2014 Annual Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
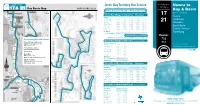
Jervis Bay Territory Bus Service Look for Bus Nowra to Numbers 17 & 21 Bus Route Map NOWRA COACHES Pty
LOOK FOR BUS Jervis Bay Territory Bus Service Look for bus Nowra to numbers 17 & 21 Bus Route Map NOWRA COACHES Pty. Ltd Transport initiative supplied by the Commonwealth of Australia and serviced by Nowra Coaches Bay & Basin Nowra Coaches Pty Ltd - Phone 4423 5244 Buses Servicing Wreck Bay Village to Vincentia – (Weekdays) 17 Departs Nowra Wreck Bay Village 6.25am 9.10am 11.10am 12.45pm 2.17pm Huskisson Summercloud Bay 6.30am 9.15am 11.15am 12.48pm 2.22pm 21 Green Patch 6.40am 9.25am 11.25am 12.58pm 2.32pm Vincentia Jervis Bay Village 6.47am 9.32am 11.32am 1.05pm 2.39pm HMAS Creswell 6.50am 9.35am 11.35am 1.08pm 2.42pm Bay & Basin Visitors Centre 6.55am 9.42am 11.41am 1.13pm 2.48pm Vincentia 7.08am 9.53am 11.51am 1.23pm 2.58pm Central Avenue Bus Departs Tomerong To Nowra (Via Huskisson) 7.10am 9.55am – 1.25pm** 3.00pm **Services Sanctuary Point, St. Georges Basin & Basin View only. Routes (Via Bay & Basin) – – 11.53am – 3.30pm Connecting Bus Operators 732 Wreck Bay Village to Vincentia – Saturday & Sunday Kennedy’s Bus and Coach Departs (Via Bay & Basin) 733 www.kennedystours.com.au See back cover for Tel: 1300 133 477 Wreck Bay Village 9.08am 1.20pm Summercloud Bay 9.13am 1.25pm detailed route descriptions Premier Motor Service Green Patch 9.23am 1.35pm www.premierms.com.au Jervis Bay Village 9.30am 1.42pm Price 50c Tel: 13 34 10 HMAS Creswell 9.33am 1.45pm Visitors Centre 9.38am 1.48pm Shoal Bus Tel: 02 4423 2122 Vincentia 9.48am 1.58pm Email: [email protected] Bus Departs To Nowra (Via Huskisson) 9.50am – Stuarts Coaches (Via -

Booderee National Park Management Plan 2015-2025
(THIS PAGE IS INTENTIONALLY BLANK – INSIDE FRONT COVER) Booderee National Park MANAGEMENT PLAN 2015- 2025 Management Plan 2015-2025 3 © Director of National Parks 2015 ISBN: 978-0-9807460-8-2 (Print) ISBN: 978-0-9807460-4-4 (Online) This plan is copyright. Apart from any use permitted under the Copyright Act 1968, no part may be reproduced by any process without prior written permission from the Director of National Parks. Requests and inquiries concerning reproduction and rights should be addressed to: Director of National Parks GPO Box 787 Canberra ACT 2601 This management plan sets out how it is proposed the park will be managed for the next ten years. A copy of this plan is available online at: environment.gov.au/topics/national-parks/parks-australia/publications. Photography: June Andersen, Jon Harris, Michael Nelson Front cover: Ngudjung Mothers by Ms V. E. Brown SNR © Ngudjung is the story for my painting. “It's about Women's Lore; it's about the connection of all things. It's about the seven sister dreaming, that is a story that governs our land and our universal connection to the dreaming. It is also about the connection to the ocean where our dreaming stories that come from the ocean life that feeds us, teaches us about survival, amongst the sea life. It is stories of mammals, whales and dolphins that hold sacred language codes to the universe. It is about our existence from the first sunrise to present day. We are caretakers of our mother, the land. It is in balance with the universe to maintain peace and harmony. -

