WHO Guidelines on Hand Hygiene in Health Care (Advanced Draft)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
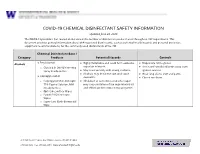
EH&S COVID-19 Chemical Disinfectant Safety Information
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -

Chlorhexidine Soap Instructions
Pre-Operative Bathing Instructions Infection Prevention Because skin is not sterile, we need to be sure that your skin is as free of germs as possible before your admission. You can reduce the number of germs on your skin and decrease the risk of surgical site infection by preparing your skin with a special soap called chlorhexidine gluconate (CHG). The instructions for use are attached. What is CHG? CHG is a chemical antiseptic that is effective on both gram-positive and gram-negative bacteria. It is both bacteriocidal (kills) and bacteriostatic (stops reproductions) of any bacteria on the skin. CHG is in several products such as mouthwash, contact lens solution, wound wash, acne skin wash topical skin cleansers (chloraprep-what is used to clean your skin before an IV), thus we do not expect using this soap will cause skin irritation but please speak with your primary care physician to discuss any allergies. Studies show that repeated use of CHG soap enhances the ability of CHG to reduce bacterial counts on the skin; not only during the immediate period after the shower, but for a number of hours afterward. Studies suggest that patients may benefit from bathing or showering with CHG soap for at least 3 days before surgery in order to achieve the most benefit. It is unknown whether using CHG soap for less than or more than 3 days is beneficial. We recommend 3 days of treatment but understand this is not always possible and bathing the night before and the day of using CHG is acceptable. CHG soap can be purchased at any local pharmacy. -

Infection Control in Dentistry: How to Asepsis Photographic Mirrors?
Infection control in dentistry: how to asepsis photographic mirrors? Amanda Osório Ayres de Freitas* Mariana Marquezan* Giselle Naback Lemes Vilani* Rodrigo César Santiago* Luiz Felipe de Miranda Costa* Sandra Regina Torres** Abstract: The aim of this study was to evaluate the efficacy of six different methods of disinfection and sterilization of intraoral photographic mirrors through microbiological testing and to analysis their potential harm to mirrors’ surface. Fourteen occlusal mirrors were divided into seven groups. Group 1 comprised two mirrors as received from manufacturer. The other six groups comprised mirrors disinfected/sterilized by autoclave, immersion in enzymatic detergent, and friction with chlorhexidine detergent, chlorhexidine wipes, common detergent and 70% ethylic alcohol. Microbiological and quality surface analyses were performed. Sterilization in autoclave was microbiologic effective, but caused damage to the mirror surface. Chlorhexidine (in wipes or detergent) and liquid soap were effective disinfectant agents for photographic mirrors decontamination, without harmful effect on its surface. Enzymatic detergent immersion and friction with 70% ethylic alcohol were not effective as disinfectant agents for photographic mirrors decontamination. According to the results, the more effective and safe methods for photographic mirrors disinfection were friction with chlorhexidine wipes or detergent, as well as liquid soap. Results, the most efficacious methods for photographic mirrors disinfection were friction with chlorhexidine wipes and detergent, as well as common detergent. Descriptors: Dental Instruments; Decontamination; Microbiology; Surface Properties. *Doutoranda em Odontologia na Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brasil **Pósdoutora em odontologia pela University of Washington (UW), Seattle, WA, Estados Unidos ISSN 22365843 │ 93 Introduction Dental photography is an important tool for diagnostic and treatment planning, and it’s also a registration of the patient’s condition before and after treatment. -

Health Evidence Review Commission's Value-Based Benefits Subcommittee
Health Evidence Review Commission's Value-based Benefits Subcommittee September 28, 2017 8:00 AM - 1:00 PM Clackamas Community College Wilsonville Training Center, Room 111-112 29373 SW Town Center Loop E, Wilsonville, Oregon, 97070 Section 1.0 Call to Order AGENDA VALUE-BASED BENEFITS SUBCOMMITTEE September 28, 2017 8:00am - 1:00pm Wilsonville Training Center, Rooms 111-112 29353 SW Town Center Loop E Wilsonville, Oregon 97070 A working lunch will be served at approximately 12:00 PM All times are approximate I. Call to Order, Roll Call, Approval of Minutes – Kevin Olson 8:00 AM II. Staff report – Ariel Smits, Cat Livingston, Darren Coffman 8:05 AM A. Chronic Pain Task Force meeting report B. Errata C. Retreat III. Straightforward/Consent agenda – Ariel Smits 8:15 AM A. Consent table B. Straightforward Modifications to the Prioritized List Changes: Continuous Glucose Monitoring in Diabetes Mellitus C. Straightforward changes to the PPI guideline for Barrett’s esophagus with dysplasia D. Tobacco cessation guideline clarification IV. Advisory Panel reports 8:25 AM A. OHAP 1. 2018 CDT code placement recommendations V. Previous discussion items 8:30 AM A. Consideration for prioritization on lines 500/660, Services with Minimal or No Clinical Benefit and/or Low Cost-Effectiveness 1. New medications for the treatment of Duchenne muscular dystrophy i. deflazacort (Emflaza) ii. etepliren (Exondys 51) VI. New discussion items 9:30 AM A. Testicular prostheses B. Capsulorrhaphy for recurrent shoulder dislocation C. Transcutaneous neurostimulators D. Physical therapy for interstitial cystitis E. Acute peripheral nerve injuries F. SOI on role of Prioritized List in Coverage G. -

