2018 Apigenin Male Infertility (2).Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Baicalin Promotes the Viability of Schwann Cells in Vitro by Regulating Neurotrophic Factors
EXPERIMENTAL AND THERAPEUTIC MEDICINE 14: 507-514, 2017 Baicalin promotes the viability of Schwann cells in vitro by regulating neurotrophic factors WENPU ZUO1*, HUAYU WU2*, KUN ZHANG3,4, PEIZHEN LV3,4, FUBEN XU1,5, WEIZHE JIANG6, LI ZHENG1,5 and JINMIN ZHAO3-5 1Medical and Scientific Research Center;2 Department of Cell Biology and Genetics, School of Premedical Sciences; 3Guangxi Key Laboratory of Regenerative Medicine, Guangxi Medical University; 4Department of Orthopedic Trauma and Hand Surgery, The First Affiliated Hospital of Guangxi Medical University;5 Key Laboratory of Regenerative Medicine of Guangxi High School; 6Department of Pharmacology, Guangxi Medical University, Nanning, Guangxi 530021, P.R. China Received January 20, 2016; Accepted February 14, 2017 DOI: 10.3892/etm.2017.4524 Abstract. The proliferation and migration of Schwann of baicalin exhibited the greatest cell viability and gene cells (SCs) are key events in the process of peripheral nerve expression of the studied neurotrophic factors. The present repair. This is required to promote the growth of SCs and is findings suggested that baicalin likely affects SCs metabo- a challenge during the treatment of peripheral nerve injury. lism, through modulating the expression of neurotrophic Baicalin is a natural herb‑derived flavonoid compound, which factors. To conclude, the present study indicates that baicalin has been reported to possess neuroprotective effects on rats may be potential therapeutic agent for treating peripheral with permanent brain ischemia and neuronal differentiation nerve regeneration. of neural stem cells. The association of baicalin with neuro- protection leads to the suggestion that baicalin may exert Introduction effects on the growth of SCs. -

The Antidepressant Effect of Testosterone an Effect Of
Neurology, Psychiatry and Brain Research 32 (2019) 104–110 Contents lists available at ScienceDirect Neurology, Psychiatry and Brain Research journal homepage: www.elsevier.com/locate/npbr The antidepressant effect of testosterone: An effect of neuroplasticity? T ⁎ Andreas Walthera,b,c, , Joanna Marta Wasielewskad, Odette Leitere a Biological Psychology, Technische Universität Dresden, Dresden, Germany b Clinical Psychology and Psychotherapy, University of Zurich, Zurich, Switzerland c Task Force on Men’s Mental Health of the World Federation of the Societies of Biological Psychiatry (WFSBP), Germany d Center for Regenerative Therapies (CRTD), Technische Universität Dresden, Germany e Queensland Brain Institute (QBI), University of Queensland, St Lucia, QLD, 4072, Australia ARTICLE INFO ABSTRACT Keywords: Background: Rodent and human studies indicate that testosterone has an antidepressant effect. The mechanisms Testosterone via which testosterone exerts its antidepressant effect, however, remain to be elucidated. Some studies assume Depression downstream effects of testosterone on sexual function and vitality followed by improvement of mood. Emerging Men evidence suggests that testosterone may be acting in the brain within depression-relevant areas, whereby eli- Neurogenesis citing direct antidepressant effects, potentially via neuroplasticity. Neuroplasticity Methods: Literature was searched focusing on testosterone treatment and depression and depression-like be- Antidepressant havior. Due to the unilateral clinical use of testosterone in men and the different modes of action of sex hor- mones in the central nervous system in men and women, predominantly studies on male populations were identified. Results: The two proposed mechanisms via which testosterone might act as antidepressant in the central nervous system are the support of neuroplasticity as well as the activation of the serotonin system. -