Jervis Bay Territory Page 1 of 50 21-Jan-11 Species List for NRM Region (Blank), Jervis Bay Territory
Biodiversity Summary for NRM Regions Species List What is the summary for and where does it come from? This list has been produced by the Department of Sustainability, Environment, Water, Population and Communities (SEWPC) for the Natural Resource Management Spatial Information System. The list was produced using the AustralianAustralian Natural Natural Heritage Heritage Assessment Assessment Tool Tool (ANHAT), which analyses data from a range of plant and animal surveys and collections from across Australia to automatically generate a report for each NRM region. Data sources (Appendix 2) include national and state herbaria, museums, state governments, CSIRO, Birds Australia and a range of surveys conducted by or for DEWHA. For each family of plant and animal covered by ANHAT (Appendix 1), this document gives the number of species in the country and how many of them are found in the region. It also identifies species listed as Vulnerable, Critically Endangered, Endangered or Conservation Dependent under the EPBC Act. A biodiversity summary for this region is also available. For more information please see: www.environment.gov.au/heritage/anhat/index.html Limitations • ANHAT currently contains information on the distribution of over 30,000 Australian taxa. This includes all mammals, birds, reptiles, frogs and fish, 137 families of vascular plants (over 15,000 species) and a range of invertebrate groups. Groups notnot yet yet covered covered in inANHAT ANHAT are notnot included included in in the the list. list. • The data used come from authoritative sources, but they are not perfect. All species names have been confirmed as valid species names, but it is not possible to confirm all species locations. -

Agenda of Strategy and Assets Committee
Meeting Agenda Strategy and Assets Committee Meeting Date: Tuesday, 18 May, 2021 Location: Council Chambers, City Administrative Centre, Bridge Road, Nowra Time: 5.00pm Membership (Quorum - 5) Clr John Wells - Chairperson Clr Bob Proudfoot All Councillors Chief Executive Officer or nominee Please note: The proceedings of this meeting (including presentations, deputations and debate) will be webcast and may be recorded and broadcast under the provisions of the Code of Meeting Practice. Your attendance at this meeting is taken as consent to the possibility that your image and/or voice may be recorded and broadcast to the public. Agenda 1. Apologies / Leave of Absence 2. Confirmation of Minutes • Strategy and Assets Committee - 13 April 2021 ........................................................ 1 3. Declarations of Interest 4. Mayoral Minute 5. Deputations and Presentations 6. Notices of Motion / Questions on Notice Notices of Motion / Questions on Notice SA21.73 Notice of Motion - Creating a Dementia Friendly Shoalhaven ................... 23 SA21.74 Notice of Motion - Reconstruction and Sealing Hames Rd Parma ............. 25 SA21.75 Notice of Motion - Cost of Refurbishment of the Mayoral Office ................ 26 SA21.76 Notice of Motion - Madeira Vine Infestation Transport For NSW Land Berry ......................................................................................................... 27 SA21.77 Notice of Motion - Possible RAAF World War 2 Memorial ......................... 28 7. Reports CEO SA21.78 Application for Community -

Regional Overview
1 Regional Overview Population: 172,650 persons (2016 est. resident population) Growth Rate: 3.74% (2011 – 2016) 0.51% average annual growth Key Industries: Retail, Health Care and Social Assistance, Construction, Manufacturing, Defence, Tourism and Agriculture Number of Businesses by Industry – (top 10 shown) Construction 2484 Agriculture, forestry and fishing 1250 Rental, hiring and real estate services 1165 Retail trade 1101 Professional, scientific and technical services 989 Tourism 863 Financial and insurance services 647 Health care and social assistance 638 Transport, postal and warehousing 631 Other services 613 Total Businesses FSC (2014) 12,123 Council Areas: City of Shoalhaven, Eurobodalla Shire and Bega Valley Shire Location & Environment The Far South Coast (FSC) of NSW is a region covering 14,230sqkm of coastal land from Berry in the north to the NSW/ Victoria border in the south. 2 It is made up of three local government areas – Shoalhaven City, Eurobodalla Shire and Bega Valley Shire. The FSC is strategically located between the nation’s main capital cities, approximately 2-5 hours from Sydney, 6-10 hours from Melbourne and just 2 hours from Canberra. The FSC is renowned for its natural beauty with nearly 400 km of coastline; numerous marine parks, thirty one national park areas and extensive areas of state parks. The region generally has mild, pleasant weather. The summers are warm with an average maximum of 27°C while the winters generally have a minimum range from 1°C to 12°C. (Bureau of Meteorology). People & Community The estimated resident population of the FSC as at 30 June 2016 was 172,500 persons. -

