Incidence Rate of Adjacent-Segment Disorder After Oblique Lateral Interbody Fusion at More Than Two Levels: Data from the Chiba Spine Surgery Registry Database
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Official Guide T2 All En.Pdf
2020 , 1 December 2020 FLOOR GUIDE ENGLISH December Narita International Airport Terminal2 Narita Airport is working in conjunction with organizations such as Japan’s Ministry of Narita International Airport FLOOR GUIDE, Planned and Published by Narita International Airport Corporation (NAA), Published Planned andPublished by Narita International FLOOR GUIDE, Airport Narita International Justice and Ministry of Health, Labour and Welfare to combat the spread of COVID-19. Due to the spread of the virus, business hours may have changed at some terminal facilities and stores. For the latest information, please consult the Narita International Airport Official Website. Narita International Airport Ofcial Website 英語 CONTENTS INFORMATION & SERVICES Lost Item Inquiries/infotouch Interactive Digital Displays NariNAVI/Lounges …………………………………………………………4 Flight Information/ Terminals and Airlines ……………………………………… 5 Internet Services ……………………………………………………………5 General Information ………………………………………………………5 FLOOR MAP Terminal 2 Services Map ……………………………………… 6–7 B1F Railways (Airport Terminal2 Station) ……………………………………………… 8–9 1F International Arrival Lobby …………………………………………… 10–11 2F Parking Lot Accessway ……………………………………………… 12–13 3F International Departure Lobby (Check-in Counter) ………………… 14–15 4F Restaurants and Shops/Observation Deck ……………………… 16–17 3F International Departure Lobby (Boarding Gate)/ Duty Free and Shopping Area ……………………………………… 18–21 Domestic Flights …………………………………………………… 22–23 SHOPS AND FACILITIES Before Passport Control … 24–29 After Domestic Check-in -

Entrance Ceremony Held to Welcome Newest Students by JIU Times
Produced by × JIU TIMES Vol. 16 SPRING 2016 Entrance ceremony held to welcome newest students by JIU Times Josai International University (JIU) held an entrance ceremony for new students on April 2 at its Togane Campus in Chiba Prefecture. The university, which is celebrating the 25th year anniversary, welcomed 1,650 students to its eight faculties and graduate school, as well as its school of Japanese Language and Culture. Among freshmen, 330 were non-Japanese from 22 countries and regions in Asia, Europe and South America. The ceremony at the Sports Culture Center was attended by foreign dignitaries, including HRH Tuanku Syed Faizuddin Putra Ibni Tu- anku Syed Sirajuddin Jamalullail, the Crown Prince of Perlis, Malaysia; HRH Tuanku Haj- jah Lailatul Shahreen Akashah Binti Khalil, Right photo: The Crown Prince of Perlis, Malaysia, HRH Tuanku Syed Faizuddin Putra Ibni Tuanku Syed Sirajuddin Jamalullail, one of the guests at the JIU entrance ceremony, addresses new students at the Togane the Crown Princess of Perlis, Malaysia; former Campus in Chiba Prefecture on April 2; Left photo: The Crown Prince and Crown Princess of Perlis, Malaysia, HRH Tuanku Hajjah Lailatul Shahreen Akashah Binti Khalil, look on during the ceremony. Malaysian Minister of Tourism and Josai Cen- tre of ASEAN Studies Director Ng Yen Yen; Foundation that enabled five female students Bright future ahead for latest graduates of JIU Kamarudin Hussin, former vice chancellor of from the Southeast Asian country to study at Universiti Malaysia Perlis (UniMAP); and Zul the university from the 2016 academic year. by Terutada Tsunoda, Student Her Imperial Highness Princess Taka- Azhar Zahid Jamal, deputy vice chancellor of “Created by the mother of his royal high- Faculty of International Humanities mado attended the ceremony, offering a UniMAP. -