Estroquench™ Hormone Specific Formulation™
PRODUCT DATA DOUGLAS LABORATORIES® 08/2014 1 EstroQuench™ Hormone Specific Formulation™ DESCRIPTION EstroQuench™ is a Hormone Specific Formulation™ of ingredients that have documented anti-aromatase activity as well as androgenic adaptogens which support the function of endogenous aromatase inhibitors. Collectively these herbs promote minimal production and function of estrogens, while promoting testosterone function, including optimal sexual function in both genders. This formulation is designed to quench excessive production of estrogens and aberrant functions of them while supporting optimal function of androgens by maintaining the health of androgen producing glands.† Hormone Specific Formulation™ provided by Douglas Laboratories® and formulated by Dr. Joseph J Collins is created to support the optimal function of specific hormones through the use of hormone specific adaptogens, hormone specific agonists and hormone specific functional mimetics. This formulation may be used as part of a hormone health program with dietary and nutrient support. In addition, this formulation may be used by clinicians as an adjuvant to support optimal hormone health in patients who have been prescribed bioidentical hormone therapies. FUNCTIONS Aromatase (a cytochrome P450 enzyme {CYP19}) is the enzyme that controls the conversion of androgens to estrogens. More specifically, aromatase is the enzyme responsible for catalyzing the biosynthesis of androstenedione into estrone, and the biosynthesis of testosterone to estradiol. Estrogens include the broad range of aromatized hormones created form androgens. The specific attribute of estrogens that separate them from progestogens, androgens and corticoids is that estrogens are the only aromatized steroid hormones. Estradiol, the most potent endogenous estrogen, is biosynthesized by aromatization from androgens by aromatase (which is also called estrogen synthase). -

Mechanism of the Inhibitory Effect of Antiinflammatory Baicalin on Airway Reconstruction in COPD Rats
Research Paper Mechanism of the Inhibitory Effect of Antiinflammatory Baicalin on Airway Reconstruction in COPD Rats J. QIU, W. GONG AND J. DONG* Department of Integrative Medicine, Huashan Hospital, Fudan University, 12 Middle Wulumiqi Road, Shanghai, China Qiu et al.: Mechanism of baicalin in inhibiting airway reconstruction in COPD rats The mechanism of baicalin in airway reconstruction in rats with chronic obstructive pulmonary disease was investigated. The chronic obstructive pulmonary disease models were established in rats through smoke inhalation and instilling lipopolysaccharide. The rats were then divided into the control group and the experimental group, a blank group was used as a reference point of the experiment. Rats in the experiment group received baicalin either at a high dose (80 mg/kg/d, H1) or at a low dose (25 mg/kg/d, H2) to analyse the airway reconstruction functions and antiinflammatory effects of baicalin. During the experiment, the general conditions of the rats were compared. After the experiment, lung tissues of the rats were obtained for Hematoxylin-Eosin staining, and the pathological changes were observed. In addition, the bronchial walls were measured and analysed. Using immunohistochemical staining, the expression levels of tumour necrosis factor-α and interferon-γ in rat lung tissues were analysed and compared. Hematoxylin-Eosin staining of lung tissues showed that the rats with chronic obstructive pulmonary disease had severe pathological damages; compared to the blank group, while in rats treated with baicalin, bronchial obstruction, alveolar structure and inflammatory infiltration were improved, and the differences were statistically significant (p<0.05). After baicalin administration, the bronchial wall thickness in chronic obstructive pulmonary disease rats was reduced, collagen deposition in the bronchial epithelium was improved, and airway smooth muscle proliferation was alleviated compared to the control group. -

