New Technologies for 211At Targeted Α-Therapy Research Using 211Rn and 209At
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lawrence Berkeley National Laboratory Recent Work
Lawrence Berkeley National Laboratory Recent Work Title PART A. AN X-RAY SPECTROMETER FOR USE IN RADIOACTIVITY MEASUREMENTS, THE L X- RAYS OF NEPTUNIUM AND PLUTONIUM. PART B. SOME LIGHTER ISOTOPES OF ASTATINE Permalink https://escholarship.org/uc/item/9ss952mr Author Barton, G.W. Publication Date 1950-05-02 eScholarship.org Powered by the California Digital Library University of California ·. l '; UCRL~67o · cy 2 UNIVERSITY OF CALIFORNIA TWO-WEEK LOAN COPY This is a Library Circulating Copy which may be borrowed for two weeks. For a personal retention copy, call Tech. Info. Division, Ext. 5545 BERKELEY, CALIFORNIA DISCLAIMER This document was prepared as an account of work sponsored by the United States Government. While this document is believed to contain correct information, neither the United States Government nor any agency thereof, nor the Regents of the University of California, nor any of their employees, makes any warranty, express or implied, or assumes any legal responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represents that its use would not infringe privately owned rights. Reference herein to any specific commercial product, process, or service by its trade name, trademark, manufacturer, or otherwise, does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States Government or any agency thereof, or the Regents of the University of California. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States Government or any agency thereof or the Regents of the University of California. • .\ UCRL-670 No Distribution II]ECLASSIF~ED UNIVERSITY OF CALIFORNIA Radiation Laboratory Contract No. -

Experimental Aspects of Geoneutrino Detection: Status and Perspectives
Experimental Aspects of Geoneutrino Detection: Status and Perspectives O. Smirnov,1 1JINR, Joint Institute for Nuclear Research, Dubna, Russian Federation October 22, 2019 Abstract Neutrino geophysics, the study of the Earth's interior by measuring the fluxes of geologically produced neutrino at its surface, is a new interdisciplinary field of science, rapidly developing as a synergy between geology, geophysics and particle physics. Geoneutrinos, antineutrinos from long- lived natural isotopes responsible for the radiogenic heat flux, provide valuable information for the chemical composition models of the Earth. The calculations of the expected geoneutrino signal are discussed, together with experimental aspects of geoneutrino detection, including the description of possible backgrounds and methods for their suppression. At present, only two detectors, Borexino and KamLAND, have reached sensitivity to the geoneutrino. The experiments accumulated a set of ∼190 geoneutrino events and continue the data acquisition. The detailed description of the experiments, their results on geoneutrino detection, and impact on geophysics are presented. The start of operation of other detectors sensitive to geoneutrinos is planned for the near future: the SNO+ detector is being filled with liquid scintillator, and the biggest ever 20 kt JUNO detector is under construction. A review of the physics potential of these experiments with respect to the geoneutrino studies, along with other proposals, is presented. New ideas and methods for geoneutrino detection are reviewed. Contents 1 Introduction 2 2 Geoneutrinos and the Earth's heat 4 2.1 Long-lived radiogenic elements . 4 2.2 Radiogenic heat and geoneutrino luminosity of the Earth . 9 arXiv:1910.09321v1 [physics.geo-ph] 21 Oct 2019 3 Geoneutrino flux calculation 11 3.1 Neutrino oscillations . -

Lawrence Berkeley National Laboratory Recent Work
