Product Monograph Fosrenol®*
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
How to Take Your Phosphate Binders
How to take your phosphate binders Information for renal patients Oxford Kidney Unit Page 2 What are phosphate binders? To reduce the amount of phosphate you absorb from your food you may have been prescribed a medicine called a phosphate binder. Phosphate binders work by binding (attaching) to some of the phosphate in food. This will reduce the amount of phosphate being absorbed into your blood stream. A list of phosphate binders and how to take them is shown below. Phosphate binder How to take it Calcichew (calcium carbonate) Chew thoroughly 10-15 minutes before or immediately before food Renacet (calcium acetate) Phosex (calcium acetate) Osvaren (calcium acetate and magnesium carbonate) Swallow whole after the first Renagel 2-3 mouthfuls of food (sevelemer hydrochloride) Renvela tablets (sevelemer carbonate) Alucaps (aluminium hydroxide) Renvela powder Dissolve in 60ml of water and (sevelemer carbonate) take after the first 2-3 mouthfuls of food Fosrenol tablets Chew thoroughly towards the (lanthanum carbonate) end/immediately after each meal Fosrenol powder Mix with a small amount of (lanthanum carbonate) food and eat immediately Velphoro Chew thoroughly after the first (sucroferric oxyhydroxide) 2-3 mouthfuls The phosphate binder you have been prescribed is: ……………………………………………………………………………………………………………………………………………………….. Page 3 How many phosphate binders should I take? You should follow the dose that has been prescribed for you. Your renal dietitian can advise how best to match your phosphate binders to your meal pattern, as well as which snacks require a phosphate binder. What happens if I forget to take my phosphate binder? For best results, phosphate binders should be taken as instructed. -

Effect of Lanthanum Carbonate and Calcium Acetate in the Treatment of Hyperphosphatemia in Patients of Chronic Kidney Disease P
Research Article Effect of lanthanum carbonate and calcium acetate in the treatment of hyperphosphatemia in patients of chronic kidney disease P. Thomas Scaria, Reneega Gangadhar1, Ramdas Pisharody2 ABSTRACT OObjectives:bjectives: The tolerability and efficacy of lanthanum carbonate has not been studied in the Indian population. This study was, therefore, undertaken to compare the efficacy and tolerability of lanthanum carbonate with calcium acetate in patients with stage 4 chronic kidney disease. Departments of Pharmacology and DDesign:esign: A randomized open label two group cross-over study. Therapeutics, Government Medical MMaterialsaterials aandnd MMethods:ethods: Following Institutional Ethics Committee approval and valid College, Thiruvananthapuram, consent, patients with stage 4 chronic kidney disease were randomized to receive either 1 Pharmacology, Government lanthanum carbonate 500 mg thrice daily or calcium acetate 667 mg thrice daily for Medical College, Kottayam, 4 weeks. After a 4-week washout period, the patients were crossed over for another 2Nephrology, Government Medical College, Thiruvananthapuram, 4 weeks. Serum phosphorous, serum calcium, serum alkaline phosphatase, and serum Kerala, India creatinine were estimated at fixed intervals. RResults:esults: Twenty-six patients were enrolled in the study. The mean serum phosphorous RReceived:eceived: 28.03.2008 concentrations showed a declining trend with lanthanum carbonate (from pre-drug levels of RRevised:evised: 12.07.2008 7.88 ± 1.52 mg/dL-7.14 ± 1.51 mg/dL) and calcium acetate (from pre-drug levels of 7.54 ± AAccepted:ccepted: 11.07.2009 1.39 mg/dL-6.51 ± 1.38 mg/dL). A statistically significant difference was seen when comparing the change in serum calcium produced by these drugs (P < 0.05). -

Fosrenol-Pm-En.Pdf
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION FOSRENOL® lanthanum carbonate hydrate Chewable tablets, 250 mg, 500 mg, 750 mg, and 1000 mg, oral Phosphate binder ATC code: V03A E03 Takeda Canada Inc. Date of Initial Approval: 22 Adelaide Street West, December 14, 2012 Suite 3800 Toronto Ontario M5H 4E3 Date of Revision: January 5, 2021 Submission Control No: 242595 FOSRENOL® and the FOSRENOL Logo are registered trademarks of Shire International Licensing BV, a Takeda company. Takeda® and the Takeda Logo are trademarks of Takeda Pharmaceutical Company Limited, used under license. FOSRENOL® Product Monograph Page 1 of 31 RECENT MAJOR LABEL CHANGES Not applicable TABLE OF CONTENTS RECENT MAJOR LABEL CHANGES ............................................................................ 2 TABLE OF CONTENTS .................................................................................................. 2 PART I: HEALTH PROFESSIONAL INFORMATION .................................................... 4 1 INDICATIONS ...................................................................................................... 4 1.1 Pediatrics ..................................................................................................... 4 1.2 Geriatrics ..................................................................................................... 4 2 CONTRAINDICATIONS ....................................................................................... 4 DOSAGE AND ADMINISTRATION .................................................................... -

