COVID-19 Vaccination Policy Faqs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Implementation of Mass-Vaccination Against SARS-Cov-2: a Systematic Review of Existing Strategies and Guidelines
Review The Implementation of Mass-Vaccination against SARS-CoV-2: A Systematic Review of Existing Strategies and Guidelines Tasnim Hasan 1,2, Justin Beardsley 1, Ben J. Marais 3 , Thu Anh Nguyen 2 and Greg J. Fox 1,2,* 1 Faculty of Medicine and Health, The University of Sydney, Sydney, NSW 2006, Australia; [email protected] (T.H.); [email protected] (J.B.) 2 The Woolcock Institute of Medical Research, Glebe, NSW 2037, Australia; [email protected] 3 Marie Bahir Institute, The University of Sydney, Westmead, NSW 2145, Australia; [email protected] * Correspondence: [email protected] Abstract: The global drive to vaccinate against severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) began in December 2020 with countries in Europe, Middle East, and North America leading the roll out of a mass-vaccination program. This systematic review synthesised all available English-language guidelines and research regarding mass-vaccination for COVID-19 until 1 March 2021—the first three months of the global mass-vaccination effort. Data were extracted from national websites, PubMed, Embase, Medline and medRxiv, including peer and non-peer review research findings. A total of 15 national policy documents were included. Policies were summarised according to the World Health Organisation (WHO) framework for mass vaccination. All included policies prioritised front-line health care workers and the elderly. Limited information was available regarding staffing, cold chain, communication strategies and infrastructure requirements for effective vaccine Citation: Hasan, T.; Beardsley, J.; delivery. A total of 26 research studies were identified, reporting roll-out strategies, vaccine uptake Marais, B.J.; Nguyen, T.A.; Fox, G.J. -

From the Factory to the Frontlines the Operation Warp Speed Strategy for Distributing a COVID-19 Vaccine
From the Factory to the Frontlines The Operation Warp Speed Strategy for Distributing a COVID-19 Vaccine What This Strategy Aims to Do This report to Congress details a strategy to achieve the principal purpose and objective of Operation Warp Speed (OWS): ensuring that every American who wants to receive a COVID-19 vaccine can receive one, by delivering safe and effective vaccine doses to the American people beginning January 2021. The leadership of OWS has committed to being transparent with Congress, the media, and the American people. OWS has provided regular briefings on topics of interest to Congress and the media and will continue to provide updates and announcements as OWS reaches new milestones. Congress has been a vital partner in the all-of-America response to the COVID-19 pandemic. With support provided through emergency supplemental and flexible discretionary funding, OWS has now made strong progress toward a safe and effective COVID-19 vaccine, with multiple candidates in Phase 3 clinical trials. Simultaneously, OWS and partners are developing a plan for delivering a safe and effective product to Americans as quickly and reliably as possible. Experts from the Department of Health and Human Services (HHS) are leading vaccine development, while experts from the Department of Defense (DoD) are partnering with the Centers for Disease Control and Prevention (CDC) and other parts of HHS to coordinate supply, production, and distribution of vaccines. Successful implementation of the national COVID-19 vaccination program requires precise coordination across federal, state, local, tribal, and territorial governments and among many public and private partners. -

The Hepatitis B Vaccine Is the Most Widely Used Vaccine in the World, with Over 1 Billion Doses Given
