Differential Diagnosis of Coronavirus Disease 2019 from Community
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

World Bank Document
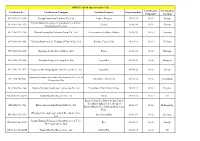
Project Name : Anhui Highway Maintenance Innovation and Demonstration Project Financed by the World Bank 、、、、、、、、、、、、、、、、、、、、、 Procurement Plan、、、、 Public Disclosure Authorized Date /、、、July 4, 2017/2017、7、4、 Thresholds for Procurement Method 、、、、、、 Description、、 Thresholds 、、 Works 、、/ S&I NCB、、、、、、、: <USD40,000,000.00 、、、、、、、 4000、、、、、、、、、、、、、、、、 Shopping、、、、: <USD500,000.00 、、、、、、、 50、、、、、、、、、、、、、 Goods 、、 NCB、、、、、、、、 <USD10,000,000.00 、、、、、、、 1000、、、、、、、、、、、、、、、、 Shopping、、、、: : <USD200,000.00、、、、、、、 20、、、、、、、、、、、、、 Consultant 、、 CQS、、、、、、、、、、、: <=USD300,000.00、、、、、、、 30、、、、、、、、、、、、、、、、、、、、 Public Disclosure Authorized Thresholds for Prior Review 、、、、 Description、、 Thresholds 、、 Works 、、/ S&I >=USD20,000,000.00; 、、、、、、、、、 2000、、、、、、、、、、、 Goods 、、 >=USD6,000,000.00; 、、、、、、、、、 600、、、、、、、、、、、 Consultant 、、 Firm being consultant、、、、: >=USD4,000,000.00; 、、、、、、、、、 400、、、、、、、、、、、、、、、、、、、、、 Individual being consultant、、、、:>=USD500,000.00、、、、、、、、、 50、、、、、、、、、、、、、、、、、、、、、 Public Disclosure Authorized Threshold for Shortlist Comprising Entirely national Consultants: <=USD500,000 or equivalent 、、、、、、、、、、、、、、、、、、、、、50、、、 Public Disclosure Authorized Project Name: Anhui Highway Maintenance Innovation and Demonstration Project Financed by the World Bank 、、、、: 、、、、、、、、、、、、、、、、 Procurement Plan 、、、、 Updated Date 、、、、、 2017.7.4 For Contracts For Contracts Not Signed Already Signed 、、、、、、、、、 、、、、、、、、、、 Cost Prior Contract Procurement Number Works/S&I/Goods/Consultants Estimate /Post Actual Remarks Number Contract Description 、、、、、、、、、、、、、、 Method Estimated -

A Miraculous Ningguo City of China and Analysis of Influencing Factors of Competitive Advantage
www.ccsenet.org/jgg Journal of Geography and Geology Vol. 3, No. 1; September 2011 A Miraculous Ningguo City of China and Analysis of Influencing Factors of Competitive Advantage Wei Shui Department of Eco-agriculture and Regional Development Sichuan Agricultural University, Chengdu Sichuan 611130, China & School of Geography and Planning Sun Yat-Sen University, Guangzhou 510275, China Tel: 86-158-2803-3646 E-mail: [email protected] Received: March 31, 2011 Accepted: April 14, 2011 doi:10.5539/jgg.v3n1p207 Abstract Ningguo City is a remote and small county in Anhui Province, China. It has created “Ningguo Miracle” since 1990s. Its general economic capacity has been ranked #1 (the first) among all the counties or cities in Anhui Province since 2000. In order to analyze the influencing factors of competitive advantages of Ningguo City and explain “Ningguo Miracle”, this article have evaluated, analyzed and classified the general economic competitiveness of 61 counties (cities) in Anhui Province in 2004, by 14 indexes of evaluation index system. The result showed that compared with other counties (cities) in Anhui Province, Ningguo City has more advantages in competition. The competitive advantage of Ningguo City is due to the productivities, the effect of the second industry and industry, and the investment of fixed assets. Then the influencing factors of Ningguo’s competitiveness in terms of productivity were analyzed with authoritative data since 1990 and a log linear regression model was established by stepwise regression method. The results demonstrated that the key influencing factor of Ningguo City’s competitive advantage was the change of industry structure, especially the change of manufacture structure. -