Laaketilasto07 2.Pdf
Keskeisiä lukuja lääkkeiden myynnistä ja lääkekorvauksista vuonna 2007 Muutos vuodesta 2006 Lääkkeiden kokonaismyynti 2 500 milj. € 5,9 % avohoidon reseptilääkkeiden myynti (verollisin vähittäismyyntihinnoin) 1 817 milj. € 4,2 % avohoidon itsehoitolääkkeiden myynti (verollisin vähittäismyyntihinnoin) 275 milj. € 15,5 % sairaalamyynti (tukkuohjehinnoin) 408 milj. € 7,5 % Lääkkeistä maksetut korvaukset 1 142 milj. € 3,8 % peruskorvaukset 369 milj. € 0,6 % erityiskorvaukset 662 milj. € 6,8 % lisäkorvaukset 111 milj. € -2,3 % Key figures for medicine sales and their reimbursement in 2007 Change from 2006 Total sales of pharmaceuticals EUR 2,500 million 5.9% prescription medicines in outpatient care (at pharmacy prices with VAT) EUR 1,817 million 4.2% OTC medicines in outpatient care (at pharmacy prices with VAT) EUR 275 million 15.5% sales to hospitals (at wholesale prices) EUR 408 million 7.5% Reimbursement of medicine costs EUR 1,142 million 3.8% Basic Refunds EUR 369 million 0.6% Special Refunds EUR 662 million 6.8% Additional Refunds EUR 111 million -2.3% SUOMEN LÄÄKETILASTO FINNISH STATISTICS ON MEDICINES 2007 Lääkelaitos ja Kansaneläkelaitos National Agency for Medicines and Social Insurance Institution Helsinki 2008 LÄÄKELAITOS KANSANELÄKELAITOS NATIONAL AGENCY SOCIAL INSURANCE FOR MEDICINES INSTITUTION Lääketurvaosasto Tutkimusosasto Department of Safety Research Department and Drug Information Mannerheimintie 103b Nordenskiöldinkatu 12 P.O. Box 55 P.O. Box 450 FI-00301 Helsinki FI-00101 Helsinki Finland Finland Puh. (09) 473 341 Puh. 020 634 11 Tel. +358 9 473 341 Tel. +358 20 634 11 Telekopio (09) 473 34297 Telekopio 020 634 1700 Fax +358 9 473 34297 Fax +358 20 634 1700 ISSN 0786-2180 Kansi / Cover: Kari Piippo Edita Prima Oy Helsinki 2008 SISÄLLYS Kuvaluettelo ..................................................................................................................... -

Chronic Kidney Disease (CKD) in Dogs & Cats
Chronic Kidney Disease (CKD) in Dogs & Cats - Staging and Management Strategies Dennis J. Chew, DVM Diplomate ACVIM (Internal Medicine) The Ohio State University College of Veterinary Medicine Columbus, Ohio, USA Introduction Chronic kidney disease is diagnosed commonly in dogs and cats. The incidence of the diagnosis of CKD in cats is made 2 to 3 times as frequently compared to dogs and is especially common in geriatric cats. CKD is clinically characterized by the development of variably progressive irreversible intrarenal lesions and loss of renal functions. A variety of interventions (diet and drugs) can slow the progression of the renal disease, improve the quality of life for the patient, and/or extend the quantity of life. Compensatory increases (so called adaptations) in glomerular hemodynamics and glomerular volume may actually be maladaptive in some instances as shown in the figure below. The incidence of azotemic CKD was compared between dogs with and without periodontal disease in a recent epidemiological study. The hazard ratio for detection of azotemic CKD increased with the increasing severity of periodontal disease. Increasing severity of periodontal disease was also associated with serum creatinine >1.4 mg/dl and blood urea nitrogen >36 mg/dl whether or not the veterinarian diagnosed CKD (Glickman 2011). Figure 1. Concept of increased protein-trafficking as a consequence of intraglomerular hypertension and glomerular hypertrophy that occur in remnant nephrons associated with advanced CKD. Protein in urine is both a marker and a creator or more renal disease as shown in the graphic below. (From Canine and Feline Nephrology and Urology, 2nd edition –Chew DJ, DiBartola SP, Schenck PA, Elsevier Saunders, St. -