Hepatitis B Vaccine Protect Yourself and Those You Love What is Hepatitis B? Hepatitis B is the most common serious liver infection in the world. It is caused by the hepatitis B virus (HBV), which attacks liver cells and can lead to liver failure, cirrhosis (scarring), or liver cancer later in life. The virus is transmitted through direct contact with infected blood and bodily fluids, and from an infected woman to her newborn at birth. Is there a safe vaccine for hepatitis B? YES! The good news is that there is a safe and effective vaccine for hepatitis B. The vaccine is a series, typically given as three shots over a six-month period that will provide a lifetime of protection. You cannot get hepatitis B from the vaccine – there is no human blood or live virus in the vaccine. The hepatitis B vaccine is the most widely used vaccine in the world, with over 1 billion doses given. The hepatitis B vaccine is the first "anti-cancer" vaccine because it can help prevent liver cancer! Who should be vaccinated against hepatitis B? The World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (CDC) recommend the hepatitis B vaccine for all newborns and children up to 18 years of age, and all high-risk adults. All infants should receive the first dose of the vaccine in the delivery room or in the first 24 hours of life, preferably within 12 hours. (CDC recommends the first dose within 12 hours vs. the WHO recommendation of 24 hours.) The HBV vaccine is recommended to anyone who is at high risk of infection. -
Provided By: Techserve Alliance
Provided by: TechServe Alliance Table of Contents Introduction .............................................................................................. 4 Return-to-Work at a Glance ....................................................................... 5 COVID-19 Return-to-Work Plans ..................................................................................... 5 Other Return-to-Work Considerations ........................................................................... 7 COVID-19 Vaccine Overview ....................................................................... 8 COVID-19 Vaccines and the Workplace ..................................................... 11 Government Guidance Related to COVID-19 Vaccines and Workplaces ...................11 OSHA Perspective ............................................................................... 11 EEOC Perspective ................................................................................ 11 Deciding Between a Mandatory or Voluntary Vaccination Policy ..............................13 General Employer Considerations ..................................................... 13 The Case for Mandatory Workplace Vaccination............................. 14 The Case for Voluntary Workplace Vaccination ............................... 14 Developing a Workplace Vaccination Plan ...................................................................16 Step 1: Gauge the Situation .............................................................. 16 Step 2: Make the Choice ................................................................... -

Would Parents Get Their Children Vaccinated Against SARS-Cov-2? Rate and Predictors of Vaccine Hesitancy According to a Survey Over 5000 Families from Bologna, Italy
Article Would Parents Get Their Children Vaccinated Against SARS-CoV-2? Rate and Predictors of Vaccine Hesitancy According to a Survey over 5000 Families from Bologna, Italy Marco Montalti 1,* , Flavia Rallo 1, Federica Guaraldi 2, Lapo Bartoli 3, Giulia Po 4 , Michela Stillo 5, Paola Perrone 5, Lorena Squillace 5, Laura Dallolio 1 , Paolo Pandolfi 5, Davide Resi 5, Maria Pia Fantini 1 , Chiara Reno 1 and Davide Gori 1 1 Unit of Hygiene, Department of Biomedical and Neuromotor Sciences, Public Health and Medical Statistics, University of Bologna, 40126 Bologna, Italy; fl[email protected] (F.R.); [email protected] (L.D.); [email protected] (M.P.F.); [email protected] (C.R.); [email protected] (D.G.) 2 IRCCS Istituto delle Scienze Neurologiche di Bologna, 40139 Bologna, Italy; [email protected] 3 Unit of Primary Health Care, Department of Medical and Surgical Sciences, University of Bologna, 40126 Bologna, Italy; [email protected] 4 School of Hygiene and Preventive Medicine, University of Ferrara, 44121 Ferrara, Italy; [email protected] 5 Department of Public Health, Bologna Local Health Authority, 40124 Bologna, Italy; [email protected] (M.S.); [email protected] (P.P.); [email protected] (L.S.); paolo.pandolfi@ausl.bologna.it (P.P.); [email protected] (D.R.) * Correspondence: [email protected]; Tel.: +39-051-209-4802 Citation: Montalti, M.; Rallo, F.; Guaraldi, F.; Bartoli, L.; Po, G.; Stillo, Abstract: In the near future, COVID-19 vaccine efficacy trials in larger cohorts may offer the possibility M.; Perrone, P.; Squillace, L.; Dallolio, to implement child and adolescent vaccination. -

