A Novel Three–Dimensional Human Peritubular Microvascular System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urinary System
OUTLINE 27.1 General Structure and Functions of the Urinary System 818 27.2 Kidneys 820 27 27.2a Gross and Sectional Anatomy of the Kidney 820 27.2b Blood Supply to the Kidney 821 27.2c Nephrons 824 27.2d How Tubular Fluid Becomes Urine 828 27.2e Juxtaglomerular Apparatus 828 Urinary 27.2f Innervation of the Kidney 828 27.3 Urinary Tract 829 27.3a Ureters 829 27.3b Urinary Bladder 830 System 27.3c Urethra 833 27.4 Aging and the Urinary System 834 27.5 Development of the Urinary System 835 27.5a Kidney and Ureter Development 835 27.5b Urinary Bladder and Urethra Development 835 MODULE 13: URINARY SYSTEM mck78097_ch27_817-841.indd 817 2/25/11 2:24 PM 818 Chapter Twenty-Seven Urinary System n the course of carrying out their specific functions, the cells Besides removing waste products from the bloodstream, the uri- I of all body systems produce waste products, and these waste nary system performs many other functions, including the following: products end up in the bloodstream. In this case, the bloodstream is ■ Storage of urine. Urine is produced continuously, but analogous to a river that supplies drinking water to a nearby town. it would be quite inconvenient if we were constantly The river water may become polluted with sediment, animal waste, excreting urine. The urinary bladder is an expandable, and motorboat fuel—but the town has a water treatment plant that muscular sac that can store as much as 1 liter of urine. removes these waste products and makes the water safe to drink. -

The Urinary System Dr
The urinary System Dr. Ali Ebneshahidi Functions of the Urinary System • Excretion – removal of waste material from the blood plasma and the disposal of this waste in the urine. • Elimination – removal of waste from other organ systems - from digestive system – undigested food, water, salt, ions, and drugs. + - from respiratory system – CO2,H , water, toxins. - from skin – water, NaCl, nitrogenous wastes (urea , uric acid, ammonia, creatinine). • Water balance -- kidney tubules regulate water reabsorption and urine concentration. • regulation of PH, volume, and composition of body fluids. • production of Erythropoietin for hematopoieseis, and renin for blood pressure regulation. Anatomy of the Urinary System Gross anatomy: • kidneys – a pair of bean – shaped organs located retroperitoneally, responsible for blood filtering and urine formation. • Renal capsule – a layer of fibrous connective tissue covering the kidneys. • Renal cortex – outer region of the kidneys where most nephrons is located. • Renal medulla – inner region of the kidneys where some nephrons is located, also where urine is collected to be excreted outward. • Renal calyx – duct – like sections of renal medulla for collecting urine from nephrons and direct urine into renal pelvis. • Renal pyramid – connective tissues in the renal medulla binding various structures together. • Renal pelvis – central urine collecting area of renal medulla. • Hilum (or hilus) – concave notch of kidneys where renal artery, renal vein, urethra, nerves, and lymphatic vessels converge. • Ureter – a tubule that transport urine (mainly by peristalsis) from the kidney to the urinary bladder. • Urinary bladder – a spherical storage organ that contains up to 400 ml of urine. • Urethra – a tubule that excretes urine out of the urinary bladder to the outside, through the urethral orifice. -
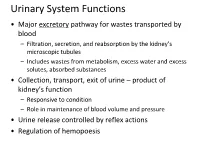
Urinary System Functions
Urinary System Functions • Major excretory pathway for wastes transported by blood – Filtration, secretion, and reabsorption by the kidney’s microscopic tubules – Includes wastes from metabolism, excess water and excess solutes, absorbed substances • Collection, transport, exit of urine – product of kidney’s function – Responsive to condition – Role in maintenance of blood volume and pressure • Urine release controlled by reflex actions • Regulation of hemopoesis Organs and Vessels of the Urinary System Hepatic veins (cut) Esophagus (cut) Inferior vena cava Renal artery Adrenal gland Renal hilum Aorta Renal vein Kidney Iliac crest Ureter - peristalsis Rectum (cut) Uterus (part of female reproductive system) Urinary bladder Urethra Figure 25.2 Dissection of urinary system organs (male). Kidney Renal artery Renal hilum Renal vein Ureter Urinary bladder