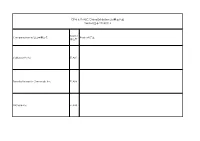
Test Report Comprehensive Hormone Insights™
698814 COMPREHENSIVE HORMONE INSIGHTS™ TEST REPORT Dr. Maximus, N.D. E: [email protected] Date of Collection: P: 403-241-4500 Time of Collection: F: 403-241-4501 Date of Receipt: www.rmalab.com Reported On: CHI Accession: 698814 Healthcare Professional Patient Age: Dr. Maximus, N.D. Date of Birth: Gender: Male F: Relevant Medications Biometrics Curcumin Height (in) : 73 Weight (lb) : 180 BMI : 24 Waist (in) : 35 Hip (in) : 41 CHI Accession: 698814 SUMMARY HMUS01 How to read the graphs LEGEND: 50 66 Sex Steroid Hormones 50 66 Middle third of 33 33 84 reference population Hormone Start of 83 100 80 100 highest 16 Percentile Precursors 16 Percentile third of Sum of Androgens Sum of Estrogens 50 66 reference 0 0 population (T, DHT, α+β androstanediol) Listed in Interp Guide 33 84 End of 100 16 lowest Percentile00 50 66 50 66 third of 33 33 84 reference 0 population Patient’s percentile rank 81 100 95 100 compared to reference 16 Percentile 16 Percentile population (see summary) DHEA + Metabolites Sum of Progesterone Metabolites 0 (DHEA + A + E) 0 α+β Pregnanediol Cortisol Melatonin Oxidative Stress Free Cortisol Profile (ng/mg) 100 50 66 50 66 33 84 33 84 80 64 100 0 100 16 Percentile 16 Percentile 60 6-sulfatoxy 8-Hydroxy-2- 0 Melatonin 0 deoxyguanosine 40 (Overnight) (Overnight) 20 6-sulfatoxymelatonin provides 8-hydroxy-2-deoxyguanosine is Cortisol/Creatinine (ng/mg) insight into melatonin levels. a marker of oxidative stress 0 Morning Dinner Bedtime A B C 50 66 Free cortisol Cortisol Metabolites 33 84 profile is used to provides a general Testosterone Cortisol assess diurnal assessment of 16 100 cortisol rhythm adrenal cortisol 16 Percentile Cortisol production Cortisol Metabolites 0 (α+β THF + THE) Testosterone Cortisol/Testosterone provides insight into relative catabolic (cortisol) and anabolic (testosterone) states. -

(Apigenin, Luteolin, Chrysin) and Their Importance for Health
Mellifera 2020, 20(1):16-27 MELLIFERA REVIEW ARTICLE Flavones (Apigenin, Luteolin, Chrysin) and Their Importance for Health Fatma Özsel ÖZCAN1*, Ozan ALDEMİR2, Bülent KARABULUT3 1Beykoz Üniversity, Faculty of Art and Design, Department of Gastronomy and Culinary Arts, İstanbul, Turkey 2Ege University Faculty of Medicine, Department of Biochemistry, İzmir, TURKEY 3Ege University Faculty of Medicine, Department of Oncology, İzmir, TURKEY * Corresponding author e-mail: [email protected] Received: 14th March, 2020; accepted: 4th May, 2020; published: 29th June, 2020 A B S T R A C T It has been shown in recent years that foods called functional foods may protect against certain types of cancer, cardiovascular diseases and cognitive dysfunctions. In the studies performed, the flavonoids (apigenin, chrysin, luteolin) which are subclass of flavonoids have been shown to have antioxidant, antiinflammatory, antiallergic, neuroprotective and cardioprotective effects and it is presented as the current treatment method in the treatment of some diseases. The structure function, nutritional resources and potential therapeutic properties of the flavones, which are also used as supplement in the compost, have been studied. The purpose of this review is to evaluate the therapeutic effects of flavones in certain diseases. The positive effect of 16 flavones on health can be proven in many experimental studies and can be proven in the long run. Keywords: Functional nutrients, flavones, apigenin, luteolin, chrysin Introduction Polyphenolic flavonoids are among the affected by factors such as plant species, wide variety of phytochemicals found in the environment, genetics, light, maturity, human diet. Current studies reveal that harvest [3]. Flavones, a subset of dietary flavonoids are inversely related to flavonoids, form glycosylation and contain many cancers and age-related diseases [1]. -

