Human Anatomy & Physiology Introduction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

35-40 Institute of Normal Anatomy
35 Lymphology 28 (1995) 35-40 Institute of Normal Anatomy (PP,AT), Institute of Histology and General Embryology (CM), and Department of Human Pathology (RS), University of Pavia, Italy ABSTRACT light and electron microscopy (2,3). To clarify vesical lymph drainage, we now examined the After endoscopic transurethral biopsies of fine structure of small lymphatic vessels (SL V) normal human urinary bladder, an extensive and their distribution in the normal human network of small initial lymphatic vessels was urinary bladder. Particular attention was depicted by means of light and electron directed to the structure and composition of microscopy. Using light microscopy, lymphatic the connective matrix that surrounds the vessels were seen in the mucosa and lymphatic vessels in the different regions of submucosa and formed a complex network in the bladder wall. the detrusor muscular coat. These lymphatics were characterized by an irregular and MATERIALS AND METHODS attenuated wall and increased in number and size from the superficial to the deeper region of Ten male subjects (40 to 60 years of age) the bladder. Ultrastructurally, the lymphatic who had symptoms of bladder outlet wall was characterized by endothelial cells obstruction were utilized for this investigation. joined together end-to-end or by complicated Two endoscopic transurethral biopsies from interdigitations. Often intercellular channels the lateral wall of the normal urinary bladder and gaps between two contiguous endothelial were performed under a constant bladder cells were present. A broad network of elastic distention after introduction of physiological and collagen fibers joined the lymphatic saline at 50 cm H20 constant pressure. The endothelial wall to the neighboring connective biopsy trocar was regulated to obtain vesical tissue. -

Clinical and Functional Anatomy of the Urethral Sphincter
Review Article International Neurourology Journal Int Neurourol J 2012;16:102-106 http://dx.doi.org/10.5213/inj.2012.16.3.102 pISSN 2093-4777 · eISSN 2093-6931 INJ Clinical and Functional Anatomy of the Urethral Sphincter Junyang Jung, Hyo Kwang Ahn, Youngbuhm Huh Department of Anatomy, Kyung Hee University School of Medicine, Seoul, Korea Continence and micturition involve urethral closure. Especially, insufficient strength of the pelvic floor muscles including the urethral sphincter muscles causes urinary incontinence (UI). Thus, it is most important to understand the main mechanism causing UI and the relationship of UI with the urethral sphincter. Functionally and anatomically, the urethral sphincter is made up of the internal and the external sphincter. We highlight the basic and clinical anatomy of the internal and the external sphinc- ter and their clinical meaning. Understanding these relationships may provide a novel view in identifying the main mechanism causing UI and surgical techniques for UI. Keywords: Urethral sphincters; Pudendal nerve; Autonomic nervous system; Urinary incontinence; Urination INTRODUCTION tomical damage to the ligaments, facial support, and pelvic floor musculature, including the levator ani [8]. The pudendal nerve The urethral sphincter is crucial for the maintenance of urinary innervating the EUS is susceptible to injury during vaginal birth continence [1,2]. The urethral sphincter refers to one of the fol- because it travels between the sacrospinous and sacrotuberous lowing muscles [3]: 1) the internal urethral sphincter (IUS), ligaments [9]. In this article, we discuss the basic and clinical which consists of smooth muscle and is continuous with the anatomy of the urethral sphincter and the relationship between detrusor muscle and under involuntary control, and 2) the ex- the urethral sphincter and UI. -