Figure 25.3a Position of the kidneys against the posterior body wall. Three layers of supportive tissue surround kidney Renal fascia outer layer of dense fibrous connective tissue Perirenal fat capsule Fatty cushion Fibrous capsule Transparent capsule Anterior Inferior vena cava Aorta Peritoneum Peritoneal cavity (organs removed) Supportive Renal tissue layers vein • Renal fascia anterior Renal posterior artery • Perirenal fat capsule • Fibrous Body of capsule vertebra L2 Body wall Posterior Kidney Function Maintain the body’s internal environment by: – Regulating total water volume and total solute concentration in water – Regulating ion concentrations in ECF – Ensuring long-term acid-base -

The Distal Convoluted Tubule and Collecting Duct
Chapter 23 *Lecture PowerPoint The Urinary System *See separate FlexArt PowerPoint slides for all figures and tables preinserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Introduction • Urinary system rids the body of waste products. • The urinary system is closely associated with the reproductive system – Shared embryonic development and adult anatomical relationship – Collectively called the urogenital (UG) system 23-2 Functions of the Urinary System • Expected Learning Outcomes – Name and locate the organs of the urinary system. – List several functions of the kidneys in addition to urine formation. – Name the major nitrogenous wastes and identify their sources. – Define excretion and identify the systems that excrete wastes. 23-3 Functions of the Urinary System Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Diaphragm 11th and 12th ribs Adrenal gland Renal artery Renal vein Kidney Vertebra L2 Aorta Inferior vena cava Ureter Urinary bladder Urethra Figure 23.1a,b (a) Anterior view (b) Posterior view • Urinary system consists of six organs: two kidneys, two ureters, urinary bladder, and urethra 23-4 Functions of the Kidneys • Filters blood plasma, separates waste from useful chemicals, returns useful substances to blood, eliminates wastes • Regulate blood volume and pressure by eliminating or conserving water • Regulate the osmolarity of the body fluids by controlling the relative amounts of water and solutes -

Urinary System Kidney Anatomy Nephrons Let's Make the Filtrate
Kidney anatomy Urinary system Renal Aids homeostasis by cortex removing cellular wastes and Renal medulla foreign compounds, and Cortex maintains salt and water Renal balance of plasma pelvis Medulla Ureter Nephrons Let’s make the filtrate... Each kidney has about one million nephrons Blood is filtered at the glomerulus. Water Afferent arteriole brings and solutes leave the blood to glomerulus and blood and enter then forms efferent Bowman’s capsule. arteriole. Efferent arteriole branches to peritubular capillaries 1 Glomerulus physiology Bowman’s capsule contains podocytes that encircle Glomerular filtration the glomerulus. Glomerular filtration Normally blood cells and plasma proteins are not is similar to Capillary filtered ultrafiltration of 55 blood pressure capillaries Osmotic Hydrostatic 20% of plasma pressure 30 15 pressure becomes filtrate Glomerular filtration rate (GFR) determined by: Net filtration pressure and glomerulus permeability Adjusting GFR Filtrate is adjusted along the nephron Distal Blood pressure tubule Proximal tubule Cortex region Bowman’s capsule Radius of afferent arteriole Juxtaglomerular apparatus - helps in Decreasing GFR helps retain adjustments to filtration rate fluid and salts Loop of Henle Medulla region 2 Tubular reabsorption and secretion 180 liters per day are filtered, most is reabsorbed Reabsorption: filtered substances leave the nephron and enter peritubular capillaries Secretion: some substances from the peritubular capillaries enter the nephron So what is urine, then? Everything in the nephron that does not get Reabsorption physiology reabsorbed into the blood leaves as ….urine!!! 3 + Reabsorption of Na + (the key to it all…) Na reabsorption Na+ reabsorption (RA) drives the movement of many other substances in the tubule Water will “follow” Na+ movement Lumen Proximal tubular cell Control of sodium RA Page 533 When ECF volume is low, need to Na+ RA Osmosis Interstitial fluid Peritubular + Water capillary Na RA at distal and collection tubules with channel aldosterone. -

URINARY SYSTEM Components