5 Bunaan Close WRECK BAY JBT 2540
5 Bunaan Close WRECK BAY JBT 2540 Contents Introduction ................................................................................................................................................... 3 WBACC location ............................................................................................................................................. 4 Organisational Chart ..................................................................................................................................... 5 Purposes........................................................................................................................................................... 6 WBACC’s Vision .......................................................................................................................................... 6 WBACC’s Goals ........................................................................................................................................... 7 Provide more Housing and Improve Living Standards .................................................................. 7 Continue to maintain Good Governance Principles ......................................................................... 7 Obtain Sole Ownership of Land and Waters of Jervis Bay ........................................................ 8 Undertake Skills Analysis and Skills Training ................................................................................ 8 Implement New Management Structure ........................................................................................ -

Report of the House of Representatives Standing Committee on Environment and Conservation
THE PARLIAMENT OF THE COMMONWEALTH OF AUSTRALIA RELOCATION OF NAVAL FACILITIES TO JERVIS BAY Report of the House of Representatives Standing Committee on Environment and Conservation September 1986 W.1 V™ V ^•^ » ^^ Australian Government Publishing Serves Canberra 1986 *CM © Commonwealth of Australia 1986 ISBN 0 644 05487 5 Publisher's note: Parts of this publication have been reproduced from photocopies of original documents. Any loss of definition in reproduction quality is regretted. Printed by Authority by the Commonwealth Government Printer Terms of Reference of the Committee That a Standing Committee be appointed to inquire into and report on: (a) environmental aspects of legislative and administrative measures which ought to be taken in order to ensure the wise and effective management of the Australian environment and of Australia's natural resources; and (b) such other matters relating to the environment and conservation and the management of Australia's natural resources as are referred to it by - (i) the Minister responsible for those matters; or (ii) resolution of the House. Members of the Committee Chai rman Mr P. Milton, MP Deputy Chai rman Mr A.P. Webster, MP Members Mr R.L. Chynoweth, MP Mr R.F. Edwards, MP .Mr P.S. Fisher, MP Mr G. Gear, MP Ms J. McHugh, MP Mr C.G. Miles, MP Secretary to the Committee Mr J.R. Cummins Research staff Mr I. A. Dundas Mr R. I. Kropp CONTENTS Chapter Paragraph 1. Introduction 1 2. Jervis Bay Natural Features 11 Development 14 3. Naval Proposals Current Facilities 22 Relocation Proposals 25 Environmental Impact Studies 32 Comments on Proposals 40 4. -

Jervis Bay Marine Park Profile of Local Businesses
JERVIS BAY MARINE PARK PROFILE OF LOCAL BUSINESSES Department of Environment, Climate Change Prepared For: and Water Prepared By: Arche Consulting Pty Ltd Version: June 2010 Arche Consulting T + 61 0421 274076 Phillips Street Sydney NSW 2000 www.arche.com.au ABN 35 131 934 337 Disclaimer This report was prepared by Arche Consulting in good faith exercising all due care and attention, but no representation or warranty, express or implied, is made as to the relevance, accuracy, completeness or fitness for purpose of this document in respect of any particular user’s circumstances. Users of this document should satisfy themselves concerning its application to, and where necessary seek expert advice in respect of, their situation. The views expressed within are not necessarily the views of the Department of Environment, Climate Change and Water NSW (DECCW) and may not represent DECCW policy. © Copyright State of NSW and the Department of Environment, Climate Change and Water NSW ii Table of Contents 1 Introduction........................................................................................ 1 1.1 Overview...................................................................................... 1 1.2 The Marine Park ............................................................................. 1 2 Economic profile of the local region........................................................... 3 2.1 Overview of the local region .............................................................. 3 2.1.1 Overview ............................................................................... -

