Attachment: Extract from Clinical Evaluation Report Sodium
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
How to Take Your Phosphate Binders
How to take your phosphate binders Information for renal patients Oxford Kidney Unit Page 2 What are phosphate binders? To reduce the amount of phosphate you absorb from your food you may have been prescribed a medicine called a phosphate binder. Phosphate binders work by binding (attaching) to some of the phosphate in food. This will reduce the amount of phosphate being absorbed into your blood stream. A list of phosphate binders and how to take them is shown below. Phosphate binder How to take it Calcichew (calcium carbonate) Chew thoroughly 10-15 minutes before or immediately before food Renacet (calcium acetate) Phosex (calcium acetate) Osvaren (calcium acetate and magnesium carbonate) Swallow whole after the first Renagel 2-3 mouthfuls of food (sevelemer hydrochloride) Renvela tablets (sevelemer carbonate) Alucaps (aluminium hydroxide) Renvela powder Dissolve in 60ml of water and (sevelemer carbonate) take after the first 2-3 mouthfuls of food Fosrenol tablets Chew thoroughly towards the (lanthanum carbonate) end/immediately after each meal Fosrenol powder Mix with a small amount of (lanthanum carbonate) food and eat immediately Velphoro Chew thoroughly after the first (sucroferric oxyhydroxide) 2-3 mouthfuls The phosphate binder you have been prescribed is: ……………………………………………………………………………………………………………………………………………………….. Page 3 How many phosphate binders should I take? You should follow the dose that has been prescribed for you. Your renal dietitian can advise how best to match your phosphate binders to your meal pattern, as well as which snacks require a phosphate binder. What happens if I forget to take my phosphate binder? For best results, phosphate binders should be taken as instructed. -

Calcium Acetate Capsules
Calcium Acetate Capsules Type of Posting Revision Bulletin Posting Date 27–Dec–2019 Official Date 01–Jan–2020 Expert Committee Chemical Medicines Monographs 6 Reason for Revision Compliance In accordance with the Rules and Procedures of the 2015–2020 Council of Experts, the Chemical Medicines Monographs 6 Expert Committee has revised the Calcium Acetate Capsules monograph. The purpose for the revision is to add Dissolution Test 4 to accommodate FDA-approved drug products with different dissolution conditions and/or tolerances than the existing dissolution tests. • Dissolution Test 4 was validated using a YMC-Pack ODS-A C18 brand of L1 column. The typical retention time for calcium acetate is about 4.3 min. The Calcium Acetate Capsules Revision Bulletin supersedes the currently official monograph. Should you have any questions, please contact Michael Chang, Senior Scientific Liaison (301-230-3217 or [email protected]). C236679-M11403-CHM62015, rev. 00 20191227 Revision Bulletin Calcium 1 Official January 1, 2020 Calcium Acetate Capsules PERFORMANCE TESTS DEFINITION Change to read: Calcium Acetate Capsules contain NLT 90.0% and NMT · DISSOLUTION á711ñ 110.0% of the labeled amount of calcium acetate Test 1 (C4H6CaO4). Medium: Water; 900 mL IDENTIFICATION Apparatus 2: 50 rpm, with sinkers · A. The retention time of the calcium peak of the Sample Time: 10 min solution corresponds to that of the Standard solution, as Mobile phase, Standard solution, Chromatographic obtained in the Assay. system, and System suitability: Proceed as directed in · B. IDENTIFICATION TESTSÐGENERAL á191ñ, Chemical the Assay. Identification Tests, Acetate Sample solution: Pass a portion of the solution under test Sample solution: 67 mg/mL of calcium acetate from through a suitable filter of 0.45-µm pore size. -