Suggested Limitations of the Public Policy Doctrine Charles B
University of Minnesota Law School Scholarship Repository Minnesota Law Review 1935 Suggested Limitations of the Public Policy Doctrine Charles B. Nutting Follow this and additional works at: https://scholarship.law.umn.edu/mlr Part of the Law Commons Recommended Citation Nutting, Charles B., "Suggested Limitations of the Public Policy Doctrine" (1935). Minnesota Law Review. 993. https://scholarship.law.umn.edu/mlr/993 This Article is brought to you for free and open access by the University of Minnesota Law School. It has been accepted for inclusion in Minnesota Law Review collection by an authorized administrator of the Scholarship Repository. For more information, please contact [email protected]. MINNESOTA LAW REVIEW SUGGESTED LIMITATIONS OF THE PUBLIC POLICY DOCTRINE By CHARLES B. NUTTING* ECENT activity among writers in the field of the conflict of laws has revealed an awakened interest in the ever-vexing problem of determining the law applicable to situations in which the law of the forum differs from that of some other jurisdiction which may govern.' Apparently proceeding on the assumption that a court in such case is at liberty to select the law to be applied, varying suggestions have been made as to the criterion to be adopted. If the vested rights theory of conflicts is followed, much of this discussion becomes irrelevant, since under that theory there is, strictly speaking, no "choice" of law, one law and one alone being properly applicable in every case.- Whether this or some other theory embodies the true explanation of conflicts cases, we may leave to those who hurl thunderbolts about Olympus.' The writer, being sympathetically inclined toward the high church party in these matters, favors it for reasons which will appear hereafter. -
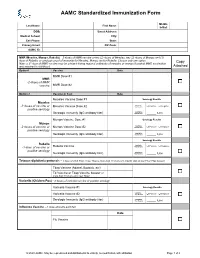
AAMC Standardized Immunization Form
AAMC Standardized Immunization Form Middle Last Name: First Name: Initial: DOB: Street Address: Medical School: City: Cell Phone: State: Primary Email: ZIP Code: AAMC ID: MMR (Measles, Mumps, Rubella) – 2 doses of MMR vaccine or two (2) doses of Measles, two (2) doses of Mumps and (1) dose of Rubella; or serologic proof of immunity for Measles, Mumps and/or Rubella. Choose only one option. Copy Note: a 3rd dose of MMR vaccine may be advised during regional outbreaks of measles or mumps if original MMR vaccination was received in childhood. Attached Option1 Vaccine Date MMR Dose #1 MMR -2 doses of MMR vaccine MMR Dose #2 Option 2 Vaccine or Test Date Measles Vaccine Dose #1 Serology Results Measles Qualitative -2 doses of vaccine or Measles Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Mumps Vaccine Dose #1 Serology Results Mumps Qualitative -2 doses of vaccine or Mumps Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Serology Results Rubella Qualitative Positive Negative -1 dose of vaccine or Rubella Vaccine Titer Results: positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Tetanus-diphtheria-pertussis – 1 dose of adult Tdap; if last Tdap is more than 10 years old, provide date of last Td or Tdap booster Tdap Vaccine (Adacel, Boostrix, etc) Td Vaccine or Tdap Vaccine booster (if more than 10 years since last Tdap) Varicella (Chicken Pox) - 2 doses of varicella vaccine or positive serology Varicella Vaccine #1 Serology Results Qualitative Varicella Vaccine #2 Titer Results: Positive Negative Serologic Immunity (IgG antibody titer) Quantitative Titer Results: _____ IU/ml Influenza Vaccine --1 dose annually each fall Date Flu Vaccine © 2020 AAMC. -

Hepatitis B Vaccine – Frequently Asked Questions (Information from the CDC)