Sucroferric Oxyhydroxide 500Mg Chewable Tablets (Velphoro®) SMC No
sucroferric oxyhydroxide 500mg chewable tablets (Velphoro®) SMC No. (1035/15) Fresenius Medical Care (UK) Ltd. 6 March 2015 The Scottish Medicines Consortium (SMC) has completed its assessment of the above product and advises NHS Boards and Area Drug and Therapeutic Committees (ADTCs) on its use in NHS Scotland. The advice is summarised as follows: ADVICE: following a full submission sucroferric oxyhydroxide (Velphoro®) is accepted for use within NHS Scotland. Indication under review: For the control of serum phosphorus levels in adult chronic kidney disease (CKD) patients on haemodialysis (HD) or peritoneal dialysis (PD). It should be used within the context of a multiple therapeutic approach, which could include calcium supplement, 1,25-dihydroxy vitamin D3 or one of its analogues, or calcimimetics to control the development of renal bone disease. After 12 weeks, sucroferric oxyhydroxide was non-inferior to a non-calcium, non-aluminium- based phosphate binder at lowering serum phosphorus levels in adults with CKD, receiving HD or PD. Overleaf is the detailed advice on this product. Chairman, Scottish Medicines Consortium Published 13 April 2015 Indication For the control of serum phosphorus levels in adult chronic kidney disease (CKD) patients on haemodialysis (HD) or peritoneal dialysis (PD). It should be used within the context of a multiple therapeutic approach, which could include calcium supplement, 1,25-dihydroxy vitamin D3 or one of its analogues, or calcimimetics to control the development of renal bone disease. Dosing Information The recommended starting dose is 1,500mg iron (3 tablets) per day. Serum phosphorus levels must be monitored and the dose titrated up or down in increments of 500mg iron (1 tablet) per day every 2 to 4 weeks until an acceptable serum phosphorus level is reached, with regular monitoring afterwards. -

Effects of Lanthanum Carbonate on the Absorption and Oral Bioavailability of Ciprofloxacin
Effects of Lanthanum Carbonate on the Absorption and Oral Bioavailability of Ciprofloxacin Priscilla P. How,* James H. Fischer,* Jose A. Arruda,† and Alan H. Lau* Departments of *Pharmacy Practice and †Medicine (Section of Nephrology), University of Illinois at Chicago, Chicago, Illinois Background and objectives: Phosphate binders such as calcium salts or sevelamer, a cationic polymer, can markedly reduce absorption of oral ciprofloxacin. This randomized, open-label, two-way, crossover study examined the influence of the cation lanthanum on systemic ciprofloxacin exposure after oral administration. Design, setting, participants, & measurements: Twelve patients randomly received in a crossover manner a single oral dose of ciprofloxacin 750 mg alone and plus lanthanum carbonate 1 g three times daily with meals for six doses, with a washout interval of 7 to 14 d. Serial blood and urine samples were collected for 24 h after ciprofloxacin administration, and ciprofloxacin concentrations were determined using reverse-phase HPLC. Pharmacokinetic parameters of ciprofloxacin were calculated by noncompartmental methods, and the effect of lanthanum on ciprofloxacin pharmacokinetic parameters was assessed using ANOVA. Results: Lanthanum decreased (P < 0.001) the mean ciprofloxacin area under the plasma concentration–time curve by 54% and the maximum plasma concentration by 56%. The 24-h urinary recovery of ciprofloxacin was reduced by 52% by lanthanum (P < 0.001). No statistically significant differences in ciprofloxacin time to maximum plasma concentration, elimination half-life, and renal clearance occurred between the two arms. Conclusions: Lanthanum carbonate significantly reduces the systemic exposure to orally administered ciprofloxacin. Concomitant administration of both drugs should be avoided to prevent possible suboptimal response to ciprofloxacin. -