Human Anatomy Unit 3 URINARY SYSTEM Components • Kidneys • Ureters • Urinary bladder • Urethra Funcons • Storage of urine – Bladder stores up to 1 L of urine • Excreon of urine – Transport of urine out of body • Regulaon: – Plasma pH – Blood volume/pressure – Plasma ion concentraons (Ca2+, Na+, K+, CL-) – Assist liver in detoxificaon, amino acid metabolism Kidney Gross Anatomy • Retroperitoneal – Anterior surface covered with peritoneum – Posterior surface directly against posterior abdominal wall • Superior surface at about T12 • Inferior surface at about L3 • Ureters enter urinary bladder posteriorly • LeT kidney 2cm superior to right – Size of liver Structure of the Kidney • Hilum = the depression along the medial border through which several structures pass – renal artery – renal vein – ureter – renal nerves Surrounding Tissue • Fibrous capsule – Innermost layer of dense irregular CT – Maintains shape, protec:on • Adipose capsule – Adipose ct of varying thickness – Cushioning and insulaon • Renal fascia – Dense irregular CT – Anchors kidney to peritoneum & abdominal wall • Paranephric fat – Outermost, adipose CT between renal fascia and peritoneum Frontal Sec:on of the Kidney • Cortex – Layer of renal :ssue in contact with capsule – Renal columns – parts of cortex that extend into the medulla between pyramids • Medulla – Striped due to renal tubules • Renal pyramids – 8-15 present in medulla of adult – Conical shape – Wide base at cor:comedullary juncon Flow of Filtrate/Urine • Collec:ng ducts – Collect from mul:ple nephrons • Minor calyx – Collect from each pyramid • Major calyx – Collect from minor calyx • Renal pelvis – Collects from calyces, passes onto • Ureter – Collects from pelvis • Urinary Bladder – Collects from ureters Histology Renal Cortex Renal Medulla Renal Tubules • Nephron – func:onal unit of the kidney. -
Lecture (1) Urinary System
UrinaryUrinaryUrinary systemsystemsystem Dr. Carmen E. Rexach Anatomy 35 Mt. San Antonio College Functions •Storage of urine – Bladder stores up to 1 L of urine • Excretion of urine – Transport of urine out of body • Blood volume regulation – Effects of hormones on kidneys • Regulation of erythrocyte production –Kidneys • Monitor oxygen content of blood • Produce EPO = erthrocyte production Components •Kidneys • Ureters • Urinary Bladder • Urethra Kidneys Gross Anatomy • Kidneys approx weight = 125- 150g each • Retroperitoneal – Anterior surface covered with peritoneum – Posterior surface directly against posterior abdominal wall • Superior surface at about T12 • Inferior surface at about L3 • ureters enter urinary bladder posteriorly • Left kidney 2cm superior to right –Size of liver Transverse section at L1 surface features of kidney • Hilum = the depression along the medial border through which several structures pass –renal artery –renal vein –ureter – renal nerves Surrounding structures • Fibrous capsule – Innermost layer of dense irregular CT – Maintains shape, protection • Adipose capsule (perinephric fat) – Adipose ct of varying thickness – Cushioning and insulation • Renal fascia – Dense irregular CT – Anchors kidney to peritoneum & abdominal wall • Paranephric fat – Outermost, adipose CT between renal fascia and peritoneum Coronal section •Cortex – layer of renal tissue in contact with capsule –Lighter shade –Renal columns= parts of cortex that extend into the medulla between pyramids •Medulla –Innermost – striped due to renal tubules •renal pyramids – 8-15 present in medulla of adult – conical shape – Wide base at corticomedullary junction Coronal section • Renal pelvis – collects from calyces, passes onto ureter •Calyces (pl) – funnel shaped regions – collect urine into pelvis •Minor calyx (s) – in contact with each pyramid •Major calyx (s) – collect from minor Microscopic Anatomy Microscopic anatomy Renal tubules • Nephron – functional unit of the kidney. -

The Urinary System Consists of Kidneys, Ureters, Urinary Bladder