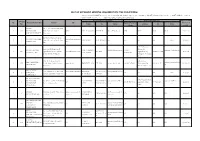
Summary of Family Membership and Gender by Club MBR0018 As of June, 2009
Summary of Family Membership and Gender by Club MBR0018 as of June, 2009 Club Fam. Unit Fam. Unit Club Ttl. Club Ttl. District Number Club Name HH's 1/2 Dues Females Male TOTAL District 333 C 25243 ABIKO 5 5 6 7 13 District 333 C 25249 ASAHI 0 0 2 75 77 District 333 C 25254 BOSHUASAI L C 0 0 3 11 14 District 333 C 25257 CHIBA 9 8 9 51 60 District 333 C 25258 CHIBA CHUO 3 3 4 21 25 District 333 C 25259 CHIBA ECHO 0 0 2 24 26 District 333 C 25260 CHIBA KEIYO 0 0 1 19 20 District 333 C 25261 CHOSHI 2 2 1 45 46 District 333 C 25266 FUNABASHI 4 4 5 27 32 District 333 C 25267 FUNABASHI CHUO 5 5 8 56 64 District 333 C 25268 FUNABASHI HIGASHI 0 0 0 23 23 District 333 C 25269 FUTTSU 1 0 1 21 22 District 333 C 25276 ICHIKAWA 0 0 2 36 38 District 333 C 25277 ICHIHARA MINAMI 1 1 0 33 33 District 333 C 25278 ICHIKAWA HIGASHI 0 0 2 14 16 District 333 C 25279 IIOKA 0 0 0 36 36 District 333 C 25282 ICHIHARA 9 9 7 26 33 District 333 C 25292 KAMAGAYA 12 12 13 31 44 District 333 C 25297 KAMOGAWA 0 0 0 37 37 District 333 C 25299 KASHIWA 0 0 4 41 45 District 333 C 25302 BOSO KATSUURA L C 0 0 3 54 57 District 333 C 25303 KOZAKI 0 0 2 25 27 District 333 C 25307 KAZUSA 0 0 1 45 46 District 333 C 25308 KAZUSA ICHINOMIYA L C 0 0 1 26 27 District 333 C 25309 KIMITSU CHUO 0 0 1 18 19 District 333 C 25310 KIMITSU 5 5 14 42 56 District 333 C 25311 KISARAZU CHUO 1 1 5 14 19 District 333 C 25314 KISARAZU 0 0 1 14 15 District 333 C 25316 KISARAZU KINREI 3 3 5 11 16 District 333 C 25330 MATSUDO 0 0 0 27 27 District 333 C 25331 SOBU CHUO L C 0 0 0 39 39 District 333 C -
List of Approved Sending Organization (The Philippines)
LIST OF APPROVED SENDING ORGANIZATION (THE PHILIPPINES) ※フィリピンの認定送出機関については,フィリピン海外雇用庁(POEA)が運営する以下のURLにて,送出機関の名称を入力することにより,同機関の連絡先やライセンス の取得状況等を検索できます。 http://www.poea.gov.ph/cgi-bin/agSearch.asp Person in charge of Training Contact Point in Japan Approved date OTIT List No. Name of Organization Address URL Name of Person in (the date of No. Name TEL Email Address TEL Email Charge receipt) AC SICAT Blk. 5 Lot 9 Villa Lourdes Subd. 1 306 INTERNATIONAL Brgy. San Isidro Bacolor NONE ARTURO C. SICAT 9661748085 [email protected] NONE NONE NONE NONE 2020/1/15 MANPOWER SERVICES Pampanga 6/F Metro Lifestyle Complex, F. A. KANAN MANPOWER www.akananmanpower. 2 2 Torres St., cor. Jacinto St., Davao HISANO HORI (053) 482-8451 N/A N/A N/A N/A N/A 2018/6/1 CORPORATION com City 2-24-22, Bunkyo, Suite 501 AP Bldg. 1563 F. Minami-ku, AB INTERNATIONAL ELIAS FERNANDO [email protected] OLIVIA S. [email protected] 3 287 Agoncillo St. corner Pedro Gil www.abmanpower.com 523-6268 Sagamihara City +8142-701-0538 2019/7/4 PLACEMENT INC R. SALVADOR m KAWAGUCHI m Ermita, Manila, Philippines Kanagawa Pref. 252- 0307 11th Flr. Goldloop Tower A, Saitama Ken ABBA PERSONNEL [email protected] 4 155 Escriva Drive, Ortigas Center, www.abba.ph JENEVIEVE P. ORA 637-1324 [email protected] LALAINE KENDO Tokorozawa City 042-941-4152 2019/1/23 SERVICES INC. .jp Pasig City Matsuba Cho 20-23 ABD OVERSEAS 23 10 Marconi St. corner Morse www.abdrecruitment.co ANANIAS B. 843-4757 / 0917- [email protected] 5 8 MANPOWER N/A N/A N/A N/A 2018/6/1 St. -
![Growth Strategy for "Sustainable Management" [PDF:993KB]](https://docslib.b-cdn.net/cover/7571/growth-strategy-for-sustainable-management-pdf-993kb-1047571.webp)
Growth Strategy for "Sustainable Management" [PDF:993KB]