Lawrence Berkeley National Laboratory Recent Work Title PRODUCTION AND DECAY PROPERTIES OF THORIUM ISOTOPES OF MASS 221-224 FORMED IN HEAVY ION REACTIONS Permalink https://escholarship.org/uc/item/9bp2f39g Authors Valli, Kalevi Hyde, Earl K. Borggreen, Jorn. Publication Date 1969-10-01 eScholarship.org Powered by the California Digital Library University of California Submitted to Physical Review UCRL-18992 Preprint ,. 2 "'--' Ht:::.cE.l'VED l'VJRENCE RAD\AliOI'l lABORAlOR'l tEt3 Z6 1970 ..,. , L\BRARY AND N ""NTS sE.CTlO .1 0 ocut'J\r;;.. PRODUCTION AND DECAY PROPERTIES OF THORIUM ISOTOPES p• OF MASS 221-224 FORMED IN HEAVY ION REACTIONS Kalevi Valli, Earl K. Hyde, and Jprn Borggreen October 1969 AEC Contract No. W -7405-eng-48 TWO-WEEK LOAN COPY This is a library Circulating Copy which may be borrowed for two weeks. For a personal retention copy, call ··~~. Tech. Info. Division, Ext. 5545 ,.... -< () LAWRENCE RADIATION LABORATOR~ Z ~0~ UNI,1ERSI'"fY of C:AJ_.JIF'()RNIA BEllKELEry rt ·oce ' ' DISCLAIMER This document was prepared as an account of work sponsored by the United States Government. While this document is believed to contain coiTect information, neither the United States Government nor any agency thereof, nor the Regents of the University of California, nor any of their employees, makes any waiTanty, express or implied, or assumes any legal responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represents that its use would not infringe privately owned rights. Reference herein to any specific commercial product, process, or service by its trade name, trademark, manufacturer, or otherwise, does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States Government or any agency thereof, or the Regents of the University of California. -

ASTATINE Element Symbol: at Atomic Number: 85
ASTATINE Element Symbol: At Atomic Number: 85 An initiative of IYC 2011 brought to you by the RACI LINDA ABBLITT www.raci.org.au ASTATINE Element symbol: At Atomic number: 85 Astatine is a highly radioactive chemical element. It is chemically similar to the other halogens above it in Group 17 of the periodic table. It is the heaviest known halogen. As chemists would expect, Astatine acts more like a metal than iodine, the element just above it in the table. Astatine is produced by radioactive decay in nature, but due to its short half-life it is found only in minute amounts. It is currently the rarest naturally occurring element, with less than 30 grams estimated to be contained in the entire Earth’s crust. This amounts to less than one teaspoon of the element. Isaac Asimov in a 1957 essay on large numbers, scientific notation and the size of the atom, wrote that in “all of North and South America to a depth of ten miles”, the number of astatine-215 atoms at any time is “only a trillion”. Guinness Book of Records lists it as the rarest element. It is found near thorium and uranium in the Earth’s crust. Astatine would be expected to be a nearly black solid, which, when heated, sublimes into a dark, purplish vapor (darker than iodine) Astatine (after Greek astatos meaning unstable) was first synthesized in 1940 by Dale R Corson, Kenneth Ross MacKenzie an Emilio Segrè at the University of California, Berkeley by bombarding bismuth with alpha particles in a cyclotron. -

Exploration of Astatine Chemistry in Solution : Focus on the Pourbaix Diagram in Noncomplexing Medium and Characterization of Astatine-Mediated Halogen Bonds Lu Liu
Exploration of astatine chemistry in solution : focus on the Pourbaix diagram in noncomplexing medium and characterization of astatine-mediated halogen bonds Lu Liu To cite this version: Lu Liu. Exploration of astatine chemistry in solution : focus on the Pourbaix diagram in noncom- plexing medium and characterization of astatine-mediated halogen bonds. Radiochemistry. Ecole na- tionale supérieure Mines-Télécom Atlantique, 2020. English. NNT : 2020IMTA0205. tel-03123005 HAL Id: tel-03123005 https://tel.archives-ouvertes.fr/tel-03123005 Submitted on 27 Jan 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. THESE DE DOCTORAT DE L’ÉCOLE NATIONALE SUPERIEURE MINES-TELECOM ATLANTIQUE BRETAGNE PAYS DE LA LOIRE - IMT ATLANTIQUE ECOLE DOCTORALE N° 596 Matière, Molécules, Matériaux Spécialité : Chimie Analytique et Radiochimie Par Lu LIU Exploration de la chimie de l'astate en solution : Focalisation sur le diagramme de Pourbaix en milieu non complexant et caractérisation de liaisons halogènes induites par l'astate Thèse présentée et soutenue à Nantes, -