Anatomy Lecture Notes Chapter 23 the urinary system consists of kidneys, ureters, urinary bladder, and urethra the function of the kidneys is NOT "to make urine" the kidneys: 1) regulate water balance 2) regular ECF electrolyte levels (Na, K, Ca) 3) eliminate some metabolic wastes urine is a by-product of these functions A. kidneys 1. located against posterior abdominal wall (retroperitoneal) T11 or T12 to L3 right kidney lower than left kidney 2. surrounded by a. pararenal fat (posterior only) b. renal fascia c. adipose capsule - perirenal fat d. renal capsule - dense c.t. covering surface of kidney e. parietal peritoneum Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 3. layers a. cortex - contains renal corpuscles and extends inwards as renal columns b. medulla - consists of renal pyramids which consist mostly of collecting ducts papilla - apex of renal pyramid; where collecting ducts drain into calyx 4. cavities and associated structures a. renal sinus - space in medial part of kidney; contains renal pelvis b. renal pelvis - expanded superior part of ureter minor calyx collects urine from one renal papilla major calyx formed by junction of 2 or more minor calyces renal pelvis formed by junction of all major calyces Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 5. renal hilum - medial indentation; where ureter leaves kidney 6. blood flow through the kidney - renal fraction = 20% of cardiac output aorta renal artery segmental arteries lobar arteries interlobar arteries arcuate arteries cortical radiate (interlobular) arteries afferent arterioles glomerular capillaries (glomerulus) efferent arteriole peritubular capillaries and vasa recta cortical radiate (interlobular) veins arcuate veins interlobar veins renal vein inferior vena cava Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 7. -

Phenotypic Diversity and Metabolic Specialization of Renal Endothelial Cells
REVIEWS Phenotypic diversity and metabolic specialization of renal endothelial cells Sébastien J. Dumas1,6, Elda Meta1,6, Mila Borri 1,6, Yonglun Luo 2,3, Xuri Li 4 ✉ , Ton J. Rabelink5 ✉ and Peter Carmeliet 1,4 ✉ Abstract | Complex multicellular life in mammals relies on functional cooperation of different organs for the survival of the whole organism. The kidneys play a critical part in this process through the maintenance of fluid volume and composition homeostasis, which enables other organs to fulfil their tasks. The renal endothelium exhibits phenotypic and molecular traits that distinguish it from endothelia of other organs. Moreover, the adult kidney vasculature comprises diverse populations of mostly quiescent, but not metabolically inactive, endothelial cells (ECs) that reside within the kidney glomeruli, cortex and medulla. Each of these populations supports specific functions, for example, in the filtration of blood plasma, the reabsorption and secretion of water and solutes, and the concentration of urine. Transcriptional profiling of these diverse EC populations suggests they have adapted to local microenvironmental conditions (hypoxia, shear stress, hyperosmolarity), enabling them to support kidney functions. Exposure of ECs to microenvironment- derived angiogenic factors affects their metabolism, and sustains kidney development and homeostasis, whereas EC- derived angiocrine factors preserve distinct microenvironment niches. In the context of kidney disease, renal ECs show alteration in their metabolism and phenotype in response to pathological changes in the local microenvironment, further promoting kidney dysfunction. Understanding the diversity and specialization of kidney ECs could provide new avenues for the treatment of kidney diseases and kidney regeneration. The mammalian vascular system consists of two con- three anatomical and functional compartments of the nected and highly branched networks that pervade kidney, the glomeruli, cortex and medulla — where they the whole body — each with specific roles. -
2 النسج the Urinary System الجهاز البولي محاضرة 9
النسج 2 The Urinary System الجهاز البولي محاضرة 9 أ. د. رائدة الخاني The Urinary System . Two kidneys . A ureter for each kidney . Urinary bladder . Urethra 2 Kidneys: . Dimensions: about 10x6x3cm . Protected by . Ribs 11 + 12 . Lateral surface is convex . Medial surface is concave ,contains: vessels سرة الكلية Renal Hilus . ureter and nerves . An adrenal gland lies superior to each kidney 3 4 Function . Filtration of blood (1700 L/day) and excreting urine (1L) . Eliminate waste products of metabolism in the urine . Regulating body fluid and salt balance . maintains the appropriate acid balance of plasma . Regulation of blood pressure . Hormone secretion: Endocrine function . Renin secretion: Regulation of blood pressure Function . Erythropoietin secretion: Kidney is the main organ for production of erythropoietin in postnatal life. Secreted by the interstitial fibroblasts in close association with the peritubular capillaries and proximal convoluted tubules. The steroid prohormone vitamin D, initially produced in skin keratinocytes, is hydroxylated in kidneys to an active form (1,25- dihydroxyvitamin D3 or calcitriol ) involved in regulating calcium balance. 