Update on Diagnosis and Treatment of Idiopathic Pulmonary Fibrosis
J Bras Pneumol. 2015;41(5):454-466 http://dx.doi.org/10.1590/S1806-37132015000000152 REVIEW ARTICLE Update on diagnosis and treatment of idiopathic pulmonary fibrosis José Baddini-Martinez1, Bruno Guedes Baldi2, Cláudia Henrique da Costa3, Sérgio Jezler4, Mariana Silva Lima5, Rogério Rufino3,6 1. Divisão de Pneumologia, Departamento de Clínica Médica, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo, Ribeirão Preto, Brasil. 2. Divisão de Pneumologia, Instituto do Coração, Hospital das Clínicas, ABSTRACT Faculdade de Medicina, Universidade de São Paulo, São Paulo, Brasil. Idiopathic pulmonary fibrosis is a type of chronic fibrosing interstitial pneumonia, of 3. Disciplina de Pneumologia e Tisiologia, unknown etiology, which is associated with a progressive decrease in pulmonary Faculdade de Ciências Médicas, function and with high mortality rates. Interest in and knowledge of this disorder have Universidade do Estado do Rio de grown substantially in recent years. In this review article, we broadly discuss distinct Janeiro, Rio de Janeiro, Brasil. aspects related to the diagnosis and treatment of idiopathic pulmonary fibrosis. We 4. Ambulatório de Pneumologia, Hospital list the current diagnostic criteria and describe the therapeutic approaches currently Ana Nery, Salvador, Brasil. available, symptomatic treatments, the action of new drugs that are effective in slowing 5. Ambulatório de Doenças Pulmonares Intersticiais, Hospital do Servidor the decline in pulmonary function, and indications for lung transplantation. Público Estadual de São Paulo, São Keywords: Idiopathic pulmonary fibrosis/diagnosis; Idiopathic pulmonary fibrosis/therapy; Paulo, Brasil. Idiopathic pulmonary fibrosis/rehabilitation. 6. Programa de Pós-Graduação em Ciências Médicas, Universidade do Estado do Rio de Janeiro, Rio de Janeiro, Brasil. -

Mantke, Peitz, Surgical Ultrasound -- Index
419 Index A esophageal 218 Anorchidism 376 gallbladder 165 Aorta 364–366 A-mode imaging 97 gastric 220 abdominal aneurysm (AAA) AAA (abdominal aortic aneurysm) metastasis 142 20–21, 364, 366 20–21, 364, 366 pancreatic 149, 225 dissection 364, 366 Abdominal wall Adenofibroma, breast 263 perforation 366 abscess 300–301 Adenoma pseudoaneurysm 364 diagnostic evaluation 297 adrenal 214 Aortic rupture 20 hematoma 73, 300, 305 colorectal 231, 232 Aplasia, muscular 272 rectus sheath 297–300 duodenal papilla 229, 231 Appendicitis 1–4 hernia 300, 302–304 gallbladder 165 consequences for surgical indications for sonography 297 hepatic 54, 58, 141 treatment 2 seroma 298, 300, 305 multiple 141 sonographic criteria 1 trauma 297–300 parathyroid 213 Archiving 418 Abortion, tubal 30 renal 241 Arteriosclerosis 346, 348 Abscess thyroid 202–203 carotid artery 335, 337, 338 abdominal wall 300–301 Adenomyomatosis 8, 164, 165 plaque 337, 338, 345, 367, 370 causes 301 Adrenal glands 214–216 Arteriovenous (AV) malformation amebic 138 adenoma 214 139, 293, 326–329 breast 264 carcinoma 214 Artery chest wall 173, 178 cyst 214 carotid 334–339 diverticular 120, 123 hematoma 214 aneurysm 338 drainage 85–88, 93 hemorrhage 214 arteriosclerosis 335 hepatic 6, 138, 398 hyperplasia 214 plaque characteristics inflammatory bowel disease limpoma/myelipoma 214 337, 338, 345 116, 119 metastases 214 bifurcation 334, 337 intramural 5 sonographic criteria 214 bulb 339 lung 183, 186, 190 tuberculosis 214 dissection 338, 339, 346 pancreatic 11 Advanced dynamic flow (ADF) sonographic -