AAMC Standardized Immunization Form 2020 Hepatitis B Vaccine – Frequently Asked Questions (Information from the CDC) 1. What are the hepatitis B vaccines licensed for use in the United States? Three single-antigen vaccines and two combination vaccines are currently licensed in the United States. Single-antigen hepatitis B vaccines: • ENGERIX-B® • RECOMBIVAX HB® • HEPLISAV-B™ Combination vaccines: • PEDIARIX®: Combined hepatitis B, diphtheria, tetanus, acellular pertussis (DTaP), and inactivated poliovirus (IPV) vaccine. Cannot be administered before age 6 weeks or after age 7 years. • TWINRIX®: Combined Hepatitis A and hepatitis B vaccine. Recommended for people aged ≥18 years who are at increased risk for both HAV and HBV infections. 2. What are the recommended schedules for hepatitis B vaccination? The vaccination schedule most often used for children and adults is three doses given at 0, 1, and 6 months. Alternate schedules have been approved for certain vaccines and/or populations. A new formulation, Heplisav-B (HepB-CpG), is approved to be given as two doses one month apart. 3. If there is an interruption between doses of hepatitis B vaccine, does the vaccine series need to be restarted? No. The series does not need to be restarted but the following should be considered: • If the vaccine series was interrupted after the first dose, the second dose should be administered as soon as possible. • The second and third doses should be separated by an interval of at least 8 weeks. • If only the third dose is delayed, it should be administered as soon as possible. 4. Is it harmful to administer an extra dose of hepatitis B vaccine or to repeat the entire vaccine series if documentation of the vaccination history is unavailable or the serology test is negative? No, administering extra doses of single-antigen hepatitis B vaccine is not harmful. -

COVID-19 Vaccines Frequently Asked Questions
Page 1 of 12 COVID-19 Vaccines 2020a Frequently Asked Questions Michigan.gov/Coronavirus The information in this document will change frequently as we learn more about COVID-19 vaccines. There is a lot we are learning as the pandemic and COVID-19 vaccines evolve. The approach in Michigan will adapt as we learn more. September 29, 2021. Quick Links What’s new | Why COVID-19 vaccination is important | Booster and additional doses | What to expect when you get vaccinated | Safety of the vaccine | Vaccine distribution/prioritization | Additional vaccine information | Protecting your privacy | Where can I get more information? What’s new − Pfizer booster doses recommended for some people to boost waning immunity six months after completing the Pfizer vaccine. Why COVID-19 vaccination is important − If you are fully vaccinated, you don’t have to quarantine after being exposed to COVID-19, as long as you don’t have symptoms. This means missing less work, school, sports and other activities. − COVID-19 vaccination is the safest way to build protection. COVID-19 is still a threat, especially to people who are unvaccinated. Some people who get COVID-19 can become severely ill, which could result in hospitalization, and some people have ongoing health problems several weeks or even longer after getting infected. Even people who did not have symptoms when they were infected can have these ongoing health problems. − After you are fully vaccinated for COVID-19, you can resume many activities that you did before the pandemic. CDC recommends that fully vaccinated people wear a mask in public indoor settings if they are in an area of substantial or high transmission. -

1 Democratic Deliberation and Social Choice: a Review Christian List1
1 Democratic Deliberation and Social Choice: A Review Christian List1 This version: June 2017 Forthcoming in the Oxford Handbook of Deliberative Democracy 1. Introduction In normative political theory, it is widely accepted that democratic decision making cannot be reduced to voting alone, but that it requires reasoned and well-informed discussion by those involved in and/or subject to the decisions in question, under conditions of equality and respect. In short, democracy requires deliberation (e.g., Cohen 1989; Gutmann and Thompson 1996; Dryzek 2000; Fishkin 2009; Mansbridge et al. 2010). In formal political theory, by contrast, the study of democracy has focused less on deliberation, and more on the aggregation of individual preferences or opinions into collective decisions – social choices – typically through voting (e.g., Arrow 1951/1963; Riker 1982; Austen-Smith and Banks 2000, 2005; Mueller 2003). While the literature on deliberation has an optimistic flavour, the literature on social