Emergencies Preparedness, Response Monkeypox – Democratic Republic of the Congo
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Poxvirus and Rabies Branch (PRB) Fact Sheet
Poxvirus & Rabies Branch (PRB) The epidemiologists, laboratory scientists, and public health professionals in PRB are responsible for surveillance, control, and prevention of illness and death due to poxviruses and rabies. Our Work Laboratory Reference, Diagnostics, & Training PRB’s provides laboratory reference, diagnostic services, and trainings to state and local health departments, the Department of Defense (DOD), international organizations, and the Laboratory Response Network (over 150 labs across the U.S. prepared to respond to bioterrorism). PRB collaborates with the private sector to develop and evaluate novel diagnostic assays, therapeutics, and vaccines for rabies and pox-related viruses. The branch maintains high-containment laboratories (BSL3 &4) to safely conduct public health research. Research & Surveillance PRB conducts research studies on the microbiology, molecular biology, pathogenesis (disease process), ecology, and evolution of Our Pathogens poxviruses and rabies. The branch monitors the incidence rates of PRB’s Poxvirus Team provides subject matter these diseases in the U.S. and internationally. expertise on: Expert Consultation Orthopoxviruses, including PRB provides consultation regarding poxvirus and rabies- Smallpox associated diseases and their diagnoses, prevention, control, and Monkeypox treatments. Assistance is offered to healthcare providers, academic Cowpox institutions, state and local health departments, other government Vaccinia Virus agencies, and the general public. PRB collaborates with non- governmental organizations to develop risk communication Parapoxviruses, including tools for disease prevention. The branch provides training on Orf Virus simple surveillance techniques and trains healthcare workers on monkeypox in the Democratic Republic of the Congo (DRC). PRB Pseudocowpox collaborates with the national government of Haiti on a rabies surveillance and control program which includes health education, enhanced diagnostics, surveillance, and an extensive dog vaccination campaign. -

MONUSCO, 20 Years in Democratic Republic of Congo. What
MONUSCO, 20 Years in Democratic Republic of Congo. What Are the Priorities For Its New Mandate? Analysis December 2019 / N° 746a Cover picture: The gates to the MONUSCO headquarters in Kinshasa, Democratic Republic of Congo (DRC), 19 February 2015. © Michael Kappeler / DPA/DPA Picture Alliance TABLE OF CONTENTS ACRONYMS 5 MAP OF MONUSCO’S PRESENCE IN DRC 6 EXECUTIVE SUMMARY 7 METHODOLOGY 9 INTRODUCTION 10 I. OVERVIEW OF THE POLITICAL, SECURITY AND HUMAN RIGHTS CONTEXT IN DRC 12 A. An uncertain context of emergence from political crisis and lifting of restrictions on democratic space 12 B. A worrying security context, marked by continuing violations of human rights and inter-communal tensions and conflicts throughout the country 14 II. OVERVIEW OF THE CONTEXT OF RENEWAL OF MONUSCO’S MANDATE 18 A. A nine-month interim mandate 18 B. Towards MONUSCO’s reconfiguration 19 III. PRIORITIES FOR THE NEW MONUSCO MANDATE ACCORDING TO FIDH AND ITS MEMBER ORGANISATIONS IN DRC 21 A. On democratic space and governance 21 1. Consolidate efforts already undertaken to open up democratic space 21 2. Encourage institutional reforms 22 B. On security and civilian protection 24 1. Prioritise a non-military community-based and local approach to civilian protection 24 2. Strengthen civil and military coordination 25 3. Provide a rapid response to protection needs 26 4. Adopt a regional approach to civilian protection 26 5. Pursue efforts to reform the UN peacekeeping system 26 C. On justice and the fight against impunity 27 1. Fight impunity for the most serious crimes 27 2. Build the capacities of the judicial system to increase its efficiency and independence 29 3. -