Find Your Local Brigade
Find your local brigade Find your district based on the map and list below. Each local brigade is then listed alphabetically according to district and relevant fire control centre. 10 33 34 29 7 27 12 31 30 44 20 4 18 24 35 8 15 19 25 13 5 3 45 21 6 2 14 9 32 23 1 22 43 41 39 16 42 36 38 26 17 40 37 28 11 NSW RFS Districts 1 Bland/Temora 13 Hawkesbury 24 Mid Coast 35 Orana 2 Blue Mountains 14 Hornsby 25 Mid Lachlan Valley 36 Riverina 3 Canobolas 15 Hunter Valley 26 Mid Murray 37 Riverina Highlands 4 Castlereagh 16 Illawarra 27 Mid North Coast 38 Shoalhaven 5 Central Coast 17 Lake George 28 Monaro 39 South West Slopes 6 Chifley Lithgow 18 Liverpool Range 29 Namoi Gwydir 40 Southern Border 7 Clarence Valley 19 Lower Hunter 30 New England 41 Southern Highlands 8 Cudgegong 20 Lower North Coast 31 North West 42 Southern Tablelands 9 Cumberland 21 Lower Western 32 Northern Beaches 43 Sutherland 10 Far North Coast 22 Macarthur 33 Northern Rivers 44 Tamworth 11 Far South Coast 23 MIA 34 Northern Tablelands 45 The Hills 12 Far West Find your local brigade 1 Find your local brigade 1 Bland/Temora Springdale Kings Plains – Blayney Tara – Bectric Lyndhurst – Blayney Bland FCC Thanowring Mandurama Alleena Millthorpe Back Creek – Bland 2 Blue Mountains Neville Barmedman Blue Mountains FCC Newbridge Bland Creek Bell Panuara – Burnt Yards Blow Clear – Wamboyne Blackheath / Mt Victoria Tallwood Calleen – Girral Blaxland Cabonne FCD Clear Ridge Blue Mtns Group Support Baldry Gubbata Bullaburra Bocobra Kikiora-Anona Faulconbridge Boomey Kildary Glenbrook -

WBACC Annual Report 2010 – 2011
Wreck Bay Aboriginal Community Council Annual Report 2010 –2011 Cover image: Mary’s Bay looking towards Summercloud Bay © Commonwealth of Australia 2010 ISSN 1832–5181 The contents of this Annual Report and Statement of Accounts are protected by the provisions of the Copyright Act, 1968. The document is produced solely for the purposes of reporting to its members and as required by law and the report or any part of this report must not be reproduced or published without the express written permission of the Wreck Bay Aboriginal Community Council. Address: Wreck Bay Aboriginal Community Council Administration Building 5 Bunaan Close WRECK BAY JBT 2540 Publisher: Wreck Bay Aboriginal Community Council Designer: LG2 designers www.lg2.com.au Wreck Bay Aboriginal Community Council Annual Report 2010–2011 iii iv Wreck Bay Aboriginal Community Council Annual Report 2010–2011 Contents Our Vision 1 Our Goals 1 Overview 2 Membership 3 Land Ownership/Management 7 Functions 8 Wreck Bay Village 9 Wreck Bay Community 9 Timeline 10 Board Members 16 Board Meetings 1st July 2010 to 30th June 2011 23 WBACC Annual Report 24 Chairman’s Report 25 The year in retrospect 25 Governance 25 Community Service 26 Land Management 27 Challenges moving forward 28 Chief Executive Officer’s Report 29 Funding Grants and other income 29 Subsidiary Companies and Contracts 30 Further Operational Activities with the Community 30 Compliance 31 The Future 31 Organisational Chart 33 WBACC Operations’ Report 34 Program Outcome Statement 34 Performance reporting 34 Administration -