Regulation of Bladder Storage and Voiding Involves Both Sympathetic
Center for Advanced Gyn 5530 Wisconsin Ave Suite 914 Chevy Chase, MD 20815 301-652-1231 Regulation of bladder www.centerforadvancedgyn.com storage and voiding involves both sympathetic and parasympathetic control1 BLADDER STORAGE Storage, which makes up the majority of the micturition cycle, is primarily regulated by the sympathetic nervous system via the neurotransmitter, norepinephrine.2 • Norepinephrine, released from the sympathetic nerves, activates the adrenergic receptors (ARs), beta-ARs, and alpha-ARs in the bladder to relax the detrusor muscle and close the internal sphincter, respectively2 β-ARs Norepinephrine Ureter β-AR Norepinephrine binds to β-ARs on Sympathetic the detrusor muscle, resulting in nervous system bladder relaxation α-ARs Urothelium -AR α1 Detrusor muscle Internal sphincter Norepinephrine Urethra Norepinephrine binds to α1-ARs, resulting in the closing of the internal sphincter and increased storage of urine Three different types of b-ARs are expressed in the human bladder: b1-AR, b2-AR, and b3-AR. The b3-AR made up 97% of the total b-AR messenger RNA (mRNA) in bladder tissue samples in an experiment to determine b-AR subtype expression, making it predominantly responsible for detrusor muscle relaxation. The b1-AR and b2-AR subtypes made up 1.5% and 1.4% of the total b-AR mRNA, respectively.3 While b-ARs are expressed on the detrusor muscle, they are also found on the urothelium. These receptors contribute to the regulation of bladder function. During the storage phase, the urothelium stretches in tandem with the bladder wall when the bladder starts filling with urine.4,5 6 Both a1-ARs and a2-ARs are expressed in the lower urinary tract in humans. -

Urinary System
OUTLINE 27.1 General Structure and Functions of the Urinary System 818 27.2 Kidneys 820 27 27.2a Gross and Sectional Anatomy of the Kidney 820 27.2b Blood Supply to the Kidney 821 27.2c Nephrons 824 27.2d How Tubular Fluid Becomes Urine 828 27.2e Juxtaglomerular Apparatus 828 Urinary 27.2f Innervation of the Kidney 828 27.3 Urinary Tract 829 27.3a Ureters 829 27.3b Urinary Bladder 830 System 27.3c Urethra 833 27.4 Aging and the Urinary System 834 27.5 Development of the Urinary System 835 27.5a Kidney and Ureter Development 835 27.5b Urinary Bladder and Urethra Development 835 MODULE 13: URINARY SYSTEM mck78097_ch27_817-841.indd 817 2/25/11 2:24 PM 818 Chapter Twenty-Seven Urinary System n the course of carrying out their specific functions, the cells Besides removing waste products from the bloodstream, the uri- I of all body systems produce waste products, and these waste nary system performs many other functions, including the following: products end up in the bloodstream. In this case, the bloodstream is ■ Storage of urine. Urine is produced continuously, but analogous to a river that supplies drinking water to a nearby town. it would be quite inconvenient if we were constantly The river water may become polluted with sediment, animal waste, excreting urine. The urinary bladder is an expandable, and motorboat fuel—but the town has a water treatment plant that muscular sac that can store as much as 1 liter of urine. removes these waste products and makes the water safe to drink. -