Effect of Lanthanum Carbonate and Calcium Acetate in the Treatment of Hyperphosphatemia in Patients of Chronic Kidney Disease P
Research Article Effect of lanthanum carbonate and calcium acetate in the treatment of hyperphosphatemia in patients of chronic kidney disease P. Thomas Scaria, Reneega Gangadhar1, Ramdas Pisharody2 ABSTRACT OObjectives:bjectives: The tolerability and efficacy of lanthanum carbonate has not been studied in the Indian population. This study was, therefore, undertaken to compare the efficacy and tolerability of lanthanum carbonate with calcium acetate in patients with stage 4 chronic kidney disease. Departments of Pharmacology and DDesign:esign: A randomized open label two group cross-over study. Therapeutics, Government Medical MMaterialsaterials aandnd MMethods:ethods: Following Institutional Ethics Committee approval and valid College, Thiruvananthapuram, consent, patients with stage 4 chronic kidney disease were randomized to receive either 1 Pharmacology, Government lanthanum carbonate 500 mg thrice daily or calcium acetate 667 mg thrice daily for Medical College, Kottayam, 4 weeks. After a 4-week washout period, the patients were crossed over for another 2Nephrology, Government Medical College, Thiruvananthapuram, 4 weeks. Serum phosphorous, serum calcium, serum alkaline phosphatase, and serum Kerala, India creatinine were estimated at fixed intervals. RResults:esults: Twenty-six patients were enrolled in the study. The mean serum phosphorous RReceived:eceived: 28.03.2008 concentrations showed a declining trend with lanthanum carbonate (from pre-drug levels of RRevised:evised: 12.07.2008 7.88 ± 1.52 mg/dL-7.14 ± 1.51 mg/dL) and calcium acetate (from pre-drug levels of 7.54 ± AAccepted:ccepted: 11.07.2009 1.39 mg/dL-6.51 ± 1.38 mg/dL). A statistically significant difference was seen when comparing the change in serum calcium produced by these drugs (P < 0.05). -

Fosrenol-Pm-En.Pdf
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION FOSRENOL® lanthanum carbonate hydrate Chewable tablets, 250 mg, 500 mg, 750 mg, and 1000 mg, oral Phosphate binder ATC code: V03A E03 Takeda Canada Inc. Date of Initial Approval: 22 Adelaide Street West, December 14, 2012 Suite 3800 Toronto Ontario M5H 4E3 Date of Revision: January 5, 2021 Submission Control No: 242595 FOSRENOL® and the FOSRENOL Logo are registered trademarks of Shire International Licensing BV, a Takeda company. Takeda® and the Takeda Logo are trademarks of Takeda Pharmaceutical Company Limited, used under license. FOSRENOL® Product Monograph Page 1 of 31 RECENT MAJOR LABEL CHANGES Not applicable TABLE OF CONTENTS RECENT MAJOR LABEL CHANGES ............................................................................ 2 TABLE OF CONTENTS .................................................................................................. 2 PART I: HEALTH PROFESSIONAL INFORMATION .................................................... 4 1 INDICATIONS ...................................................................................................... 4 1.1 Pediatrics ..................................................................................................... 4 1.2 Geriatrics ..................................................................................................... 4 2 CONTRAINDICATIONS ....................................................................................... 4 DOSAGE AND ADMINISTRATION .................................................................... -