Toxicological Profile for Jp-5, Jp-8, and Jet a Fuels
TOXICOLOGICAL PROFILE FOR JP-5, JP-8, AND JET A FUELS U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Agency for Toxic Substances and Disease Registry March 2017 JP-5, JP-8, AND JET A FUELS ii DISCLAIMER Use of trade names is for identification only and does not imply endorsement by the Agency for Toxic Substances and Disease Registry, the Public Health Service, or the U.S. Department of Health and Human Services. JP-5, JP-8, AND JET A FUELS iii UPDATE STATEMENT A Toxicological Profile for JP-5, JP-8, and Jet A Fuels, Draft for Public Comment was released in February 2016. This edition supersedes any previously released draft or final profile. Toxicological profiles are revised and republished as necessary. For information regarding the update status of previously released profiles, contact ATSDR at: Agency for Toxic Substances and Disease Registry Division of Toxicology and Human Health Sciences Environmental Toxicology Branch 1600 Clifton Road NE Mailstop F-57 Atlanta, Georgia 30329-4027 JP-5, JP-8, AND JET A FUELS iv This page is intentionally blank. JP-5, JP-8, AND JET A FUELS v FOREWORD This toxicological profile is prepared in accordance with guidelines* developed by the Agency for Toxic Substances and Disease Registry (ATSDR) and the Environmental Protection Agency (EPA). The original guidelines were published in the Federal Register on April 17, 1987. Each profile will be revised and republished as necessary. The ATSDR toxicological profile succinctly characterizes the toxicologic and adverse health effects information for these toxic substances described therein. Each peer-reviewed profile identifies and reviews the key literature that describes a substance's toxicologic properties. -

On the Local Political Economy of Rural Urbanisation in China, In: Journal of Current Chinese Affairs, 45, 1, 109–139
Journal of Current Chinese Affairs China aktuell Topical Issue: Policy Implementation in the New Socialist Countryside Guest Editor: René Trappel Meyer-Clement, Elena (2016), The Great Urban Leap? On the Local Political Economy of Rural Urbanisation in China, in: Journal of Current Chinese Affairs, 45, 1, 109–139. URN: http://nbn-resolving.org/urn/resolver.pl?urn:nbn:de:gbv:18-4-9488 ISSN: 1868-4874 (online), ISSN: 1868-1026 (print) The online version of this article and the other articles can be found at: <www.CurrentChineseAffairs.org> Published by GIGA German Institute of Global and Area Studies, Institute of Asian Studies and Hamburg University Press. The Journal of Current Chinese Affairs is an Open Access publication. It may be read, copied and distributed free of charge according to the conditions of the Creative Commons Attribution-No Derivative Works 3.0 License. To subscribe to the print edition: <[email protected]> For an e-mail alert please register at: <www.CurrentChineseAffairs.org> The Journal of Current Chinese Affairs is part of the GIGA Journal Family, which also includes Africa Spectrum, Journal of Current Southeast Asian Affairs and Journal of Politics in Latin America: <www.giga-journal-family.org>. Journal of Current Chinese Affairs 1/2016: 109–139 The Great Urban Leap? On the Local Political Economy of Rural Urbanisation in China Elena MEYER-CLEMENT Abstract: This paper provides insights into the local political econ- omy of China’s current in situ urbanisation as compared to the 1980s and 1990s, focusing on the role played by county and township gov- ernments in shaping urbanisation in their localities. -