INTC Minutes
CERN-INTC-2013-018 INTC-044 July 22, 2013 ISOLDE AND NEUTRON TIME-OF-FLIGHT EXPERIMENTS COMMITTEE Minutes of the 44th meeting of the INTC held on Wednesday, June 26, and Thursday, June 27, 2013 OPEN SESSION Wednesday, June 26, 2013 at 11:00 in the Council Chamber. The chairman of the INTC, Klaus Blaum, opened the meeting, presented all members of the committee and announced the agenda. ISOLDE Technical Report The ISOLDE Technical Coordinator, Richard Catherall, made a summary of the works going on during the Long Shutdown period (LS1). The civil engineering in the ISOLDE hall (wall and new trench cutting) was described as well as the status of new buildings 198 and 199 for the HIE-ISOLDE services and the idea of a new building 508. The most important points concerning the ISOLDE machine were listed, which included the upgrade of robots in the target area, extension of the RILIS room, RFQ cooler alignment, and the EBIS upgrade. New developments in the targets and ion sources were also presented. Finally, the Medicis project was briefly introduced. Following the favourable safety review completed recently, the ground works will start in the beginning of July. It was announced that the HIE-ISOLDE workshop will be held on 28th - 29th November 2013 just after the ISOLDE workshop. ISOLDE Physics Report On behalf of the ISOLDE Physics Coordinator, Magdalena Kowalska, Marek Pfützner presented the summary of the year 2012, the current shift balance, and briefly listed research activities at ISOLDE between the last INTC meeting in October/November and the end of physics programme on December 17, 2012. -
Cyclotron Produced Radionuclides: Principles and Practice
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/293816645 Cyclotron Produced Radionuclides: Principles and Practice Book · December 2008 CITATIONS READS 11 4,895 14 authors, including: Mohammad Haji-Saeid Pillai Mra International Atomic Energy Agency (IAEA) Molecular Global Group 69 PUBLICATIONS 1,127 CITATIONS 206 PUBLICATIONS 3,912 CITATIONS SEE PROFILE SEE PROFILE Thomas J Ruth Jožef J. Čomor TRIUMF ELEX Commerce d.o.o. 396 PUBLICATIONS 14,205 CITATIONS 66 PUBLICATIONS 668 CITATIONS SEE PROFILE SEE PROFILE Some of the authors of this publication are also working on these related projects: Radiopharmaceuticals View project The Extraction of Negative Carbon Ions from a Volume Cusp Ion Source View project All content following this page was uploaded by Pillai Mra on 17 January 2018. The user has requested enhancement of the downloaded file. Cyclotron Produced Isotopes: Principles and Practice XXXX 2007 The originating Section of this publication in the IAEA was: Industrial Applications and Chemistry Section International Atomic Energy Agency Wagramer Strasse 5 P.O. Box 100 A-1400 Vienna, Austria Theory and Practice of Radioisotope Production Using Cyclotrons IAEA, VIENNA, 2007 IAEA-TRS-xxxx ISSN 1011–4289 © IAEA, 2007 Printed by the IAEA in Austria XXXX 2007 FOREWORD Application of radioisotopes has shown a significant growth in the last decade and one of the major factors contributing towards this increased growth is the availability of a large number of cyclotrons exclusively dedicated to the production of radioisotopes for medical applications. As per a recent IAEA survey, it is estimated that there are more than 350 cyclotrons available in the Member States (MS) [Directory of Cyclotrons Used for Radionuclide Production in Member States, IAEA- DCRP/2006]. -
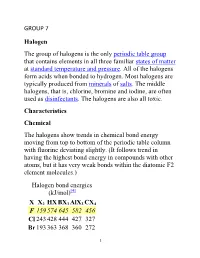
GROUP 7 Halogen the Group of Halogens Is the Only Periodic Table