Dengue Fever in Senegal 6 - 7 Ongoing Events Ebola Virus Disease in the Democratic Republic of the Congo Humanitarian Crisis in Cameroon
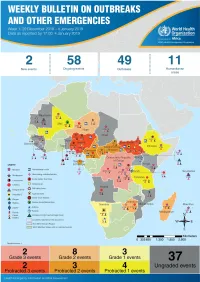
Overview Contents This Weekly Bulletin focuses on selected acute public health emergencies occurring in the WHO African Region. The WHO Health Emergencies Programme is currently monitoring 58 events in the region. This week’s edition covers key new and ongoing events, including: 2 Overview Hepatitis E in Central African Republic 3 - 5 New events Monkeypox in Central African Republic Dengue fever in Senegal 6 - 7 Ongoing events Ebola virus disease in the Democratic Republic of the Congo Humanitarian crisis in Cameroon. 8 Summary of major issues challenges and For each of these events, a brief description, followed by public health proposed actions measures implemented and an interpretation of the situation is provided. 9 All events currently A table is provided at the end of the bulletin with information on all new and being monitored ongoing public health events currently being monitored in the region, as well as events that have recently been closed. Major issues and challenges include: The Ebola virus disease (EVD) outbreak in the Democratic Republic of the Congo has reached a critical juncture, marked by a precarious security situation, persistence of pockets of community resistance/ mistrust and expanding geographical spread of the disease. During the reporting week, there was an incident involving a response team performing burial activity in Butembo. This came barely days following a widespread community strike (“ville morte”) in Beni and several towns, and an earlier armed attack in Beni. These incidents severely disrupted most outbreak control interventions. Meanwhile, EVD cases have been confirmed in new areas with worse insecurity and in close proximity to the border with Uganda. -

Imported Monkeypox, Singapore
DISPATCHES Imported Monkeypox, Singapore Sarah Ee Fang Yong, Oon Tek Ng, Zheng Jie Marc Ho, Tze Minn Mak, Kalisvar Marimuthu, Shawn Vasoo, Tsin Wen Yeo, Yi Kai Ng, Lin Cui, Zannatul Ferdous, Po Ying Chia, Bryan Jun Wei Aw, Charmaine Malenab Manauis, Constance Khia Ki Low, Guanhao Chan, Xinyi Peh, Poh Lian Lim, Li Ping Angela Chow, Monica Chan, Vernon Jian Ming Lee, Raymond Tzer Pin Lin, Mok Kwee Derrick Heng, Yee Sin Leo In May 2019, we investigated monkeypox in a traveler and public health management for this case, together from Nigeria to Singapore. The public health response with lessons learned and implications for control. included rapid identification of contacts, use of quaran- tine, and postexposure smallpox vaccination. No sec- The Case ondary cases were identified. Countries should develop On May 8, 2019, monkeypox was laboratory-con- surveillance systems to detect emerging infectious dis- firmed in a 38-year-old man from Nigeria who had eases globally. traveled to Singapore. The man resided in Delta State, Nigeria, but had attended a wedding in Ebonyi State onkeypox is a zoonosis endemic to West and during April 21–23, where he reported ingestion of MCentral Africa; human cases were first report- barbecued bushmeat that might have been contami- ed in 1970 (1). An outbreak ongoing in Nigeria since nated. He did not handle raw meat and had no expo- 2017 is the largest documented (2). Exported cases in sure to wild animals or their products. He held an ad- the United Kingdom and Israel were reported from ministrative job and reported no contact with rodents travelers infected in Nigeria in 2018 (3,4). -