Growth Strategy for “Sustainable Management” Medium Term Management Plan The 13th Medium Term Management Plan Best Bank 2020 Final stage-3 years of value co-creation From April 1, 2017 to March 31, 2020 This medium term management plan is for the final stage (three years) to accomplish our ultimate goal - to become the “best retail” banking group - by the target year of 2020 as set by the previous medium Our vision term management plan and to create the foundations for responding to environmental changes expected to occur over the medium to long term. We will bolster productivity and solidify customer confidence, and realize sustainable growth, by co-creating value (value co-creation) with our stakeholders, such as customers, shareholders, employees, and regional communities, etc. We aim to become the “best retail” banking group that provides top-class customer satisfaction through advanced services, and to be highly regarded by our regional customers, both individuals and SMEs. CS (Customer Satisfaction) ES (Employee Satisfaction) SS (Social Satisfaction) Ensure the “Customer Make a work environment Drive regional first policy” and respond where all employees can development, by speedily to customers’ realize their potential gathering the entire needs by providing with enthusiasm through Chiba Bank Group as the advanced services and diversity and work style leading bank in the area. solutions. reform. Key Issues Co-creating Realizing work style Strengthening 1 customer value 2 reforms that allow all 3 a sustainable employees to shine -

Local Cuisines, Japanese Sake) That Has Been Nurtured by the Rich Nature of the Region: the Case of the Coastal Area in Chiba Prefecture, Japan
Food and Nutrition Sciences, 2013, 4, 964-971 http://dx.dor.org/10.4236/fns.2013.49125 Published Online September 2013 (http://www.scirp.org/journal/fns) Traditional Food Culture (Local Cuisines, Japanese Sake) That Has Been Nurtured by the Rich Nature of the Region: The Case of the Coastal Area in Chiba Prefecture, Japan Korehisa Kaneko1*, Keiko Oshida2, Hajime Matsushima3 1Hokuso Creature Association, Tokyo, Japan; 2Department of Town Planning and Design, College of Science and Technology, Ni- hon University, Chiba, Japan; 3Research Faculty of Agriculture, Hokkaido University, Sapporo, Japan. Email: *[email protected] Received June 8th, 2013; revised July 8th, 2013; accepted July 15th, 2013 Copyright © 2013 Korehisa Kaneko et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT In Chiba Prefecture, Japan, during the Edo period (1603-1867), the development of waterway traffic by ships and the management of ports, highways and post towns around the ports progressed with the prosperity of the Edo (present-day Tokyo), which became heavily populated and the center of politics. We estimated that the demand of Japanese sake, which is luxury grocery item, was high. The freshwater layer that is abundant in mineral water to a depth of approxi- mately 10 m is formed in coastal sand dunes. The fresh water layer is hard water, in which the concentrations of miner- als such as calcium and magnesium are high. When the fresh water layer is used as the preparation water, the working rice malt and yeast in the sake brewing process become active. -

1,500 New Students Begin Journey by JIU Times