Original Article Hispidulin Induces Mitochondrial Apoptosis in Acute Myeloid Leukemia Cells by Targeting Extracellular Matrix Metalloproteinase Inducer
Am J Transl Res 2016;8(2):1115-1132 www.ajtr.org /ISSN:1943-8141/AJTR0014691 Original Article Hispidulin induces mitochondrial apoptosis in acute myeloid leukemia cells by targeting extracellular matrix metalloproteinase inducer Hui Gao1*, Yongji Liu2*, Kan Li3, Tianhui Wu4, Jianjun Peng5, Fanbo Jing6 1Qingdao University Medical College, Qingdao, Shandong, 266071, China; 2Qingdao Hiser Medical Center, Qingdao, Shandong 266000, China; 3Shandong Provincial Hospital Affiliated to Shandong University, Shandong 250021, China; 4Qingdao 5th People’s Hospital, Qingdao, Shandong 266000, China; 5College of Life Sciences, Chongqing Normal University, Chongqing 401331, China; 6The Affiliated Hospital of Qingdao University, Qingdao, Shandong 266003, China. *Equal contributors. Received August 18, 2015; Accepted January 12, 2016; Epub February 15, 2016; Published February 29, 2016 Abstract: Acute myeloid leukemia (AML) represents a heterogeneous group of hematological neoplasms with marked heterogeneity in response to both standard therapy and survival. Hispidulin, a flavonoid compound that is anactive ingredient in the traditional Chinese medicinal herb Salvia plebeia R. Br, has recently been reported to have anantitumor effect against solid tumors in vitro and in vivo. The aim of the present study was to investigate the effects of hispidulin on the human leukemia cell line in vitro and the underlying mechanisms of its actions on these cells. Our results showed that hispidulin inhibits AML cell proliferation in a dose- and time-dependent man- ner, and induces cell apoptosis throughan intrinsic mitochondrial pathway. Our results also revealed that hispidulin treatment significantly inhibits extracellular matrix metalloproteinase inducer (EMMPRIN) expression in both tested AML cell lines in a dose-dependent manner, and that the overexpression of EMMPRIN protein markedly attenuates hispidulin-induced cell apoptosis. -

Inhibitory Effect of Acacetin, Apigenin, Chrysin and Pinocembrin on Human Cytochrome P450 3A4
ORIGINAL SCIENTIFIC PAPER Croat. Chem. Acta 2020, 93(1), 33–39 Published online: August 03, 2020 DOI: 10.5562/cca3652 Inhibitory Effect of Acacetin, Apigenin, Chrysin and Pinocembrin on Human Cytochrome P450 3A4 Martin Kondža,1 Hrvoje Rimac,2,3 Željan Maleš,4 Petra Turčić,5 Ivan Ćavar,6 Mirza Bojić2,* 1 University of Mostar, Faculty of Pharmacy, Matice hrvatske bb, 88000 Mostar, Bosnia and Herzegovina 2 University of Zagreb, Faculty of Pharmacy and Biochemistry, Department of Medicinal Chemistry, A. Kovačića 1, 10000 Zagreb, Croatia 3 South Ural State University, Higher Medical and Biological School, Laboratory of Computational Modeling of Drugs, 454000 Chelyabinsk, Russian Federation 4 University of Zagreb, Faculty of Pharmacy and Biochemistry, Department of Pharmaceutical Botany, Schrottova 39, 10000 Zagreb, Croatia 5 University of Zagreb, Faculty of Pharmacy and Biochemistry, Department of Pharmacology, Domagojeva 2, 10000 Zagreb, Croatia 6 University of Mostar, Faculty of Medicine, Kralja Petra Krešimira IV bb, 88000 Mostar, Bosnia and Herzegovina * Corresponding author’s e-mail address: [email protected] RECEIVED: June 26, 2020 REVISED: July 28, 2020 ACCEPTED: July 30, 2020 Abstract: Cytochrome P450 3A4 is the most significant enzyme in metabolism of medications. Flavonoids are common secondary plant metabolites found in fruits and vegetables. Some flavonoids can interact with other drugs by inhibiting cytochrome P450 enzymes. Thus, the objective of this study was to determine inhibition kinetics of cytochrome P450 3A4 by flavonoids: acacetin, apigenin, chrysin and pinocembrin. For this purpose, testosterone was used as marker substrate, and generation of the 6β-hydroxy metabolite was monitored by high performance liquid chromatography coupled with diode array detector. -