To Ebola Reston
WHO/HSE/EPR/2009.2 WHO experts consultation on Ebola Reston pathogenicity in humans Geneva, Switzerland 1 April 2009 EPIDEMIC AND PANDEMIC ALERT AND RESPONSE WHO experts consultation on Ebola Reston pathogenicity in humans Geneva, Switzerland 1 April 2009 © World Health Organization 2009 All rights reserved. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distin- guished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either express or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use. This publication contains the collective views of an international group of experts and does not necessarily represent the decisions or the policies of the World Health Organization. -
Weekly Bulletin on Outbreaks
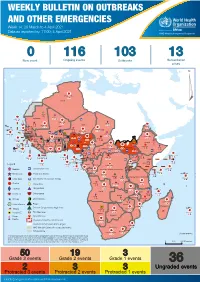
WEEKLY BULLETIN ON OUTBREAKS AND OTHER EMERGENCIES Week 14: 29 March to 4 April 2021 Data as reported by: 17:00; 4 April 2021 REGIONAL OFFICE FOR Africa WHO Health Emergencies Programme 0 116 103 13 New event Ongoing events Outbreaks Humanitarian crises 117 622 3 105 Algeria ¤ 36 13 110 0 5 420 164 Mauritania 7 2 10 501 392 110 0 7 0 Niger 17 927 449 Mali 3 334 10 567 0 6 0 2 079 4 4 595 165 Eritrea Cape Verde 38 520 1 037 Chad Senegal 4 918 185 59 0 Gambia 27 0 3 0 17 125 159 9 761 45 Guinea-Bissau 796 17 7 0 Burkina Faso 225 46 215 189 2 963 0 162 593 2 048 Guinea 12 817 150 12 38 397 1 3 662 66 1 1 23 12 Benin 30 0 Nigeria 1 873 71 0 Ethiopia 420 14 481 5 6 188 15 Sierra Leone Togo 3 473 296 53 920 779 52 14 Ghana 5 245 72 Côte d'Ivoire 10 098 108 14 484 479 63 0 40 0 Liberia 17 0 South Sudan Central African Republic 916 2 45 0 25 0 19 670 120 43 180 237 90 287 740 Cameroon 7 0 28 676 137 5 330 13 138 988 2 224 1 952 87 655 2 51 22 43 0 112 12 6 1 488 6 3 988 79 11 187 6 902 102 Equatorial Guinea Uganda 542 8 Sao Tome and Principe 32 11 2 042 85 41 016 335 Kenya Legend 7 100 90 Gabon Congo 18 504 301 Rwanda Humanitarian crisis 2 212 34 22 482 311 Measles 18 777 111 Democratic Republic of the Congo 9 681 135 Burundi 2 964 6 Monkeypox Ebola virus disease Seychelles 27 930 739 1 525 0 420 29 United Republic of Tanzania Lassa fever Skin disease of unknown etiology 189 0 4 084 20 509 21 Cholera Yellow fever 1 349 5 6 257 229 22 631 542 cVDPV2 Dengue fever 88 930 1 220 Comoros Angola Malawi COVID-19 Chikungunya 33 661 1 123 862 0 3 719 146 -

Ebola Virus Disease and Clinical Care Part I: History, Transmission, and Clinical Presentation
Ebola Virus Disease and Clinical Care Part I: History, Transmission, and Clinical Presentation This lecture is on Ebola virus disease (EVD) and clinical care. This is part one of a three-part lecture on this topic. Preparing Healthcare Workers to Work in Ebola Treatment Units (ETUs) in Africa This lecture will focus on EVD in the West African setting. Ebola Virus Disease and Clinical Care: The training and information you receive in this course will Part I: History, Transmission, and Clinical not cover the use of certain interventions such as intubation Presentation or dialysis which are not available in West African Ebola Treatment Units (ETUs). You will need supplemental training This presentation is current as of December 2014. This presentation contains materials from Centers for Disease Control and to care for patients appropriately in countries where advanced Prevention (CDC), Médecins Sans Frontières (MSF), and World Health Organization (WHO). care is available. U.S. Department of Health and Human Services U.S. Department of Health and Human Services Centers for Disease Control and Prevention Centers for Disease Control and Prevention version 12.03.2014 The learning objectives for this lecture are to: Learning Objectives ▶ Describe the routes of Ebola virus transmission Describe the routes of Ebola virus transmission Explain when and how patients are infectious ▶ Explain when and how patients are infectious Describe the clinical features of patients with Ebola ▶ Describe screening criteria for Ebola virus disease Describe the clinical features of patients with Ebola (EVD) used in West Africa Explain how to identify patients with suspected ▶ Describe screening criteria for EVD used in West Africa EVD who present to the ETU ▶ Explain how to identify patients with suspected EVD who present to the ETU This presentation contains materials from CDC, MSF, and WHO 2 A number of different viruses cause viral hemorrhagic fever. -
Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview
1 Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview Contents This Weekly Bulletin focuses on selected acute public health emergencies occurring in the WHO African Region. The WHO Health Emergencies Programme (WHE) is currently monitoring 60 events in the region. This week’s edition covers key ongoing events, including: 2 Overview Ebola virus disease outbreak in the Democratic Republic of the Congo 3 - 6 Ongoing events Cholera in Burundi Cholera in Cameroon 7 Summary of major Yellow fever in Nigeria. issues challenges and proposed actions For each of these events, a brief description, followed by public health measures implemented and an interpretation of the situation is provided. 8 All events currently being monitored Major issues and challenges include: The Ebola virus disease (EVD) outbreak in the Democratic Republic of the Congo (DRC) is in a critical phase as it enters its sixth month since the declaration of the outbreak. Despite the use of an effective vaccine, novel therapeutics as well as other EVD strategic interventions, the outbreak is persisting due to security challenges, pockets of community reluctance and inadequate infection prevention and control in some health facilities. Nevertheless, WHO and partners, under the government’s leadership, continue to respond to the EVD outbreak and remain committed to containing the outbreak. The Ministry of Health of Burundi has declared a new outbreak of cholera in the country. This outbreak, which is rapidly evolving, is particularly affecting people living in overcrowded areas, where sanitation conditions are precarious. Given that the risk factors for transmission of water-borne diseases are prevalent in the affected communities, there is a need to aggressively tackle this outbreak at its early stage using relevant sectors in order to avoid further spread. -