The Urinary System Dr
The urinary System Dr. Ali Ebneshahidi Functions of the Urinary System • Excretion – removal of waste material from the blood plasma and the disposal of this waste in the urine. • Elimination – removal of waste from other organ systems - from digestive system – undigested food, water, salt, ions, and drugs. + - from respiratory system – CO2,H , water, toxins. - from skin – water, NaCl, nitrogenous wastes (urea , uric acid, ammonia, creatinine). • Water balance -- kidney tubules regulate water reabsorption and urine concentration. • regulation of PH, volume, and composition of body fluids. • production of Erythropoietin for hematopoieseis, and renin for blood pressure regulation. Anatomy of the Urinary System Gross anatomy: • kidneys – a pair of bean – shaped organs located retroperitoneally, responsible for blood filtering and urine formation. • Renal capsule – a layer of fibrous connective tissue covering the kidneys. • Renal cortex – outer region of the kidneys where most nephrons is located. • Renal medulla – inner region of the kidneys where some nephrons is located, also where urine is collected to be excreted outward. • Renal calyx – duct – like sections of renal medulla for collecting urine from nephrons and direct urine into renal pelvis. • Renal pyramid – connective tissues in the renal medulla binding various structures together. • Renal pelvis – central urine collecting area of renal medulla. • Hilum (or hilus) – concave notch of kidneys where renal artery, renal vein, urethra, nerves, and lymphatic vessels converge. • Ureter – a tubule that transport urine (mainly by peristalsis) from the kidney to the urinary bladder. • Urinary bladder – a spherical storage organ that contains up to 400 ml of urine. • Urethra – a tubule that excretes urine out of the urinary bladder to the outside, through the urethral orifice. -
Urinary System Functions
Urinary System Functions • Major excretory pathway for wastes transported by blood – Filtration, secretion, and reabsorption by the kidney’s microscopic tubules – Includes wastes from metabolism, excess water and excess solutes, absorbed substances • Collection, transport, exit of urine – product of kidney’s function – Responsive to condition – Role in maintenance of blood volume and pressure • Urine release controlled by reflex actions • Regulation of hemopoesis Organs and Vessels of the Urinary System Hepatic veins (cut) Esophagus (cut) Inferior vena cava Renal artery Adrenal gland Renal hilum Aorta Renal vein Kidney Iliac crest Ureter - peristalsis Rectum (cut) Uterus (part of female reproductive system) Urinary bladder Urethra Figure 25.2 Dissection of urinary system organs (male). Kidney Renal artery Renal hilum Renal vein Ureter Urinary bladder Figure 25.3a Position of the kidneys against the posterior body wall. Three layers of supportive tissue surround kidney Renal fascia outer layer of dense fibrous connective tissue Perirenal fat capsule Fatty cushion Fibrous capsule Transparent capsule Anterior Inferior vena cava Aorta Peritoneum Peritoneal cavity (organs removed) Supportive Renal tissue layers vein • Renal fascia anterior Renal posterior artery • Perirenal fat capsule • Fibrous Body of capsule vertebra L2 Body wall Posterior Kidney Function Maintain the body’s internal environment by: – Regulating total water volume and total solute concentration in water – Regulating ion concentrations in ECF – Ensuring long-term acid-base -
Bladder Retraining
James Paget University Hospitals NHS Foundation Trust Bladder retraining Patient Information How should my bladder work? Urine is made in the kidneys and travels down two tubes called the ureters to the bladder. The bladder is a storage organ that expands to store the urine. The urethra is the tube that runs from the bladder to the outside of your body, just in front of the vagina, or through the penis. A healthy bladder usually holds around 400ml-600ml (0.75–1 pint). The number of times you pass urine each day depends on a number of things, including how much fluid you drink. It may be normal to pass urine up to seven times a day and up to once during the night. If you are older (more than 70 years old) passing urine once or twice at night may be normal. 2 As the bladder starts to fill it sends a warning message to the brain. You normally feel the first warning when your bladder has about 200mls (1/3 of a pint) in it. If it is not convenient to go to the toilet at that time, your brain sends messages to your bladder telling it to relax. This allows you to continue with whatever you are doing at the time. The desire to empty your bladder will gradually become stronger and more difficult to put off or control. When you find an appropriate time to empty your bladder, you sit on the toilet (or probably stand up if you’re a man), relax your pelvic floor muscles and your bladder muscle (detrusor muscle) starts to contract, expelling the urine. -