Cphi & P-MEC China Exhibition List展商名单version版本20180116
CPhI & P-MEC China Exhibition List展商名单 Version版本 20180116 Booth/ Company Name/公司中英文名 Product/产品 展位号 Carbosynth Ltd E1A01 Toronto Research Chemicals Inc E1A08 SiliCycle Inc. E1A10 SA TOURNAIRE E1A11 Indena SpA E1A17 Trifarma E1A21 LLC Velpharma E1A25 Anuh Pharma E1A31 Chemclone Industries E1A51 Hetero Labs Limited E1B09 Concord Biotech Limited E1B10 ScinoPharm Taiwan Ltd E1B11 Dongkook Pharmaceutical Co., Ltd. E1B19 Shenzhen Salubris Pharmaceuticals Co., Ltd E1B22 GfM mbH E1B25 Leawell International Ltd E1B28 DCS Pharma AG E1B31 Agno Pharma E1B32 Newchem Spa E1B35 APEX HEALTHCARE LIMITED E1B51 AMRI E1C21 Aarti Drugs Limited E1C25 Espee Group Innovators E1C31 Ruland Chemical Co., Ltd. E1C32 Merck Chemicals (Shanghai) Co., Ltd. E1C51 Mediking Pharmaceutical Group Ltd E1C57 珠海联邦制药股份有限公司/The United E1D01 Laboratories International Holdings Ltd. FMC Corporation E1D02 Kingchem (Liaoning) Chemical Co., Ltd E1D10 Doosan Corporation E1D22 Sunasia Co., Ltd. E1D25 Bolon Pharmachem Co., Ltd. E1D26 Savior Lifetec Corporation E1D27 Alchem International Pvt Ltd E1D31 Polish Investment and Trade Agency E1D57 Fischer Chemicals AG E1E01 NGL Fine Chem Limited E1E24 常州艾柯轧辊有限公司/ECCO Roller E1E25 Linnea SA E1E26 Everlight Chemical Industrial Corporation E1E27 HARMAN FINOCHEM E1E28 Zhechem Co Ltd E1F01 Midas Pharma GmbH Shanghai Representativ E1F03 Supriya Lifescience Ltd E1F10 KOA Shoji Co Ltd E1F22 NOF Corporation E1F24 上海贺利氏工业技术材料有限公司/Heraeus E1F26 Materials Technology Shanghai Ltd. Novacyl Asia Pacific Ltd E1F28 PharmSol Europe Limited E1F32 Bachem AG E1F35 Louston International Inc. E1F51 High Science Co Ltd E1F55 Chemsphere Technology Inc. E1F57a PharmaCore Biotech Co., Ltd. E1F57b Rockwood Lithium GmbH E1G51 Sarv Bio Labs Pvt Ltd E1G57 抗病毒类、抗肿瘤类、抗感染类和甾体类中间体、原料药和药物制剂及医药合约研发和加工服务 上海创诺医药集团有限公司/Shanghai Desano APIs and Finished products of ARV, Oncology, Anti-infection and Hormone drugs and E1H01 Pharmaceuticals Co., Ltd. -

Ameliorative Effects of a Combination of Baicalin, Jasminoidin and Cholic Acid on Ibotenic Acid-Induced Dementia Model in Rats
Ameliorative Effects of a Combination of Baicalin, Jasminoidin and Cholic Acid on Ibotenic Acid-Induced Dementia Model in Rats Junying Zhang1,2, Peng Li3., Yanping Wang4., Jianxun Liu3, Zhanjun Zhang2*, Weidong Cheng1*, Yongyan Wang4 1 School of Basic Medical Sciences, Lanzhou University, Lanzhou, P. R. China, 2 State Key Laboratory of Cognitive Neuroscience and Learning, Beijing Normal University, Beijing, P. R. China, 3 The Laboratory Research Center of Xiyuan Hospital, China Academy of Chinese Medical Sciences, Beijing, P. R. China, 4 The Institute of Basic Clinical Medicine, China Academy of Chinese Medical Sciences, Beijing, P. R. China Abstract Aims: To investigate the therapeutic effects and acting mechanism of a combination of Chinese herb active components, i.e., a combination of baicalin, jasminoidin and cholic acid (CBJC) on Alzheimer’s disease (AD). Methods: Male rats were intracerebroventricularly injected with ibotenic acid (IBO), and CBJC was orally administered. Therapeutic effect was evaluated with the Morris water maze test, FDG-PET examination, and histological examination, and the acting mechanism was studied with DNA microarrays and western blotting. Results: CBJC treatment significantly attenuated IBO-induced abnormalities in cognition, brain functional images, and brain histological morphology. Additionally, the expression levels of 19 genes in the forebrain were significantly influenced by CBJC; approximately 60% of these genes were related to neuroprotection and neurogenesis, whereas others were related to anti-oxidation, protein degradation, cholesterol metabolism, stress response, angiogenesis, and apoptosis. Expression of these genes was increased, except for the gene related to apoptosis. Changes in expression for 5 of these genes were confirmed by western blotting. Conclusion: CBJC can ameliorate the IBO-induced dementia in rats and may be significant in the treatment of AD. -