Shop Direct Factory List Dec 18
Factory Factory Address Country Sector FTE No. workers % Male % Female ESSENTIAL CLOTHING LTD Akulichala, Sakashhor, Maddha Para, Kaliakor, Gazipur, Bangladesh BANGLADESH Garments 669 55% 45% NANTONG AIKE GARMENTS COMPANY LTD Group 14, Huanchi Village, Jiangan Town, Rugao City, Jaingsu Province, China CHINA Garments 159 22% 78% DEEKAY KNITWEARS LTD SF No. 229, Karaipudhur, Arulpuram, Palladam Road, Tirupur, 641605, Tamil Nadu, India INDIA Garments 129 57% 43% HD4U No. 8, Yijiang Road, Lianhang Economic Development Zone, Haining CHINA Home Textiles 98 45% 55% AIRSPRUNG BEDS LTD Canal Road, Canal Road Industrial Estate, Trowbridge, Wiltshire, BA14 8RQ, United Kingdom UK Furniture 398 83% 17% ASIAN LEATHERS LIMITED Asian House, E. M. Bypass, Kasba, Kolkata, 700017, India INDIA Accessories 978 77% 23% AMAN KNITTINGS LIMITED Nazimnagar, Hemayetpur, Savar, Dhaka, Bangladesh BANGLADESH Garments 1708 60% 30% V K FASHION LTD formerly STYLEWISE LTD Unit 5, 99 Bridge Road, Leicester, LE5 3LD, United Kingdom UK Garments 51 43% 57% AMAN GRAPHIC & DESIGN LTD. Najim Nagar, Hemayetpur, Savar, Dhaka, Bangladesh BANGLADESH Garments 3260 40% 60% WENZHOU SUNRISE INDUSTRIAL CO., LTD. Floor 2, 1 Building Qiangqiang Group, Shanghui Industrial Zone, Louqiao Street, Ouhai, Wenzhou, Zhejiang Province, China CHINA Accessories 716 58% 42% AMAZING EXPORTS CORPORATION - UNIT I Sf No. 105, Valayankadu, P. Vadugapal Ayam Post, Dharapuram Road, Palladam, 541664, India INDIA Garments 490 53% 47% ANDRA JEWELS LTD 7 Clive Avenue, Hastings, East Sussex, TN35 5LD, United Kingdom UK Accessories 68 CAVENDISH UPHOLSTERY LIMITED Mayfield Mill, Briercliffe Road, Chorley Lancashire PR6 0DA, United Kingdom UK Furniture 33 66% 34% FUZHOU BEST ART & CRAFTS CO., LTD No. 3 Building, Lifu Plastic, Nanshanyang Industrial Zone, Baisha Town, Minhou, Fuzhou, China CHINA Homewares 44 41% 59% HUAHONG HOLDING GROUP No. -

Climate Research 50:161
Vol. 50: 161–170, 2011 CLIMATE RESEARCH Published December 22 doi: 10.3354/cr01052 Clim Res Contribution to CR Special 28 ‘Changes in climatic extremes over mainland China’ OPENPEN ACCESSCCESS Historical analogues of the 2008 extreme snow event over Central and Southern China Zhixin Hao1, Jingyun Zheng1, Quansheng Ge1,*, Wei-Chyung Wang2 1Institute of Geographic Sciences and Natural Resources Research, Chinese Academy of Sciences, 11A Datun Road, Chaoyang District, Beijing 100101, PR China 2Atmospheric Sciences Research Center, State University of New York, Albany, New York 12203, USA ABSTRACT: We used weather records contained in Chinese historical documents from the past 500 yr to search for extreme snow events (ESEs) that were comparable in severity to an event in early 2008, when Central and Southern China experienced persistent heavy snowfall with unusu- ally low temperatures. ESEs can be divided into 3 groups according to the geographical coverage of snowfall, using the following criteria to define an ESE: >15 snowfall days, 20 snow-cover/icing days, and 30 cm total cumulated snow depth for an individual winter. The first group covers the whole of Eastern China (East of 105° E), and ESEs occurred in 1654, 1660, 1665, 1670, 1676, 1683, 1689, 1690, 1700, 1714, 1719, 1830−32, 1840, 1877 and 1892; the second group is located mainly in the area south of Huaihe River (~33° N), and ESEs occured in 1694, 1887, 1929, and 1930; and the third group is confined within the central region between Yellow River and Nanling Mountain (roughly 26° to 35° N), and ESEs occurred in 1578, 1620, 1796, and 1841. -