Produced by × Vol. 23 SPRING 2018 1,500 new students begin journey by JIU Times Josai International University welcomed about 1,500 new stu- dents, including foreign people from 18 countries, in a matricula- tion ceremony at its Togane Cam- pus in Chiba Prefecture, on April 2. JIU, a comprehensive university with eight faculties and 10 depart- ments, focuses on international education and is engaged in ex- change programs with many uni- versities and schools in Asia, Eu- rope, particularly Eastern Europe, pay attention to the world events and the Americas. Of its approxi- and news and participate actively mately 6,000 students, 1,438 were in local community activities to ex- non-Japanese from 24 countries perience practical learning.” last year. He also encouraged new Japa- In the matriculation ceremony, nese students to participate in ex- which took place at the Sports Cul- change programs with overseas ture Center, JIU President Kenji schools because studying different Sugibayashi greeted the new stu- cultures is a good experience. dents, as well as other students, Sugibayashi also stressed ad- teachers and special guests, in- vancement of high technology and cluding Togane Mayor Naoharu the importance of learning amid Shiga. the current global environment. “JIU has three campuses in To- “With globalization and rapid gane, Awa (Chiba Prefecture) and advancement of science and tech- Kioicho (Tokyo’s Chiyoda Ward). nology, existing things disappear changes and I believe people can dents, Josai University Educational ing, “What I will be tomorrow is We have undergraduate and grad- or become completely different make innovation happen by learn- Corporation Chancellor Akira Ue- the result of what I think and do uate programs, as well as senior things. -

Deep Two-Way Matrix Reordering for Relational Data Analysis
Deep Two-Way Matrix Reordering for Relational Data Analysis Chihiro Watanabe∗1 and Taiji Suzuki†1,2 1Graduate School of Information Science Technology, The University of Tokyo, Tokyo, Japan 2Center for Advanced Intelligence Project (AIP), RIKEN, Tokyo, Japan Abstract Matrix reordering is a task to permute the rows and columns of a given observed matrix such that the resulting reordered matrix shows meaningful or interpretable structural patterns. Most existing matrix reordering techniques share the common processes of extracting some feature representations from an observed matrix in a predefined manner, and applying matrix reordering based on it. However, in some practical cases, we do not always have prior knowledge about the structural pattern of an observed matrix. To address this problem, we propose a new matrix reordering method, called deep two-way matrix reordering (DeepTMR), using a neural network model. The trained network can automatically extract nonlinear row/column features from an observed matrix, which can then be used for matrix reordering. Moreover, the proposed DeepTMR provides the denoised mean matrix of a given observed matrix as an output of the trained network. This denoised mean matrix can be used to visualize the global structure of the reordered observed matrix. We demonstrate the effectiveness of the proposed DeepTMR by applying it to both synthetic and practical datasets. Keywords: matrix reordering, relational data analysis, neural network, visualization 1 Introduction Matrix reordering or seriation is a task to permute the rows and columns of a given observed ma- trix such that the resulting matrix shows meaningful or interpretable structural patterns [4, 22]. Such reordering-based matrix visualization techniques provide an overview of the various practical data ma- trices, including gene expression data [8, 12], document-term relationship data [5], and archaeological data [18] (e.g., the relationships between tombs and objects in Egypt [26]). -

Inba Clinical Pathway for Local Stroke Network with Helicopter Emergency Medical Service in Chiba, Japan