Production and Testing of Calcium Magnesium Acetate in Maine
77 Majesty's Stationery Office, London, England, River. Res. Note FPL-0229. Forest Service, U.S. 1948. Department of Agriculture, Madison, Wis., 1974. 14. M.S. Aggour and A. Ragab. Safety and Soundness 20. W.L. James. Effect of Temperature and Moisture of Submerged Timber Bridge PU.ing. FHWA/MD In Content on Internal Friction and Speed of Sound terim Report AW082-231-046. FHWA, U.S. Depart in Douglas Fir. Forest Product Journal, Vol. ment of Transportation, June 1982. 11, No. 9, 1961, pp. 383-390, 15. B.O. Orogbemi. Equipment for Determining the 21. A, Burmester. Relationship Between Sound Veloc Dynami c Modulus of Submerged Bridge Timber Pil ity and Morphological, Physical, and Mechani ·ing. Master's thesis. University of Maryland, cal Properties of Wood. Holz als Roh und Wer College Park, 1980. stoff, Vol. 23, No. 6, 1965, pp. 227-236 (in 16. T.L. Wilkinson. Strength Evaluation of Round German) • Timber Piles. Res. Note FPL-101. Forest Ser 22. c.c. Gerhards. Stress Wave Speed and MOE of vice, U.S. Department of Agriculture, Madison, Weetgum Ranging from 150 to 15 Percent MC. Wis., 1968. Forest Product Journal, Vol. 25, No. 4, 1975, 17. J, Bodig and B.A. Jayne. Mechanics of Wood and pp. 51-57. Wood Composites. Van Nostrand, New York, 1982. 18. R.M. Armstrong. Structural Properties of Timber Piles, Behavior of Deep Foundations. Report STP-670, ASTM, Philadelphia, 1979, pp. 118-152. 19. B.A, Bendtsen. Bending Strength and Stiffness Publication of this paper sponsored by Committee on of Bridge Piles After 85 Years in the Milwaukee Structures Maintenance. -
Phosphate Binders
Pharmacy Info Sheet Phosphate Binders calcium acetate, calcium carbonate (Tums, Calsan, Apocal, Ocal), calcium liquid, aluminum hydroxide (Basaljel, Amphojel), sevelamer (Renagel), lanthanum (Fosrenol) What it does: Phosphate binders are used to treat high Special considerations for lanthamum and blood phosphorus levels. sevelamer: Calcium acetate, calcium carbonate, calcium Lanthanum should be taken during or liquid, aluminum hydroxide, lanthanum and immediately after a meal. Taking a dose on an sevelamer bind dietary phosphate. When the empty stomach can cause nausea and kidneys fail, phosphorus builds up in the body vomiting. Chew the tablet completely before because the kidneys can no longer remove swallowing. DO NOT swallow tablets whole. much phosphorus. Phosphate binders are used to lower the amount of phosphorus Sevelamer should be taken just before eating. absorbed from food to limit development of Swallow the tablet whole – Renagel should not bone and blood vessel disease. be cut or chewed. The contents of sevelamer tablets expand in water and could cause Aluminum hydroxide and calcium carbonate choking if cut chewed or crushed. may also be prescribed as antacids. Calcium preparations may also be prescribed as Phosphate binders may interfere with the calcium supplements. Use them only as absorption of certain drugs such as iron prescribed. When these medications are supplements, antibiotics, digoxin, ranitidine, prescribed as calcium supplements or antiseizure, and antiarrhythmic medications. antacids, take between meals. If you are prescribed any of these drugs, take them at least 1 hour before or 3 hours after your How it works: phosphate binder. Kidney disease can cause phosphate to accumulate which results in bone and blood What to do if you miss a dose: vessel disease. -
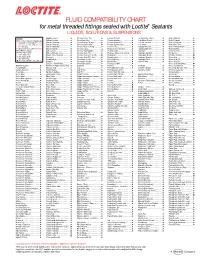
FLUID COMPATIBILITY CHART for Metal Threaded Fittings Sealed with Loctite¨ Sealants LIQUIDS, SOLUTIONS & SUSPENSIONS
FLUID COMPATIBILITY CHART for metal threaded fittings sealed with Loctite® Sealants LIQUIDS, SOLUTIONS & SUSPENSIONS LEGEND: Bagasse Fibers.......................... Chlorobenzene Dry ................... Ferrous Chloride ...................... Ion Exclusion Glycol ................. Nickel Chloride.......................... All Loctite® Anaerobic Sealants are Barium Acetate ........................ Chloroform Dry......................... Ferrous Oxalate......................... Irish Moss Slurry...................... Nickel Cyanide ......................... Compatible Including #242®, 243, Barium Carbonate..................... Chloroformate Methyl............... Ferrous Sulfate10%.................. Iron Ore Taconite ..................... Nickel Fluoborate ..................... 542, 545, 565, 567, 569, 571, 572, Barium Chloride........................ Chlorosulfonic Acid .................. Ferrous Sulfate (Sat)................. Iron Oxide ................................ Nickel Ore Fines ....................... 577, 580, 592 Barium Hydroxide..................... Chrome Acid Cleaning .............. Fertilizer Sol ............................. Isobutyl Alcohol ....................... Nickel Plating Bright ................. † Use Loctite® #270, 271™, 277, 554 Barium Sulfate.......................... Chrome Liquor.......................... Flotation Concentrates.............. Isobutyraldehyde ..................... Nickel Sulfate ........................... Not Recommended Battery Acid .............................. Chrome Plating -