C:\Data\NDA 21468 Lanthanum Carbonate
NDA 21-468 Page 4 FOSRENOL (foss-wren-all) (Lanthanum Carbonate) 250 mg and 500 mg Chewable Tablets. DESCRIPTION FOSRENOL® contains lanthanum carbonate (2:3) hydrate with molecular formula La2(CO3)3 xH2O (on average x=4-5 moles of water) and molecular weight 457.8 (anhydrous mass). Lanthanum (La) is a naturally occurring rare earth element. Lanthanum carbonate is practically insoluble in water. Each FOSRENOL®, white to off-white, chewable tablet contains lanthanum carbonate hydrate equivalent to 250 or 500 mg of elemental lanthanum and the following inactive ingredients: dextrates (hydrated) NF, colloidal silicon dioxide NF, magnesium stearate NF, and talc USP. CLINICAL PHARMACOLOGY Patients with end stage renal disease (ESRD) can develop hyperphosphatemia that may be associated with secondary hyperparathyroidism and elevated calcium phosphate product. Elevated calcium phosphate product increases the risk of ectopic calcification. Treatment of hyperphosphatemia usually includes all of the following: reduction in dietary intake of phosphate, removal of phosphate by dialysis and inhibition of intestinal phosphate absorption with phosphate binders. FOSRENOL® does not contain calcium or aluminum. Pharmacodynamics: Lanthanum carbonate dissociates in the acid environment of the upper GI tract to release lanthanum ions that bind dietary phosphate released from food during digestion. FOSRENOL® inhibits absorption of phosphate by forming highly insoluble lanthanum phosphate complexes, consequently reducing both serum phosphate and calcium phosphate product. In vitro studies have shown that in the physiologically relevant pH range of 3 to 5 in gastric fluid, lanthanum binds approximately 97% of the available phosphate when lanthanum is present in a two-fold molar excess to phosphate. In order to bind dietary phosphate efficiently, lanthanum should be administered with or immediately after a meal. -

205739Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 205739Orig1s000 MEDICAL REVIEW(S) DIVISION OF CARDIO-RENAL DRUG PRODUCTS Divisional Memorandum NDA: 205739 (pati romer; Veltassa) Sponsor: Re lypsa Review date: 17 October 2015 Reviewer: N. Stockbridge, M.D., Ph.D., HFD-110 (b) (4) (b) Patiromer is a polymer(4) intended as a non-absorbable potassium bi nder. T he appli cation has been the subject of reviews of CMC/Biopharmaceutics by Drs. Frankewich, Sapru, Chikhale, Srinivasachar and others (28 July 2015; 15 October 2015), a pharmacology/toxicology review by Dr. Link (19 June 2015), clinical pharmacology reviews by Drs. Lai, Florian, and Madabushi (23 July 2015; 16 October 2015), clinical review by Dr. Xiao (19 June 2015), and statistical review by Dr. Kong (11 June 2015). There is a CDTL memo by Dr. Thompson (9 October 2015) with which I am in substantial agreement. I note a few selected issues here. At this writing, there are no ope n CMC issues. The drug product must be refrigerated to retard fluoride release, and then used wi thin 3 months of be i ng stored outside a refrigerator at room temperature (25°C ± 2°C [77°F ± 4°F]). However, the sponsor printed carton and container labels with instructions (b) (4) . CMC’s position (email of 15 October) is that the carton and container labels need to be consistent with the PI. I agree that the carton and container labels need to be made consistent, but I believe that this can reasonably be deferred until the next printing. I do not believe that storage under the conditions on the carton and container label is less safe (b) (4) Manufacturing inspe ctions were satisfactory. -

