD] | CHOLESTASIS. INTRAHEPATIC. OF PREGNANCY 3; ICP3 [AD] | CHOLESTASIS. PROGRESSIVE ABCB4 FAMILIAL INTRAHEPATIC. 3; PFIC3 [AR] ABCB7 ANEMIA. SIDEROBLASTIC. AND SPINOCEREBELLAR ATAXIA; ASAT [XLR] ABCC2 DUBIN-JOHNSON SYNDROME; DJS [AR] ARTERIAL CALCIFICATION. GENERALIZED. OF INFANCY. 2; GACI2 [AR] | PSEUDOXANTHOMA ELASTICUM. FORME FRUSTE [AD] | ABCC6 PSEUDOXANTHOMA ELASTICUM; PXE [AR] DIABETES MELLITUS. PERMANENT NEONATAL; PNDM [AD] | HYPERINSULINEMIC HYPOGLYCEMIA. FAMILIAL. 1; HHF1 [AD] | DIABETES ABCC8 MELLITUS. NONINSULIN-DEPENDENT; NIDDM [AD] | HYPOGLYCEMIA. LEUCINE-INDUCED; LIH [AD] ABCD1 ADRENOLEUKODYSTROPHY; ALD [XLR] ABCG5 Sitosterolemia 2 618666 (3) ABCG8 SITOSTEROLEMIA 1; STSL1 [AR] ABHD12 POLYNEUROPATHY. HEARING LOSS. ATAXIA. RETINITIS PIGMENTOSA. AND CATARACT; PHARC [AR] ABHD5 CHANARIN-DORFMAN SYNDROME; CDS [AR] ACAD8 ISOBUTYRYL-CoA DEHYDROGENASE DEFICIENCY; IBDD [AR] ACAD9 MITOCHONDRIAL COMPLEX I DEFICIENCY. NUCLEAR TYPE 20; MC1DN20 [AR] ACADM ACYL-CoA DEHYDROGENASE. MEDIUM-CHAIN. DEFICIENCY OF; ACADMD [AR] ACADS ACYL-CoA DEHYDROGENASE. SHORT-CHAIN. DEFICIENCY OF; ACADSD [AR] ACADSB 2-METHYLBUTYRYL-CoA DEHYDROGENASE DEFICIENCY [AR] ACADVL ACYL-CoA DEHYDROGENASE. VERY LONG-CHAIN. DEFICIENCY OF; ACADVLD [AR] SPONDYLOEPIMETAPHYSEAL DYSPLASIA. AGGRECAN TYPE; SEMDAG [AR] | SPONDYLOEPIPHYSEAL DYSPLASIA.