Monkeypox Virus Emergence in Wild Chimpanzees Reveals Distinct Clinical Outcomes and Viral Diversity
ARTICLES https://doi.org/10.1038/s41564-020-0706-0 Monkeypox virus emergence in wild chimpanzees reveals distinct clinical outcomes and viral diversity Livia V. Patrono1,6, Kamilla Pléh1,2,6, Liran Samuni2,3, Markus Ulrich1, Caroline Röthemeier1, Andreas Sachse1, Silvia Muschter4, Andreas Nitsche4, Emmanuel Couacy-Hymann5, Christophe Boesch2,3, Roman M. Wittig 2,3, Sébastien Calvignac-Spencer1 and Fabian H. Leendertz 1 ✉ Monkeypox is a viral zoonotic disease on the rise across endemic habitats. Despite the growing importance of monkeypox virus, our knowledge on its host spectrum and sylvatic maintenance is limited. Here, we describe the recent repeated emergence of monkeypox virus in a wild, human-habituated western chimpanzee (Pan troglodytes verus, hereafter chimpanzee) population from Taï National Park, Ivory Coast. Through daily monitoring, we show that further to causing its typical exanthematous syn- drome, monkeypox can present itself as a severe respiratory disease without a diffuse rash. By analysing 949 non-invasively collected samples, we identify the circulation of at least two distinct monkeypox virus lineages and document the shedding of infectious particles in faeces and flies, suggesting that they could mediate indirect transmission. We also show that the carnivo- rous component of the Taï chimpanzees’ diet, mainly consisting of the sympatric monkeys they regularly hunt, did not change nor shift towards rodent consumption (the presumed reservoir) before the outbreaks, suggesting that the sudden emergence of monkeypox virus in this population is probably due to changes in the ecology of the virus itself. Using long-term mortality surveillance data from Taï National Park, we provide evidence of little to no prior viral activity over at least two decades. -

Understanding Ebola
Understanding Ebola With the arrival of Ebola in the United States, it's very easy to develop fears that the outbreak that has occurred in Africa will suddenly take shape in your state and local community. It's important to remember that unless you come in direct contact with someone who is infected with the disease, you and your family will remain safe. State and government agencies have been making preparations to address isolated cases of infection and stop the spread of the disease as soon as it has been positively identified. Every day, the Centers of Disease Control and Prevention (CDC) is monitoring developments, testing for suspected cases and safeguarding our lives with updates on events and the distribution of educational resources. Learning more about Ebola and understanding how it's contracted and spread will help you put aside irrational concerns and control any fears you might have about Ebola severely impacting your life. Use the resources below to help keep yourself calm and focused during this unfortunate time. Ebola Hemorrhagic Fever Ebola hemorrhagic fever (Ebola HF) is one of numerous Viral Hemorrhagic Fevers. It is a severe, often fatal disease in humans and nonhuman primates (such as monkeys, gorillas, and chimpanzees). Ebola HF is caused by infection with a virus of the family Filoviridae, genus Ebolavirus. When infection occurs, symptoms usually begin abruptly. The first Ebolavirus species was discovered in 1976 in what is now the Democratic Republic of the Congo near the Ebola River. Since then, outbreaks have appeared sporadically. There are five identified subspecies of Ebolavirus. -