The Female Pelvic Floor Fascia Anatomy: a Systematic Search and Review
life Systematic Review The Female Pelvic Floor Fascia Anatomy: A Systematic Search and Review Mélanie Roch 1 , Nathaly Gaudreault 1, Marie-Pierre Cyr 1, Gabriel Venne 2, Nathalie J. Bureau 3 and Mélanie Morin 1,* 1 Research Center of the Centre Hospitalier Universitaire de Sherbrooke, Faculty of Medicine and Health Sciences, School of Rehabilitation, Université de Sherbrooke, Sherbrooke, QC J1H 5N4, Canada; [email protected] (M.R.); [email protected] (N.G.); [email protected] (M.-P.C.) 2 Anatomy and Cell Biology, Faculty of Medicine and Health Sciences, McGill University, Montreal, QC H3A 0C7, Canada; [email protected] 3 Centre Hospitalier de l’Université de Montréal, Department of Radiology, Radio-Oncology, Nuclear Medicine, Faculty of Medicine, Université de Montréal, Montreal, QC H3T 1J4, Canada; [email protected] * Correspondence: [email protected] Abstract: The female pelvis is a complex anatomical region comprising the pelvic organs, muscles, neurovascular supplies, and fasciae. The anatomy of the pelvic floor and its fascial components are currently poorly described and misunderstood. This systematic search and review aimed to explore and summarize the current state of knowledge on the fascial anatomy of the pelvic floor in women. Methods: A systematic search was performed using Medline and Scopus databases. A synthesis of the findings with a critical appraisal was subsequently carried out. The risk of bias was assessed with the Anatomical Quality Assurance Tool. Results: A total of 39 articles, involving 1192 women, were included in the review. Although the perineal membrane, tendinous arch of pelvic fascia, pubourethral ligaments, rectovaginal fascia, and perineal body were the most frequently described structures, uncertainties were Citation: Roch, M.; Gaudreault, N.; identified in micro- and macro-anatomy. -

ANAT1551 Introductory Anatomy
Faculty of Medicine School of Medical Sciences ANAT1551 Introductory Anatomy Session 2 - 2013 Introductory Anatomy for Health & Exercise Science – Session 2, 2013 Contents Course convenor 2 Units of credit 2 Hours per week 2 What is anatomy? 2 Course aims 2 Student learning outcomes 2 Course relationships 3 Teaching rationale 4 Teaching strategies 4 Ethical behaviour and human remains 4 Anatomical terms 4 Assessment 5 Failure to sit a test 5 Resources for students 6 What is plagiarism? 6 Grievance procedures 7 Continual course improvement 7 Practical Class Attendance Requirement 7 Guidelines on extra-curricular activities affecting attendance 7 Health and Safety Rules for Students in the Dissecting Room 9 Course Lecture and Practical Class Schedule 12 Week 1: General Anatomy and Skeletal System 1 13 Week 2: Skeletal System 2 & Articular System 18 Week 3: Muscular System 1 22 Week 4: Muscular System 2 and Spinal Cord 26 Week 5: Spinal Nerves and the Autonomic Nervous System 29 Week 6: Revision Lab (9am-12pm Thursday 05/09/2013) 32 Spot Test No.1 (11am-12pm or 12-1pm Friday 06/09/2013) 32 Week 7: Brain and Cranial Nerves 33 Week 8: Eye and Ear 36 Week 9: Cardiovascular System 40 Week 10: Respiratory System 44 Week 11: Digestive System 47 Week 12: Urinary and Reproductive Systems 51 Week 13: Revision Lab (9am-12pm Thursday 31/10/2013) 54 Spot Test No.2 (11am-12pm or 12-1pm Friday 01/11/2013) 54 Cover illustration: One of the Vesalius plates (drawn by Calcar). From: Hixson, J. 1966. The History of the Human Body. -