Characterization of the CYP3A4 Enzyme Inhibition Potential of Selected Flavonoids
Article Characterization of the CYP3A4 Enzyme Inhibition Potential of Selected Flavonoids Martin Kondža 1 , Mirza Boji´c 2,* , Ivona Tomi´c 1, Željan Maleš 2 , Valentina Rezi´c 3 and Ivan Cavar´ 4 1 Faculty of Pharmacy, University of Mostar, Matice Hrvatske bb, 88000 Mostar, Bosnia and Herzegovina; [email protected] (M.K.); [email protected] (I.T.) 2 University of Zagreb Faculty of Pharmacy and Biochemistry, Ante Kovaˇci´ca1, 10000 Zagreb, Croatia; [email protected] 3 Farmavita d.o.o., Igmanska 5A, 71000 Sarajevo, Bosnia and Herzegovina; [email protected] 4 Faculty of Medicine, University of Mostar, Zrinskog Frankopana 34, 88000 Mostar, Bosnia and Herzegovina; [email protected] * Correspondence: [email protected]; Tel.: +385-1-4818-304 Abstract: Acacetin, apigenin, chrysin, and pinocembrin are flavonoid aglycones found in foods such as parsley, honey, celery, and chamomile tea. Flavonoids can act as substrates and inhibitors of the CYP3A4 enzyme, a heme containing enzyme responsible for the metabolism of one third of drugs on the market. The aim of this study was to investigate the inhibitory effect of selected flavonoids on the CYP3A4 enzyme, the kinetics of inhibition, the possible covalent binding of the inhibitor to the enzyme, and whether flavonoids can act as pseudo-irreversible inhibitors. For the determination of inhibition kinetics, nifedipine oxidation was used as a marker reaction. A hemochromopyridine test was used to assess the possible covalent binding to the heme, and incubation with dialysis was used in order to assess the reversibility of the inhibition. -

Mitochondrial Dysfunction and Chronic Inflammation in Polycystic
International Journal of Molecular Sciences Review Mitochondrial Dysfunction and Chronic Inflammation in Polycystic Ovary Syndrome Siarhei A. Dabravolski 1,*, Nikita G. Nikiforov 2,3,4, Ali H. Eid 5,6,7, Ludmila V. Nedosugova 8, Antonina V. Starodubova 9,10, Tatyana V. Popkova 11, Evgeny E. Bezsonov 4,12 and Alexander N. Orekhov 4 1 Department of Clinical Diagnostics, Vitebsk State Academy of Veterinary Medicine [UO VGAVM], 7/11 Dovatora Str., 210026 Vitebsk, Belarus 2 Center of Collective Usage, Institute of Gene Biology, Russian Academy of Sciences, 34/5 Vavilova Street, 119334 Moscow, Russia; [email protected] 3 Laboratory of Medical Genetics, Institute of Experimental Cardiology, National Medical Research Center of Cardiology, 121552 Moscow, Russia 4 Laboratory of Cellular and Molecular Pathology of Cardiovascular System, Institute of Human Morphology, 3 Tsyurupa Street, 117418 Moscow, Russia; [email protected] (E.E.B.); [email protected] (A.N.O.) 5 Department of Basic Medical Sciences, College of Medicine, QU Health, Qatar University, Doha 2713, Qatar; [email protected] 6 Biomedical and Pharmaceutical Research Unit, QU Health, Qatar University, Doha 2713, Qatar 7 Department of Pharmacology and Toxicology, Faculty of Medicine, American University of Beirut, Beirut P.O. Box 11-0236, Lebanon 8 Citation: Dabravolski, S.A.; Federal State Autonomous Educational Institution of Higher Education, I. M. Sechenov First Moscow State Nikiforov, N.G.; Eid, A.H.; Medical University (Sechenov University), 8/2 Trubenskaya Street, 119991 Moscow, Russia; [email protected] 9 Federal Research Centre for Nutrition, Biotechnology and Food Safety, 2/14 Ustinsky Passage, Nedosugova, L.V.; Starodubova, A.V.; 109240 Moscow, Russia; [email protected] Popkova, T.V.; Bezsonov, E.E.; 10 Pirogov Russian National Research Medical University, 1 Ostrovitianov Street, 117997 Moscow, Russia Orekhov, A.N.