6 . Kidney has two regions outer : القشر Cortex . inner : اللب Medulla . -Columns of cortex divide medulla into “pyramids”Darker, cone-shaped medullary or renal pyramids include collecting tubules 7 . Renal pelvis (=basin) . Superior part of ureter كؤيسات Branches to form two or three major calices . divide again, minor calices: collect urine from papillae of pyramids 8 Renal Arteries Right and left renal arteries are branches of the Aorta. They enter the kidney in the hilus and divide>> segmental A. >>9 segmental A. >> interlobar A. >> arcuate A. >> >>cortical radiate A. >> glomerular arterioles: afferent arterioles >> glomerular capillaries >> efferent arterioles. -

Molecular Determinants of Nephron Vascular Specialization in the Kidney
ARTICLE https://doi.org/10.1038/s41467-019-12872-5 OPEN Molecular determinants of nephron vascular specialization in the kidney David M. Barry1*, Elizabeth A. McMillan1, Balvir Kunar1, Raphael Lis1, Tuo Zhang 2, Tyler Lu1, Edward Daniel 3, Masataka Yokoyama1, Jesus M. Gomez-Salinero1, Angara Sureshbabu4, Ondine Cleaver3, Annarita Di Lorenzo5, Mary E. Choi4, Jenny Xiang2, David Redmond1, Sina Y. Rabbany1,6, Thangamani Muthukumar4 & Shahin Rafii1* 1234567890():,; Although kidney parenchymal tissue can be generated in vitro, reconstructing the complex vasculature of the kidney remains a daunting task. The molecular pathways that specify and sustain functional, phenotypic and structural heterogeneity of the kidney vasculature are unknown. Here, we employ high-throughput bulk and single-cell RNA sequencing of the non-lymphatic endothelial cells (ECs) of the kidney to identify the molecular pathways that dictate vascular zonation from embryos to adulthood. We show that the kidney manifests vascular-specific signatures expressing defined transcription factors, ion channels, solute transporters, and angiocrine factors choreographing kidney functions. Notably, the ontology of the glomerulus coincides with induction of unique transcription factors, including Tbx3, Gata5, Prdm1, and Pbx1. Deletion of Tbx3 in ECs results in glomerular hypoplasia, microaneurysms and regressed fenestrations leading to fibrosis in subsets of glomeruli. Deciphering the molecular determinants of kidney vascular signatures lays the foundation for rebuilding nephrons and uncovering the pathogenesis of kidney disorders. 1 Division of Regenerative Medicine, Ansary Stem Cell Institute, Weill Cornell Medicine, New York, NY 10065, USA. 2 Genomics Resources Core Facility, Weill Cornell Medicine, New York, NY 10065, USA. 3 Department of Molecular Biology, University of Texas Southwestern Medical Center, Dallas, TX 75235, USA. -

Human Anatomy & Physiology Introduction
Urinary System URLs Human Anatomy & Physiology 20 http://www.howstuffworks.com/kidney.htm/printable http://kidney.niddk.nih.gov/kudiseases/pubs/ Yoururinary/ http://content.jeffersonhospital.org/ Content.asp?PageID=P01468 http://nephron.com/htkw.html Karen Webb Smith Instructor Unit Five Introduction A. The urinary system consists of two kidneys that filter the blood, two ureters which transport urine from the kidneys, a urinary bladder which collects urine from the ureters & serves as a reservoir, & a tubular urethra to convey waste substances to the outside of the body. Next to your brain, your kidneys are The flow changes from something like a gushing some of the most complicated pieces river to many meandering streams. of equipment you have. In the next The ball of blood vessels is enclosed in a capsule minute more than one quart of blood made of 2 thin walls. The slowed blood has time to will pass through your kidneys. It will come out with filter into the surrounding membrane. All but the just the right wastes removed so it can continue to largest particles (like blood cells) filter through the carry on your life’s work. capsule into small tubes. These tubes are called Kidneys are filters. Each is a mass of more than a nephrons, & are where the cleaning takes place. million tiny filter tubes. Blood is filtered into these All of the valuable parts are reabsorbed into the tubes and then out again. Wastes are captured in blood. The wastes stay behind. All the threadlike these tubes and left behind. These wastes drain nephrons point to the kidney’s center.