Production of Low-Cost Acetate Deicers from Biomass and Industrial Wastes
Production of Low-Cost Acetate Deicers from Biomass and Industrial Wastes Shang-Tian Yang and Zuwei Jin, The Ohio State University Brian H. ChoUar, Federal Highway Administration Calcium magnesium acetate (CMA), a mixture of calcium 1 rom 10 million to 14 million tons of road salt are acetate and magnesium acetate, is used as an environmen• I used annually in the United States and Canada. tally benign roadway deicer. The present commercial F Salt is an extremely effective snow and ice con• CMA deicer made from glacial acetic acid and dolomitic trol agent and is relatively inexpensive. However, a lime or limestone is more expensive than salt and other study in New York State showed that although 1 ton of deicers. Also, a liquid potassium acetate deicer is used to road salt cost only $25, it caused more than $1,400 in replace urea and glycol in airport runway deicing. Two al• damage (1). Salt is corrosive to concrete and metals ternative low-cost methods to produce these acetate de- used in the nation's infrastructure, is harmful to road• icers from cheap feedstocks, such as biomass and side vegetation, and poses serious threats to environ• industrial wastes, were studied. CMA deicers produced ment and ground-water quality in some regions (2). from cheese whey by fermentation and extraction were FHWA spends about $12.5 billion annually, a sub• tested for their acetate content and deicing property. The stantial portion of which is used to rebuild and resur• CMA solid sample obtained from extraction of the acetic face highways and bridges damaged by salt corrosion. -

BLUE BOOK 1 Methyl Acetate CIR EXPERT PANEL MEETING
BLUE BOOK 1 Methyl Acetate CIR EXPERT PANEL MEETING AUGUST 30-31, 2010 Memorandum To: CIR Expert Panel Members and Liaisons From: Bart Heldreth Ph.D., Chemist Date: July 30, 2010 Subject: Draft Final Report of Methyl Acetate, Simple Alkyl Acetate Esters, Acetic Acid and its Salts as used in Cosmetics . This review includes Methyl Acetate and the following acetate esters, relevant metabolites and acetate salts: Propyl Acetate, Isopropyl Acetate, t-Butyl Acetate, Isobutyl Acetate, Butoxyethyl Acetate, Nonyl Acetate, Myristyl Acetate, Cetyl Acetate, Stearyl Acetate, Isostearyl Acetate, Acetic Acid, Sodium Acetate, Potassium Acetate, Magnesium Acetate, Calcium Acetate, Zinc Acetate, Propyl Alcohol, and Isopropyl Alcohol. At the June 2010 meeting, the Panel reviewed information submitted in response to an insufficient data announcement for HRIPT data for Cetyl Acetate at the highest concentration of use (lipstick). On reviewing the data in the report, evaluating the newly available unpublished studies and assessing the newly added ingredients, the Panel determined that the data are now sufficient, and issued a Tentative Report, with a safe as used conclusion. Included in this report are Research Institute for Fragrance Materials (RIFM) sponsored toxicity studies on Methyl Acetate and Propyl Acetate, which were provided in “wave 2” at the June Panel Meeting but are now incorporated in full. The Tentative Report was issued for a 60 day comment period (60 days as of the August panel meeting start date). The Panel should now review the Draft Final Report, confirm the conclusion of safe, and issue a Final Report. All of the materials are in the Panel book as well as in the URL for this meeting's web page http://www.cir- safety.org/aug10.shtml. -

Laaketilasto07 2.Pdf
Keskeisiä lukuja lääkkeiden myynnistä ja lääkekorvauksista vuonna 2007 Muutos vuodesta 2006 Lääkkeiden kokonaismyynti 2 500 milj. € 5,9 % avohoidon reseptilääkkeiden myynti (verollisin vähittäismyyntihinnoin) 1 817 milj. € 4,2 % avohoidon itsehoitolääkkeiden myynti (verollisin vähittäismyyntihinnoin) 275 milj. € 15,5 % sairaalamyynti (tukkuohjehinnoin) 408 milj. € 7,5 % Lääkkeistä maksetut korvaukset 1 142 milj. € 3,8 % peruskorvaukset 369 milj. € 0,6 % erityiskorvaukset 662 milj. € 6,8 % lisäkorvaukset 111 milj. € -2,3 % Key figures for medicine sales and their reimbursement in 2007 Change from 2006 Total sales of pharmaceuticals EUR 2,500 million 5.9% prescription medicines in outpatient care (at pharmacy prices with VAT) EUR 1,817 million 4.2% OTC medicines in outpatient care (at pharmacy prices with VAT) EUR 275 million 15.5% sales to hospitals (at wholesale prices) EUR 408 million 7.5% Reimbursement of medicine costs EUR 1,142 million 3.8% Basic Refunds EUR 369 million 0.6% Special Refunds EUR 662 million 6.8% Additional Refunds EUR 111 million -2.3% SUOMEN LÄÄKETILASTO FINNISH STATISTICS ON MEDICINES 2007 Lääkelaitos ja Kansaneläkelaitos National Agency for Medicines and Social Insurance Institution Helsinki 2008 LÄÄKELAITOS KANSANELÄKELAITOS NATIONAL AGENCY SOCIAL INSURANCE FOR MEDICINES INSTITUTION Lääketurvaosasto Tutkimusosasto Department of Safety Research Department and Drug Information Mannerheimintie 103b Nordenskiöldinkatu 12 P.O. Box 55 P.O. Box 450 FI-00301 Helsinki FI-00101 Helsinki Finland Finland Puh. (09) 473 341 Puh. 020 634 11 Tel. +358 9 473 341 Tel. +358 20 634 11 Telekopio (09) 473 34297 Telekopio 020 634 1700 Fax +358 9 473 34297 Fax +358 20 634 1700 ISSN 0786-2180 Kansi / Cover: Kari Piippo Edita Prima Oy Helsinki 2008 SISÄLLYS Kuvaluettelo ..................................................................................................................... -