Research and Reviews Inba Clinical Pathway for Local Stroke Network with Helicopter Emergency Medical Service in Chiba, Japan JMAJ 54(1): 16–21, 2011 Masahiro MISHINA,*1 Hisashi MATSUMOTO*2 Abstract Many parties and various professions are involved in stroke Tokyo care, including citizens making prompt calls for ambulance, ambulance crews who transport patients appropriately, consolidation of patients and medical resources with a Ibaraki focus on stroke units, rehabilitation hospitals for reduction Prefecture of patients’ sequelae, primary care physicians who are in charge of managing risk factors to prevent the recurrence of disease, and long-term care services and care managers that support in-home care of patients. In Chiba Prefecture, the helicopter emergency medical service (HEMS, so-called “doctor helicopter” in Japan) was launched in October 500 km 2001, with Nippon Medical School Chiba Hokusoh Hospi- tal serving as the base hospital. Currently, the number of dispatches is ranked the highest in Japan. In March 2008, Chiba Prefecture, Japan 2 the Inba Clinical Pathway for local Stroke network (InCliPS) Population: 6.2 million Area: 5,157km [Source: Statistics Division, Policy and Planning Department, was launched to build a network of medical resources Chiba Prefecture (as of Sep 1, 2010)] beyond the boundaries of healthcare zones to utilize limited rehabilitation resources better. Then in February 2009, the liaison critical pathway for stroke designed for common use throughout Chiba Prefecture was established. Although these attempts are tools that merely link the sites of stroke onset to medical facilities of acute care, rehabilitation, and convalescent phages, we hope they help to halt healthcare collapse in Chiba by promoting the efficiency of medical services and prepare clinical practice system for the next generation. -

Chiba Travel
ChibaMeguri_sideB Leisure Shopping Nature History&Festival Tobu Noda Line Travel All Around Chiba ChibaExpressway Joban Travel Map MAP-H MAP-H Noda City Tateyama Family Park Narita Dream Farm MITSUI OUTLET PARK KISARAZU SHISUI PREMIUM OUTLET® MAP-15 MAP-24 Express Tsukuba Isumi Railway Naritasan Shinshoji Temple Noda-shi 18 MAP-1 MAP-2 Kashiwa IC 7 M22 Just within a stone’s throw from Tokyo by the Aqua Line, Nagareyama City Kozaki IC M24 Sawara Nagareyama IC Narita Line 25 Abiko Kozaki Town why don’t you visit and enjoy Chiba. Kashiwa 26 Sawara-katori IC Nagareyama M1 Abiko City Shimosa IC Whether it is for having fun, soak in our rich hot springs, RyutetsuNagareyamaline H 13 Kashiwa City Sakae Town Tobu Noda Line Minami Nagareyama Joban Line satiate your taste bud with superior products from the seas 6 F Narita City Taiei IC Tobu Toll Road Katori City Narita Line Shin-Matsudo Inzai City Taiei JCT Shiroi City Tonosho Town and mountains, Chiba New Town M20 Shin-Yahashira Tokyo Outer Ring Road Higashikanto Expressway Hokuso Line Shibayama Railway Matsudo City Inba-Nichi-idai Narita Sky Access Shin-Kamagaya 24 you can enjoy all in Chiba. Narita Narita Airport Tako Town Tone Kamome Ohashi Toll Road 28 34 Narita IC Musashino Line I Shibayama-Chiyoda Activities such as milking cows or making KamagayaShin Keisei City Line M2 All these conveniences can only be found in Chiba. Naritasan Shinshoji Temple is the main temple Narita International Airport Asahi City butter can be experienced on a daily basis. Narita Line Tomisato IC Ichikawa City Yachiyo City of the Shingon Sect of Chizan-ha Buddhism, Funabashi City Keisei-Sakura Shisui IC You can enjoy gathering poppy , gerbera, Additionally, there are various amusement DATA 398, Nakajima, Kisarazu-City DATA 689 Iizumi, Shisui-Town Sobu LineKeisei-Yawata Shibayama Town M21 Choshi City Isumi and Kominato railroad lines consecutively run across Boso Peninsula, through a historical Choshi 32 and antirrhinum all the year round in the TEL:0438-38-6100 TEL:043-481-6160 which was established in 940. -