The Distal Convoluted Tubule and Collecting Duct
Chapter 23 *Lecture PowerPoint The Urinary System *See separate FlexArt PowerPoint slides for all figures and tables preinserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Introduction • Urinary system rids the body of waste products. • The urinary system is closely associated with the reproductive system – Shared embryonic development and adult anatomical relationship – Collectively called the urogenital (UG) system 23-2 Functions of the Urinary System • Expected Learning Outcomes – Name and locate the organs of the urinary system. – List several functions of the kidneys in addition to urine formation. – Name the major nitrogenous wastes and identify their sources. – Define excretion and identify the systems that excrete wastes. 23-3 Functions of the Urinary System Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Diaphragm 11th and 12th ribs Adrenal gland Renal artery Renal vein Kidney Vertebra L2 Aorta Inferior vena cava Ureter Urinary bladder Urethra Figure 23.1a,b (a) Anterior view (b) Posterior view • Urinary system consists of six organs: two kidneys, two ureters, urinary bladder, and urethra 23-4 Functions of the Kidneys • Filters blood plasma, separates waste from useful chemicals, returns useful substances to blood, eliminates wastes • Regulate blood volume and pressure by eliminating or conserving water • Regulate the osmolarity of the body fluids by controlling the relative amounts of water and solutes -
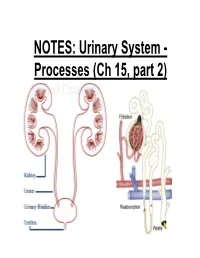
NOTES: Urinary System
NOTES: Urinary System - Processes (Ch 15, part 2) *Recall: the primary function of the urinary system is to filter the blood of ions and nitrogenous wastes; when combined with water, these wastes make up URINE. • Kidneys receive about 20-25% of total cardiac output – ~1200mL of blood goes through the kidneys per minute Blood Supply to Kidneys • Descending aorta Renal artery interlobar arcuate cortical afferent arterioles • The afferent arterioles deliver blood to nephrons NEPHRONS • NEPHRONS: the functional units of the kidneys -each kidney contains about a million nephrons! Parts of a NEPHRON: • GLOMERULUS: tangled cluster of blood capillaries • GLOMERULAR CAPSULE (a.k.a. Bowman’s capsule): thin-walled structure surrounding glomerulus Parts of a NEPHRON: • PROXIMAL CONVOLUTED TUBULE • LOOP OF HENLE -descending limb -ascending limb • DISTAL CONVOLUTED TUBULE Parts of a NEPHRON: • COLLECTING DUCT (where distal tubules from several nephrons converge and drain into; from here, urine empties into the RENAL PELVIS) Blood Supply of a Nephron: -blood is brought to a nephron from an afferent arteriole; -from here, it is passed to an efferent arteriole; -this gives rise to a system of peritubular capillaries that surround the renal tubules URINE FORMATION *nephrons remove wastes from blood and regulate water and electrolyte concentrations. URINE IS THE END PRODUCT! Three Organic Wastes Products of Urine 1) Urea: most abundant, from breakdown of amino acids 2) Creatinine: generated in skeletal muscle when creatine phosphate is broken down (creatine -

Bladder Dysfunction in Multiple Sclerosis
A RESOURCE FOR HEALTHCARE PROFESSIONALS BLADDER DYSFUNCTION IN MULTIPLE SCLEROSIS Rebecca Lavelle, MD Nancy J. Holland, EdD, RN Nancy C. Reitman, MA, RN Effective diagnosis and management of bladder dysfunction makes it possible for people with multiple sclerosis (MS) to continue their recreational and work activities with comfort, dignity and confidence. It is important to note that: • Bladder dysfunction occurs in approximately 80% of people living with MS, in people with minimal symptoms and those with major impairments. • Bladder symptoms, including frequency, urgency and incontinence, may negatively impact social and vocational activities. • Bladder symptoms are often mismanaged, precipitating such problems as acute urinary retention, damage to the detrusor (primary bladder muscle) and urinary tract infections (UTIs). NORMAL BLADDER FUNCTION The bladder wall consists of three main layers: the mucosa, submucosa, and detrusor muscle. The detrusor, a thick layer of smooth muscle, expands to store urine and contracts to expel urine. Storage and emptying of the bladder are regulated by the internal and external urethral sphincters. Sphincters are normally in a closed position, needing stimulation to open. Continence depends on sphincter–detrusor coordination. When approximately 250 to 300 cc of urine fill the bladder, the internal pressure activates stretch receptors in the bladder wall. The stretch receptors signal the nervous system, small contractile waves occur in the detrusor muscle, and the internal urethral sphincter automatically relaxes. The external sphincter is consciously tightened and the urge to urinate becomes apparent. Voluntary voiding occurs when two actions occur simultaneously: the detrusor muscle contracts to expel the urine and the external sphincter relaxes and opens to allow the urine to pass freely into the urethra and out of the body.