Chronic Kidney Disease (CKD) in Dogs & Cats
Chronic Kidney Disease (CKD) in Dogs & Cats - Staging and Management Strategies Dennis J. Chew, DVM Diplomate ACVIM (Internal Medicine) The Ohio State University College of Veterinary Medicine Columbus, Ohio, USA Introduction Chronic kidney disease is diagnosed commonly in dogs and cats. The incidence of the diagnosis of CKD in cats is made 2 to 3 times as frequently compared to dogs and is especially common in geriatric cats. CKD is clinically characterized by the development of variably progressive irreversible intrarenal lesions and loss of renal functions. A variety of interventions (diet and drugs) can slow the progression of the renal disease, improve the quality of life for the patient, and/or extend the quantity of life. Compensatory increases (so called adaptations) in glomerular hemodynamics and glomerular volume may actually be maladaptive in some instances as shown in the figure below. The incidence of azotemic CKD was compared between dogs with and without periodontal disease in a recent epidemiological study. The hazard ratio for detection of azotemic CKD increased with the increasing severity of periodontal disease. Increasing severity of periodontal disease was also associated with serum creatinine >1.4 mg/dl and blood urea nitrogen >36 mg/dl whether or not the veterinarian diagnosed CKD (Glickman 2011). Figure 1. Concept of increased protein-trafficking as a consequence of intraglomerular hypertension and glomerular hypertrophy that occur in remnant nephrons associated with advanced CKD. Protein in urine is both a marker and a creator or more renal disease as shown in the graphic below. (From Canine and Feline Nephrology and Urology, 2nd edition –Chew DJ, DiBartola SP, Schenck PA, Elsevier Saunders, St. -

Sucroferric Oxyhydroxide 500Mg Chewable Tablets (Velphoro®) SMC No
sucroferric oxyhydroxide 500mg chewable tablets (Velphoro®) SMC No. (1035/15) Fresenius Medical Care (UK) Ltd. 6 March 2015 The Scottish Medicines Consortium (SMC) has completed its assessment of the above product and advises NHS Boards and Area Drug and Therapeutic Committees (ADTCs) on its use in NHS Scotland. The advice is summarised as follows: ADVICE: following a full submission sucroferric oxyhydroxide (Velphoro®) is accepted for use within NHS Scotland. Indication under review: For the control of serum phosphorus levels in adult chronic kidney disease (CKD) patients on haemodialysis (HD) or peritoneal dialysis (PD). It should be used within the context of a multiple therapeutic approach, which could include calcium supplement, 1,25-dihydroxy vitamin D3 or one of its analogues, or calcimimetics to control the development of renal bone disease. After 12 weeks, sucroferric oxyhydroxide was non-inferior to a non-calcium, non-aluminium- based phosphate binder at lowering serum phosphorus levels in adults with CKD, receiving HD or PD. Overleaf is the detailed advice on this product. Chairman, Scottish Medicines Consortium Published 13 April 2015 Indication For the control of serum phosphorus levels in adult chronic kidney disease (CKD) patients on haemodialysis (HD) or peritoneal dialysis (PD). It should be used within the context of a multiple therapeutic approach, which could include calcium supplement, 1,25-dihydroxy vitamin D3 or one of its analogues, or calcimimetics to control the development of renal bone disease. Dosing Information The recommended starting dose is 1,500mg iron (3 tablets) per day. Serum phosphorus levels must be monitored and the dose titrated up or down in increments of 500mg iron (1 tablet) per day every 2 to 4 weeks until an acceptable serum phosphorus level is reached, with regular monitoring afterwards.