GROUP 7 Halogen The group of halogens is the only periodic table group that contains elements in all three familiar states of matter at standard temperature and pressure. All of the halogens form acids when bonded to hydrogen. Most halogens are typically produced from minerals of salts. The middle halogens, that is, chlorine, bromine and iodine, are often used as disinfectants. The halogens are also all toxic. Characteristics Chemical The halogens show trends in chemical bond energy moving from top to bottom of the periodic table column with fluorine deviating slightly. (It follows trend in having the highest bond energy in compounds with other atoms, but it has very weak bonds within the diatomic F2 element molecules.) Halogen bond energies (kJ/mol)[4] X X2 HX BX3 AlX3 CX4 F 159 574 645 582 456 Cl 243 428 444 427 327 Br 193 363 368 360 272 1 I 151 294 272 285 239 Halogens are highly reactive, and as such can be harmful or lethal to biological organisms in sufficient quantities. This high reactivity is due to the high electronegativity of the atoms due to their high effective nuclear charge. They can gain an electron by reacting with atoms of other elements. Fluorine is one of the most reactive elements in existence, attacking otherwise-inert materials such as glass, and forming compounds with the heavier noble gases. It is a corrosive and highly toxic gas. The reactivity of fluorine is such that, if used or stored in laboratory glassware, it can react with glass in the presence of small amounts of water to form silicon tetrafluoride (SiF4). -

Astatine Production in a Lead-Bismuth Target Bombarded by a Proton Beam
DOI: 10.15669/pnst.4.486 Progress in Nuclear Science and Technology Volume 4 (2014) pp. 486-490 ARTICLE Astatine production in a lead-bismuth target bombarded by a proton beam: a detailed study using INCL4.6-Abla07 Jean-Christophe Davida, Alain Boudarda, Joseph Cugnonb, Salim Ghalia, Sylvie Leraya*, Davide Mancusia and Luca Zaninic aCEA/Saclay, IRFU/SPhN, 91191 Gif-sur-Yvette Cedex, France; bUniversity of Liège, AGO Department, allée du 6 août 17, Bât. B5, B-4000 Liège 1, Belgium; cPSI, Zurich, Switzerland Liquid lead-bismuth eutectic (LBE) is often considered as a possible target in spallation neutron sources. An experiment has been performed in 2005 at ISOLDE (CERN), in which LBE has been irradiated by 1.0 and 1.4 GeV protons and isotopes of astatine, a volatile precursor of Po, have been found. Until recently no model was able to reproduce this astatine production, which is due either to double charge exchange reactions, Bi(p,π-xn)At, or to secondary reactions induced by helium nuclei. Recently, both parts of the spallation model combination INCL4-Abla have been improved leading to the new versions, INCL4.6-ABLA07. In particular, an additional mechanism to produce light and intermediate mass fragments has been added and special care has been paid to the low energy reactions. This paper first shows that all the basic features of the different reactions leading to astatine production are well predicted by the new model. The model, implemented into a beta version of MCNPX2.7 is then used to simulate the ISOLDE experiment. A very good agreement with the experimental data is observed. -

Indication for a Volatile Element 114
Radiochim. Acta 98, 133–139 (2010) / DOI 10.1524/ract.2010.1705 © by Oldenbourg Wissenschaftsverlag, München Indication for a volatile element 114 By R. Eichler1,2,∗,N.V.Aksenov3, Yu. V. Albin3, A. V. Belozerov3 ,G.A.Bozhikov3, V. I. Chepigin3 , S. N. Dmitriev3, R. Dressler1,H.W.Gäggeler1 ,2, V. A. Gorshkov3, R. A. Henderson4, A. M. Johnsen4,J.M.Kenneally4 , V. Ya. Lebedev3, O. N. Malyshev3, K. J. Moody4, Yu. Ts. Oganessian3,O.V.Petrushkin3, D. Piguet1,A.G.Popeko3, P. Rasmussen1, A. Serov1,2, D. A. Shaughnessy4, S. V. Shishkin3, A. V. Shutov3,M.A.Stoyer4,N.J.Stoyer4, A. I. Svirikhin3, E. E. Tereshatov3, G. K. Vostokin3, M. Wegrzecki5 , P. A. Wilk4, D. Wittwer2 and A. V. Yeremin3 1 Labor für Radio- und Umweltchemie, Paul Scherrer Institut, 5232 Villigen, Switzerland 