Select Biological Agent and Toxin List
Select Biological Agent and Toxin List HHS Non-Overlap Select Agents and Toxins USDA High Consequence Livestock Pathogens - Crimean-Congo haemorrhagic fever virus and Toxins (Non-Overlap agents and toxins) - Coccidioides posadasii - Akabane virus - Ebola viruses - African swine fever virus - Cercopithecine herpesvirus 1 (Herpes B virus) - African horse sickness virus - Lassa fever virus - Avian influenza virus (highly pathogenic) - Marburg virus - Blue tongue virus (Exotic) - Monkeypox virus - Bovine spongiform encephalopathy agent - Rickettsia prowazekii - Camel pox virus - Rickettsia rickettsii - Classical swine fever virus South American haemorrhagic fever viruses - Cowdria ruminantium (Heartwater) - Junin - Foot and mouth disease virus - Machupo - Goat pox virus - Sabia - Lumpy skin disease virus - Flexal - Japanese encephalitis virus - Guanarito - Malignant catarrhal fever virus (Exotic) Tick-borne encephalitis complex (flavi) viruses - Menangle virus - Central European tick-borne encephalitis - Mycoplasma capricolum/M.F38/M. mycoides capri - Far Eastern tick-borne encephalitis - Mycoplasma mycoides mycoides - Russian spring and summer encephalitis - Newcastle disease virus (VVND) - Kyasanur forest disease - Peste Des Petits Ruminants virus - Omsk hemorrhagic fever - Rinderpest virus - Variola major virus (Smallpox virus) - Sheep pox virus - Variola minor virus (Alastrim) - Swine vesicular disease virus - Yersinia pestis - Vesicular stomatitis virus (Exotic) - Abrin - Conotoxins - Diacetoxyscirpenol Plant Pathogens - Ricin - Liberobacter -

Emergence of Monkeypox — West and Central Africa, 1970–2017
Morbidity and Mortality Weekly Report Emergence of Monkeypox — West and Central Africa, 1970–2017 Kara N. Durski, MPH1; Andrea M. McCollum, PhD2; Yoshinori Nakazawa, PhD2; Brett W. Petersen, MD2; Mary G. Reynolds, PhD2; Sylvie Briand, MD, PhD1; Mamoudou Harouna Djingarey, MD3; Victoria Olson, PhD2; Inger K. Damon, MD, PhD2, Asheena Khalakdina, PhD1 The recent apparent increase in human monkeypox cases Monkeypox is a zoonotic orthopoxvirus with a similar dis- across a wide geographic area, the potential for further spread, ease presentation to smallpox in humans, with the additional and the lack of reliable surveillance have raised the level of distinguishing symptom of lymphdenopathy. After an initial concern for this emerging zoonosis. In November 2017, the febrile prodrome, a centrifugally distributed maculopapular World Health Organization (WHO), in collaboration with rash develops, with lesions often present on the palms of CDC, hosted an informal consultation on monkeypox with the hands and soles of the feet. The infection can last up to researchers, global health partners, ministries of health, and 4 weeks, until crusts separate and a fresh layer of skin is formed. orthopoxvirus experts to review and discuss human monkeypox Sequelae include secondary bacterial infections, respiratory in African countries where cases have been recently detected and distress, bronchopneumonia, gastrointestinal involvement, also identify components of surveillance and response that need dehydration, encephalitis, and ocular infections, which can improvement. Endemic human monkeypox has been reported result in permanent corneal scarring. No specific treatment for from more countries in the past decade than during the previ- a monkeypox virus infection currently exists, and patients are ous 40 years.