Illawarra South Coast Regional Emergency Management Plan
Illawarra South Coast Regional Emergency Management Plan February 2019 11/awarra South Coast Regional Emergency Management Plan Part 1 -Administration Authority The lllawarra South Coast Regional Emergency Management Plan (EMPLAN) has been prepared by the lllawarra South Coast Regional Emergency Management Committee. The plan was approved by the Regional Emergency Operations Controller and endorsed by the State Emergency Management Committee in compliance with the State Emergency & Rescue Management Act 1989 on 6 December 2018. APPROVED Regional Emergency Operations Controller lllawarra South Coast Regional Emergency Management Committee Chair Dated: 6 September 2018 ENDORSED lllawarra South Coast Region EMPLAN 06 September 2018 Page2 Illawarra South Coast Regional Emergency Management Plan Document Control Version Author Review Primary Changes Date REMO 1.0 ISC REMC Initial Draft 2017 (W. Goodall) 1.1 REMO Review subcommittee Functional updates 2017 1.2 REMO ISC REMC Risk summary updates March 2018 1.3 REMO Final copy for approval Administrative updates August 2018 2.0 REMO ISC REMC Approved 6 Sep 2018 2.1 REMO State SES Administrative updates 13 Feb 2019 Illawarra South Coast Region EMPLAN 13 February 2019 v2.1 Page 3 Illawarra South Coast Regional Emergency Management Plan Contents Part 1 – Administration ................................................................................................................ 2 Authority ........................................................................................................................................... -

Water Sharing Plan for the Clyde River Unregulated and Alluvial Water Sources 2016
KEY TO EXTRACTION MANAGEMENT UNITS LOCALITY MAP NSW Jervis Bay Territory Legend Clyde Coastal Extraction Management Unit Clyde River Extraction Management Unit Buckenbowra River Extraction Management Unit Currambene Creek WOLLUMBOOLA LAKE *# at Falls Creek gauge (216004) WATER SOURCE CURRAMBENE CREEK WATER SOURCE PRINCES HWY ! HUSKISSON NORTH TOMERONG JERVIS BAY ! WATER SOURCE MoonaMOONA Moona Ck MOONA ST GEORGES BASIN CREEK WATER SOURCE WATER SOURCE ! GEORGES SOUTH JERVIS BAY YARD SANCTUARY POINT WATER SOURCE WANDANDIAN CREEK ! WATER SOURCE PRINCES HWY SUSSEX INLET Jervis Bay Territory SWAN LAKE ! WATER SOURCE BERRARA CREEK WATER SOURCE CONJOLA CREEK WATER SOURCE HILL TOP! NERRINDILLAH CREEK WATER SOURCE HOLLAND CREEK CONJOLA LAKE WATER SOURCE WATER SOURCE PIGEON HOUSE CREEK WATER SOURCE UPPER CLYDE RIVER NARRAWALLEE INLET WATER SOURCE WATER SOURCE MILTON ! YADBORO RIVER WATER SOURCE BOYNE CREEK WATER SOURCE ! ULLADULLA BURRILL LAKE WATER SOURCE Yadboro R Boyne Ck PRINCES HWY MORTON ! TABOURIE LAKE WATER SOURCE Clyde R *# TERMEIL LAKE WATER SOURCE Clyde River at Brooman gauge (216002) BIMBERAMALA RIVER MEROO LAKE WATER SOURCE WATER SOURCE ! MOGOOD MID CLYDE RIVER WATER SOURCE THE WESTERN DISTRIBUTOR WILLINGA LAKE WATER SOURCE Bimberamala R OLD PRINCES HWY KINGS HWY CURROWAN CREEK WATER SOURCE Cockwhy Ck KIOLOA WATER SOURCE COCKWHY CREEK WATER SOURCE Buckenbowra R DURRAS LAKE WATER SOURCE PRINCES HWY CYNE MALLOWES CREEK NELLIGEN CREEK KINGS HWY WATER SOURCE WATER SOURCE ! BUCKENBOWRA CLYDE ESTUARY TRIBUTARIES Legend WATER SOURCE Water Sharing Plan Boundary Buckenbowra River at Buckenbowra No.3 ! BATEMANS gauge (216009) Water Source Boundary QUART POT RD *# BAY Highly Connected Alluvium BUCKENBOWRA RIVER WATER SOURCE *# PRINCES HWY Gauging Station River Creek MOGO Tomaga R TOMAGA RIVER ! Water Body WATER SOURCE ! Town / Locality Highway Road CANDLAGAN CREEK WATER SOURCE PRINCES HWY Note: The rules in this Plan apply to all alluvial sediments, including mapped and unmapped alluvial sediments.