Table of Codes for Each Court of Each Level
Table of Codes for Each Court of Each Level Corresponding Type Chinese Court Region Court Name Administrative Name Code Code Area Supreme People’s Court 最高人民法院 最高法 Higher People's Court of 北京市高级人民 Beijing 京 110000 1 Beijing Municipality 法院 Municipality No. 1 Intermediate People's 北京市第一中级 京 01 2 Court of Beijing Municipality 人民法院 Shijingshan Shijingshan District People’s 北京市石景山区 京 0107 110107 District of Beijing 1 Court of Beijing Municipality 人民法院 Municipality Haidian District of Haidian District People’s 北京市海淀区人 京 0108 110108 Beijing 1 Court of Beijing Municipality 民法院 Municipality Mentougou Mentougou District People’s 北京市门头沟区 京 0109 110109 District of Beijing 1 Court of Beijing Municipality 人民法院 Municipality Changping Changping District People’s 北京市昌平区人 京 0114 110114 District of Beijing 1 Court of Beijing Municipality 民法院 Municipality Yanqing County People’s 延庆县人民法院 京 0229 110229 Yanqing County 1 Court No. 2 Intermediate People's 北京市第二中级 京 02 2 Court of Beijing Municipality 人民法院 Dongcheng Dongcheng District People’s 北京市东城区人 京 0101 110101 District of Beijing 1 Court of Beijing Municipality 民法院 Municipality Xicheng District Xicheng District People’s 北京市西城区人 京 0102 110102 of Beijing 1 Court of Beijing Municipality 民法院 Municipality Fengtai District of Fengtai District People’s 北京市丰台区人 京 0106 110106 Beijing 1 Court of Beijing Municipality 民法院 Municipality 1 Fangshan District Fangshan District People’s 北京市房山区人 京 0111 110111 of Beijing 1 Court of Beijing Municipality 民法院 Municipality Daxing District of Daxing District People’s 北京市大兴区人 京 0115 -