FOSRENOL (Lanthanum Carbonate)
HIGHLIGHTS OF PRESCRIBING INFORMATION --------------------WARNINGS AND PRECAUTIONS--------------------- These highlights do not include all the information needed to use • Serious cases of gastrointestinal obstruction, ileus, subileus, FOSRENOL safely and effectively. See full prescribing information for gastrointestinal perforation, and fecal impaction. Risks include altered FOSRENOL. gastrointestinal anatomy, hypomotility disorders, and concomitant medications. Advise patients to chew or crush the tablet completely. (5.1) FOSRENOL (lanthanum carbonate) chewable tablets, for oral use • FOSRENOL has radio-opaque properties and therefore may give the FOSRENOL (lanthanum carbonate) oral powder, for oral use appearance typical of an imaging agent during abdominal X-ray Initial U.S. Approval: 2004 procedures. (5.2) -------------------------RECENT MAJOR CHANGES------------------------- ---------------------------ADVERSE REACTIONS--------------------------- Warnings and Precautions (5.1) 11/2018 • In controlled trials, the most common adverse reactions that were more -------------------------INDICATIONS AND USAGE------------------------- frequent (> 5% difference vs. placebo) in FOSRENOL were nausea, • FOSRENOL is a phosphate binder indicated to reduce serum phosphate in vomiting and abdominal pain. (6.1) patients with end stage renal disease (ESRD). (1) • The following adverse reactions have been identified during post-approval use of FOSRENOL: constipation, dyspepsia, allergic skin reactions, and ---------------------DOSAGE AND ADMINISTRATION-------------------- tooth injury while chewing the tablet. (6.2) • The recommended initial total daily dose of FOSRENOL is 1500 mg in divided doses. Titrate every 2-3 weeks based on serum phosphate level. (2) To report SUSPECTED ADVERSE REACTIONS, contact Shire US Inc. • Take FOSRENOL with or immediately after meals. (2) at 1-800-828-2088 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch • FOSRENOL Chewable Tablets: Chew or crush tablet completely before swallowing. -
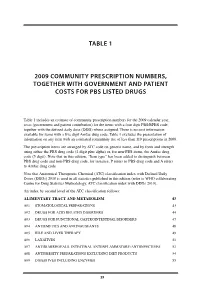
Table 1 2009 Community Prescription Numbers
TABLE 1 2009 COMMUNITY PRESCRIPTION NUMBERS, TOGETHER WITH GOVERNMENT AND PATIENT COSTS FOR PBS LISTED DRUGS Table 1 includes an estimate of community prescription numbers for the 2009 calendar year, costs (government and patient contribution) for the items with a four digit PBS/RPBS code, together with the defined daily dose (DDD) where assigned. There is no cost information available for items with a five digit Amfac drug code. Table 1 excludes the presentation of information on any item with an estimated community use of less than 110 prescriptions in 2009. The prescription items are arranged by ATC code on generic name, and by form and strength using either the PBS drug code (4 digit plus alpha) or, for non-PBS items, the Amfac drug code (5 digit). Note that in this edition, “Item type” has been added to distinguish between PBS drug code and non-PBS drug code, for instance, P refers to PBS drug code and A refers to Amfac drug code. Note that Anatomical Therapeutic Chemical (ATC) classification index with Defined Daily Doses (DDDs) 2010 is used in all statistics published in this edition (refer to WHO collaborating Centre for Drug Statistics Methodology, ATC classification index with DDDs 2010). An index by second level of the ATC classification follows: ALIMENTARY TRACT AND METABOLISM 43 A01 STOMATOLOGICAL PREPARATIONS 43 A02 DRUGS FOR ACID RELATED DISORDERS 44 A03 DRUGS FOR FUNCTIONAL GASTROINTESTINAL DISORDERS 47 A04 ANTIEMETICS AND ANTINAUSEANTS 48 A05 BILE AND LIVER THERAPY 49 A06 LAXATIVES 51 A07 ANTIDIARRHOEALS, INTESTINAL ANTIINFLAMMATORY/ANTIINFECTIVES -

Australian Public Assessment Report for Sodium Zirconium Cyclosilicate Hydrate
Australian Public Assessment Report for Sodium zirconium cyclosilicate hydrate Proprietary Product Name: Lokelma Sponsor: AstraZeneca Pty Ltd February 2018 Therapeutic Goods Administration About the Therapeutic Goods Administration (TGA) · The Therapeutic Goods Administration (TGA) is part of the Australian Government Department of Health and is responsible for regulating medicines and medical devices. · The TGA administers the Therapeutic Goods Act 1989 (the Act), applying a risk management approach designed to ensure therapeutic goods supplied in Australia meet acceptable standards of quality, safety and efficacy (performance) when necessary. · The work of the TGA is based on applying scientific and clinical expertise to decision- making, to ensure that the benefits to consumers outweigh any risks associated with the use of medicines and medical devices. · The TGA relies on the public, healthcare professionals and industry to report problems with medicines or medical devices. TGA investigates reports received by it to determine any necessary regulatory action. · To report a problem with a medicine or medical device, please see the information on the TGA website <https://www.tga.gov.au> About AusPARs · An Australian Public Assessment Report (AusPAR) provides information about the evaluation of a prescription medicine and the considerations that led the TGA to approve or not approve a prescription medicine submission. · AusPARs are prepared and published by the TGA. · An AusPAR is prepared for submissions that relate to new chemical entities, generic medicines, major variations and extensions of indications. · An AusPAR is a static document; it provides information that relates to a submission at a particular point in time. · A new AusPAR will be developed to reflect changes to indications and/or major variations to a prescription medicine subject to evaluation by the TGA.