Number/ Route Number Category Spots Telephone Adress Website
Number/ Route Category Spots Telephone Adress Website(Japanease) Website(English) Website(ภาษาไทย) Number A1 Scenery I-link Town Observation Deck 047-322-9300 1-10-1 Ichikawa-minami, Ichikawa - - - Chiba Museum of Science and http://www2.chiba- A2 Culture/Arts 047-379-2005 1-1-3 Onitaka, Ichikawa - - Industry muse.or.jp/SCIENCE/index.html A3 History Nakayama Hokekyo-ji Temple 047-334-3433 2-10-1 Nakayama, Ichikawa - - - 4-13-5 Nakayama, Ichikawa Nakayama-sando Shopping A4 Shopping (Nakayamasando Shopping Arcade), - - - Arcade/Wakaeikai Wakamiya 2-7-15, Ichikawa (Wakaeikai) Shopping arcade in the area around Funabashi and Keisei Funabashi Station A5 Shopping Kappo Ryokan Tamagawa - - - (Nakayama Shopping Arcade/Honcho-dori Shopping Arcade, others) A6 History, Cuisine, Onsen Kappo Ryokan Tamagawa 047-431-3234 2-6-25 Minatocho, Funabashi http://www.tamagawa-go.jp/ http://www.tamagawa-go.jp/en/ - A7 Cuisine Dairen 047-422-8952 4-20-17 Honcho, Funabashi - - - A8 Scenery Yatsu-higata tidal flat 047-454-8416 5-1-1 Akitsu, Narashino http://www.seibu-la.co.jp/yatsuhigata/ - - 1-106-16 Kemigawa-cho, A9 Cuisine Indian Cuisine Sitar 043-271-0581 http://www.sitar.co.jp/ - - Hanamigawa-ku, Chiba A10 Shopping Inage Shopping Arcade 070-2173-2458 3-6-2 Inage, Inage-ku, Chiba - - A11 History Inage-Sengen-jinja Shrine 043-245-7777 1-15-10 Inage, Inage-ku, Chiba http://www.inage-sengenjinja.or.jp/ - - A12 History Chiba-jinja Shrine 043-224-2211 1-16-1 Innai, Chuo-ku, Chiba https://www.chibajinja.com/ - - http://www.ccma- A13 Culture/Arts Chiba City Museum -

Chiba Don Quijote Funabashi Minamiguchi
02 HANEDA AIRPORT NARITA AIRPORT TOKYO 09 Flower viewing CHIBA JAPAN 05 10 06 spots and Mt.FUJI 08 CHIBA fruit picking farms 04 in Chiba 11 12 07 03 01 13 01 Mother Farm 02 Shimizu Park 03 Mobara Park Rape blossoms: late February-late March Cherry blossom: late March-early April Cherry blossom: late March-early April Approx. 3.5 million rape blossoms This is one of the most popular spots in Enjoy the breathtaking contrast carpeting the entire hillside are a Chiba for cherry blossom viewing. You between the red Bentendo Hall and the seasonal feature of Mother Farm! can enjoy about 50 different kinds of pink blossoms, and the romantic 940-3 Tagura, Futtsu cherry blossoms. atmosphere when light up at night. Approx. 30-40 minutes by direct bus from 906 Shimizu, Noda 1325-1 Takashi, Mobara Kimitsu Station South Exit (JR Uchibo Line) Approx. 10 minutes’ walk from Shimizu- Approx. 7 minutes by Kominato Bus (Feb.-Nov.) Weekdays 9:30-16:30 / kōen Station (Tobu Urban Park Line) from Mobara Station (JR Sotobo Line) Sat., Sun., national holiday 9:00-17:00 9:00-17:00 (Varies in winter) 24 hours (Dec.-Jan.) Weekdays 10:00-16:00 / Open 365 days Open 365 days Sat., Sun., national holiday 9:30-16:00 Several days in Dec. and Jan. 04 Sakura Castle Park 05 Naritasan Park 06 Sakura Furusato Square 07 Country Farm 08 Keisei Rose Garden Cherry blossom: late March-early April Cherry blossom: late March-early April Tulips: mid-late April Tokyo German Village Roses: May-June, October-November Official mascot“CHI-BA+KUN” The sight of the cherry blossoms at 350 someiyoshino and other varieties The Dutch windmill, the park’s symbol, Moss phlox: mid-late April Over 10,000 rose bushes bloom in the night (yozakura) from the neighboring of cherry trees blossom in this huge and the carpet of tulips make you feel huge 30,000 m2 garden.