Annual Report 2019
HAITONG SECURITIES CO., LTD. 海通證券股份有限公司 Annual Report 2019 2019 年度報告 2019 年度報告 Annual Report CONTENTS Section I DEFINITIONS AND MATERIAL RISK WARNINGS 4 Section II COMPANY PROFILE AND KEY FINANCIAL INDICATORS 8 Section III SUMMARY OF THE COMPANY’S BUSINESS 25 Section IV REPORT OF THE BOARD OF DIRECTORS 33 Section V SIGNIFICANT EVENTS 85 Section VI CHANGES IN ORDINARY SHARES AND PARTICULARS ABOUT SHAREHOLDERS 123 Section VII PREFERENCE SHARES 134 Section VIII DIRECTORS, SUPERVISORS, SENIOR MANAGEMENT AND EMPLOYEES 135 Section IX CORPORATE GOVERNANCE 191 Section X CORPORATE BONDS 233 Section XI FINANCIAL REPORT 242 Section XII DOCUMENTS AVAILABLE FOR INSPECTION 243 Section XIII INFORMATION DISCLOSURES OF SECURITIES COMPANY 244 IMPORTANT NOTICE The Board, the Supervisory Committee, Directors, Supervisors and senior management of the Company warrant the truthfulness, accuracy and completeness of contents of this annual report (the “Report”) and that there is no false representation, misleading statement contained herein or material omission from this Report, for which they will assume joint and several liabilities. This Report was considered and approved at the seventh meeting of the seventh session of the Board. All the Directors of the Company attended the Board meeting. None of the Directors or Supervisors has made any objection to this Report. Deloitte Touche Tohmatsu (Deloitte Touche Tohmatsu and Deloitte Touche Tohmatsu Certified Public Accountants LLP (Special General Partnership)) have audited the annual financial reports of the Company prepared in accordance with PRC GAAP and IFRS respectively, and issued a standard and unqualified audit report of the Company. All financial data in this Report are denominated in RMB unless otherwise indicated. -
OFDC Certified Operators(2017-12) Certificate No.* Certification
OFDC Certified Operators(2017-12) Certification Certification Certificate No.* Certification Consigner Certified Products Expiration date Programs* Location OF-3102-932-1384 Jiangsu Lanshanhu Eco-farm Co., Ltd. Lettuce; Brassica 2018/1/29 01;02 Jiangsu Jiangxi Zhongda Ecological Agriculture Sci. & Tech. OF-3102-936-1259 Paddy 2018/1/4 01;02 Jiangxi Development Co., Ltd. OF-3104-925-1300 Dalian Haiyangdao Fisheries Group Co., Ltd. Sea cucumber; Scallop; Abalone 2018/1/8 01;02 Liaoning OF-3104-965-1440 Xinjiang Bositeng Lake Ecological Fishery Co., Ltd. Shrimp; Fishes; Crab 2018/1/18 01;02 Xinjiang OF-3104-965-1445 Xinjiang Aertai Glacier fish Co., Ltd. Fishes 2018/1/4 01;02 Xinjiang OF-3106-931-1200 Shanghai Tongchu Trading Co., Ltd. Vegetables 2018/1/2 01;02 Shanghai OF-3106-943-1973 Yongzhou Shennong Organic Farm Research Co., Ltd. Vegetables 2018/1/22 01;02 Hu'nan Quanxing Hanhua Agriculture Development Co., Ltd. of OF-3106-944-546 Vegetables; Strawberry 2018/1/14 01;02 Guangdong Guangzhou City OF-3106-964-1264 Ningxia Ninghua Landscape Engineering Co., Ltd. Vegetables; Plum; Peach; Grape 2018/1/12 01;02 Ningxia OF-3108-912-2645A Tianjin Hao Niu Bio-tech Co., Ltd. Alfalfa 2018/1/16 01;02 US Roasted Corn Tea; Roasted Corn Tassel Tea; Roasted Barley Tea; Steamed OP-3002-923-706 Harbin Organic Island Foodstuffs Co., Ltd. 2018/1/3 01;02 Heilongjiang Roasted Barley Tea; Soybean Meal; Corn Flake Zhejiang Qiancenglü Agricultural Development Co., OP-3002-933-1213 Dried osmanthus 2018/1/6 01;02 Zhejiang Ltd. Jiangxi Zhongda Ecological Agriculture Sci. -

Daily Life for the Common People of China, 1850 to 1950
Daily Life for the Common People of China, 1850 to 1950 Ronald Suleski - 978-90-04-36103-4 Downloaded from Brill.com04/05/2019 09:12:12AM via free access China Studies published for the institute for chinese studies, university of oxford Edited by Micah Muscolino (University of Oxford) volume 39 The titles published in this series are listed at brill.com/chs Ronald Suleski - 978-90-04-36103-4 Downloaded from Brill.com04/05/2019 09:12:12AM via free access Ronald Suleski - 978-90-04-36103-4 Downloaded from Brill.com04/05/2019 09:12:12AM via free access Ronald Suleski - 978-90-04-36103-4 Downloaded from Brill.com04/05/2019 09:12:12AM via free access Daily Life for the Common People of China, 1850 to 1950 Understanding Chaoben Culture By Ronald Suleski leiden | boston Ronald Suleski - 978-90-04-36103-4 Downloaded from Brill.com04/05/2019 09:12:12AM via free access This is an open access title distributed under the terms of the prevailing cc-by-nc License at the time of publication, which permits any non-commercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited. An electronic version of this book is freely available, thanks to the support of libraries working with Knowledge Unlatched. More information about the initiative can be found at www.knowledgeunlatched.org. Cover Image: Chaoben Covers. Photo by author. Library of Congress Cataloging-in-Publication Data Names: Suleski, Ronald Stanley, author. Title: Daily life for the common people of China, 1850 to 1950 : understanding Chaoben culture / By Ronald Suleski.