2 Departement für Chemie und Biochemie, Universität Bern, 3012 Bern, Switzerland 3 Flerov Laboratory of Nuclear Reactions, Joint Institute for Nuclear Research, 141980 Dubna, Russia 4 Lawrence Livermore National Laboratory, Livermore, CA 94551, USA 5 Insitute of Electron Technology, 02-668 Warsaw, Poland (Received June 30, 2009; accepted in revised form November 2, 2009) Transactinides / Element 114 / Adsorption / into group 14 together with carbon, silicon, germanium, Thermochromatography tin, and lead. The enhancement of the metallic character with increasing atomic number Z is an obvious trend ob- served along the main groups 13–17 of the periodic table. Summary. Recently, the chemical investigation of element Thus, a metallic character can be expected for element 112 revealed a highly volatile, noble metallic behaviour, as 114 [9, 10]. However, relativistic calculations of the elec- expected for the last group 12 member of the periodic table. -

Indication for a Volatile Element 114 135
Radiochim. Acta 98, 133–139 (2010) / DOI 10.1524/ract.2010.1705 © by Oldenbourg Wissenschaftsverlag, München Indication for a volatile element 114 By R. Eichler1,2,∗,N.V.Aksenov3, Yu. V. Albin3, A. V. Belozerov3 ,G.A.Bozhikov3, V. I. Chepigin3 , S. N. Dmitriev3, R. Dressler1,H.W.Gäggeler1 ,2, V. A. Gorshkov3, R. A. Henderson4, A. M. Johnsen4,J.M.Kenneally4 , V. Ya. Lebedev3, O. N. Malyshev3, K. J. Moody4, Yu. Ts. Oganessian3,O.V.Petrushkin3, D. Piguet1,A.G.Popeko3, P. Rasmussen1, A. Serov1,2, D. A. Shaughnessy4, S. V. Shishkin3, A. V. Shutov3,M.A.Stoyer4,N.J.Stoyer4, A. I. Svirikhin3, E. E. Tereshatov3, G. K. Vostokin3, M. Wegrzecki5 , P. A. Wilk4, D. Wittwer2 and A. V. Yeremin3 1 Labor für Radio- und Umweltchemie, Paul Scherrer Institut, 5232 Villigen, Switzerland 2 Departement für Chemie und Biochemie, Universität Bern, 3012 Bern, Switzerland 3 Flerov Laboratory of Nuclear Reactions, Joint Institute for Nuclear Research, 141980 Dubna, Russia 4 Lawrence Livermore National Laboratory, Livermore, CA 94551, USA 5 Insitute of Electron Technology, 02-668 Warsaw, Poland (Received June 30, 2009; accepted in revised form November 2, 2009) Transactinides / Element 114 / Adsorption / into group 14 together with carbon, silicon, germanium, Thermochromatography tin, and lead. The enhancement of the metallic character with increasing atomic number Z is an obvious trend ob- served along the main groups 13–17 of the periodic table. Summary. Recently, the chemical investigation of element Thus, a metallic character can be expected for element 112 revealed a highly volatile, noble metallic behaviour, as 114 [9, 10]. However, relativistic calculations of the elec- expected for the last group 12 member of the periodic table. -
Inverse Odd-Even Staggering in Nuclear Charge Radii and Possible Octupole Collectivity in $\Sideset{^{217218219}}
PHYSICAL REVIEW C 99, 054317 (2019) Inverse odd-even staggering in nuclear charge radii and possible octupole collectivity in 217,218,219At revealed by in-source laser spectroscopy A. E. Barzakh,1,* J. G. Cubiss,2 A. N. Andreyev,2,3,4 M. D. Seliverstov,1,2 B. Andel,5 S. Antalic,5 P. Ascher,6 D. Atanasov,6 D. Beck,7 J. Bieron,´ 8 K. Blaum,6 Ch. Borgmann,6 M. Breitenfeldt,9 L. Capponi,10 T. E. Cocolios,4,11 T. Day Goodacre,4,11 X. Derkx,10,12 H. De Witte,9 J. Elseviers,9 D. V. Fedorov,1 V. N. Fedosseev,4 S. Fritzsche,13,14 L. P. Gaffney,9 S. George,6 L. Ghys,9,15 F. P. Heßberger,16,17 M. Huyse,9 N. Imai,4,18 Z. Kalaninová,5,19 D. Kisler,6 U. Köster,20 M. Kowalska,4 S. Kreim,6,4 J. F. W. Lane,10 V. Liberati,10 D. Lunney,21 K. M. Lynch,4,11 V. Manea,4,21 B. A. Marsh,4 S. Mitsuoka,3 P. L. Molkanov,1 Y. Nagame,3 D. Neidherr,7 K. Nishio,3 S. Ota,3 D. Pauwels,15 L. Popescu,15 D. Radulov,9 E. Rapisarda,4 J. P. Revill,22 M. Rosenbusch,23,24 R. E. Rossel,4,25 S. Rothe,4,25 K. Sandhu,10 L. Schweikhard,23 S. Sels,9 V. L. Truesdale,2 C. Van Beveren,9 P. Van den Bergh,9 P. Van Duppen,9 Y. Wakabayashi,3 K. D. A. Wendt,25 F. Wienholtz,23,4 B.