choice is more mixed. It is centred around several paradoxes and impossibility results showing that collective decision making cannot generally satisfy certain plausible desiderata. Any democratic aggregation rule that we use in practice seems, at best, a compromise. Initially, the two literatures were largely disconnected from each other. Since the 1990s, however, there has been a growing dialogue between them (e.g., Miller 1992; Knight and Johnson 1994; van Mill 1996; Dryzek and List 2003; Landa and Meirowitz 2009). This chapter reviews the connections between the two. Deliberative democratic theory is relevant to social choice theory in that deliberation can complement aggregation and open up an escape route from some of its negative results. -
Immunogenicity and Safety of a Third Dose, and Immune Persistence Of
medRxiv preprint doi: https://doi.org/10.1101/2021.07.23.21261026; this version posted July 25, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. 1 Immunogenicity and safety of a third dose, and immune persistence of 2 CoronaVac vaccine in healthy adults aged 18-59 years: interim results 3 from a double-blind, randomized, placebo-controlled phase 2 clinical 4 trial 5 6 Hongxing Pan MSc1*, Qianhui Wu MPH2*, Gang Zeng Ph.D.3*, Juan Yang Ph.D.1, Deyu 7 Jiang MSc4, Xiaowei Deng MSc2, Kai Chu MSc1, Wen Zheng BSc2, Fengcai Zhu M.D.5†, 8 Hongjie Yu M.D. Ph.D.2,6,7†, Weidong Yin MBA8† 9 10 Affiliations 11 1. Vaccine Evaluation Institute, Jiangsu Provincial Center for Disease Control and 12 Prevention, Nanjing, China 13 2. School of Public Health, Fudan University, Key Laboratory of Public Health Safety, 14 Ministry of Education, Shanghai, China 15 3. Clinical Research Department, Sinovac Biotech Co., Ltd., Beijing, China 16 4. Covid-19 Vaccine Department, Sinovac Life Sciences Co., Ltd., Beijing, China 17 5. Jiangsu Provincial Center for Disease Control and Prevention, Nanjing, China 18 6. Shanghai Institute of Infectious Disease and Biosecurity, Fudan University, 19 Shanghai, China 20 7. Department of Infectious Diseases, Huashan Hospital, Fudan University, 21 Shanghai, China 22 8. Sinovac Biotech Co., Ltd., Beijing, China NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. -

The Mississippi Covid-19 Vaccine Confidence Survey: Population Results Report
MAY 2021 THE MISSISSIPPI COVID-19 VACCINE CONFIDENCE SURVEY: POPULATION RESULTS Report A collaborative population-based study The Mississippi Community Engagement Alliance Against COVID-19 Disparities (CEAL) Team The Mississippi State Department of Health: Office of Preventive Health and Health Equity EXECUTIVE SUMMARY Since the Spring of 2020, the Novel 2019 Office of Preventive Health and Health Coronavirus (COVID-19) Pandemic has Equity (OPHHE) disseminated a statewide impacted Mississippians of every race, vaccine confidence survey beginning end ethnicity, age, gender, and income bracket. of December 2020 and collecting data Unfortunately, it has disproportionately until March 2021. The survey is intended to impacted Mississippians of color, the elderly, be representative of Mississippians, with and those living with chronic disease. For intentional efforts invested to reach lower most of the past year, the State has worked income and rural Mississippi populations, as to protect its population through preventive well as the state’s Black, Hispanic (Latino/ measures such as social distancing and Latinx), Asian (including the Vietnamese personal protective equipment. However, population of the Gulf Coast), and Native with the release of COVID-19 Vaccines to American/Choctaw communities. The sur- the public, the population of Mississippi has vey was administered in three languages- the opportunity to embrace a long-term English, Spanish, and Vietnamese- through a solution to COVID-19. That is, if Mississippians mixed-modal survey effort, including: web- are willing to receive the vaccine. To based, paper-based, and verbal-oratory assess Mississippians’ COVID-19 Vaccine administration. All targeted populations confidence, the Mississippi Community were ultimately reached and are represented Engagement Alliance Against COVID-19 in the over 11,000 completed responses Disparities (CEAL) Team and the Mississippi from all 82 of Mississippi’s counties.