SAP Connected Goods – Smart Toilets
SAP Connected Goods – Smart Toilets Story A toilet is basically all that’s between you and a life full of disease and hardship. It’s certainly the most important appliance in your house. Just ask the millions of people around the world who die from diseases brought on by bad sanitation. One in three people around the world don’t have access to even the most basic of sanitation services, which means they are forced to go outside. Municipalities and civic bodies were driven by a basic premise that sanitation and more specifically public sanitation is untouched by innovation of any nature in the past century or so, in spite of innovations invading all other spheres of our life. The problem: Not enough toilets. One of the solutions to this problem is ‘Smart Toilets’, with state-of-the-art technology to address public sanitation challenges. Smart toilets work on a sensor-based technology. The self-cleaning and water conservation mechanism in the toilet makes it unique. In addition, there are features such as coin-operated door, sensor-based light system, auto flush, solar powered, self-clean every 10 uses, bio fuels output, etc. To monitor these connected Smart Toilets spread across regions and cities, a SAP Connected Goods solution is prototyped here that will control, optimize and automate functions and maximize the true value of our Smart Toilets. 1 © SAP SE or an SAP affiliate company. All rights reserved. Persona Mr. Lava Tory Civic Head “I would like to improve the sanitation needs of the general public, ensuring a cleaner and healthy environment.” About • 42 year old male, married, has 2 kids. -

Quaternary Ammonium Compounds
FACT SHEET: Quaternary Ammonium Compounds Quaternary ammonium compounds, also known as “quats” or “QACs,” include a number of chemicals used as sanitizers and disinfectants, including benzalkonium chloride, benzethonium chloride, cetalkonium chloride, cetrimide, cetrimonium bromide, cetylpyridinium chloride, glycidyl trimethyl, ammonium chloride, and stearalkonium chloride.[i] In general, quats cause toxic effects through all Mutagenicity routes of exposure including inhalation, Some quats have shown to be mutagenic and to ingestion, dermal application, and irrigation of damage animal DNA and DNA in human body cavities. Exposure to diluted solutions may lymphocytes at much lower levels than are result in mild irritation, while concentrated present in cleaning chemicals.[6] solutions are corrosive, causing burns to the skin and mucous Membranes. They can produce Antimicrobial Resistance systemic toxicity and can also cause allergic Genes have been discovered that mediate reactions.[2] resistance to quats. There has been an association of some of these genes with beta lactamase genes, Asthma and Allergies raising concern for a relationship between Of particular interest with regard to use as disinfectant resistance and antibiotic resistance.[7] disinfectants in the COVID-19 pandemic, quats increase the risk for asthma and allergic Reproductive Toxicity sensitization. Evidence from occupational Mice whose cages were cleaned with QACs had exposures shows increased risk of rhinitis and very low fertility rates. [8] Exposure to a common asthma -
Evaluating Disinfectants for Use Against the COVID-19 Virus
When it comes to choosing a disinfectant to combat the COVID-19 virus, research and health authorities suggest not all disinfectants are equally effective. The difference is in their active ingredient(s). HEALTH CANADA AND U.S. EPA ASSESSMENTS The work to evaluate disinfectants perhaps best starts with lists of approved disinfectants compiled by government health authorities. Health Canada has compiled a list of 85 hard surface disinfectant products (as of March 20, 2020) that meet their requirements for disinfection of emerging pathogens, including the virus that causes COVID-19. It can be accessed here. You can wade through the entire list. But if you locate the Drug Identification Number (DIN) on the disinfectant product label or the safety data sheet (SDS), then you can use the search function to quickly see if the product meets Health Canada requirements. A second list, updated on March 19, 2020, provides 287 products that meet the U.S. Environmental Protection Agency’s (EPA) criteria for use against SARS-CoV-2, the novel coronavirus that causes the disease COVID-19. This list can be found here. Like the Health Canada list, you can wade through this one too. However, to best use this list, you should locate the U.S. EPA registration number on the product label or SDS, and use that number to search the list. The U.S. EPA registration number of a product consists of two sets of numbers separated by a hyphen. The first set of numbers refers to the company identification number, and the second set of numbers following the hyphen represents the product number. -

Antimicrobial Activity of Cationic
ANTIMICROBIAL ACTIVITY OF CATIONIC ANTISEPTICS IN LAYER-BY-LAYER THIN FILM ASSEMBLIES A Thesis by CHARLENE MYRIAH DVORACEK Submitted to the Office of Graduate Studies of Texas A&M University in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE May 2009 Major Subject: Mechanical Engineering ANTIMICROBIAL ACTIVITY OF CATIONIC ANTISEPTICS IN LAYER-BY-LAYER THIN FILM ASSEMBLIES A Thesis by CHARLENE MYRIAH DVORACEK Submitted to the Office of Graduate Studies of Texas A&M University in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Approved by: Chair of Committee, Jaime Grunlan Committee Members, Michael Benedik Xinghang Zhang Head of Department, Dennis O'Neal May 2009 Major Subject: Mechanical Engineering iii ABSTRACT Antimicrobial Activity of Cationic Antiseptics in Layer-by-Layer Thin Film Assemblies. (May 2009) Charlene Myriah Dvoracek, B.S., Rose-Hulman Institute of Technology Chair of Advisory Committee: Dr. Jaime Grunlan Layer-by-layer (LbL) assembly has proven to be a powerful technique for assembling thin films with a variety of properties including electrochromic, molecular sensing, oxygen barrier, and antimicrobial. LbL involves the deposition of alternating cationic and anionic ingredients from solution, utilizing the electrostatic charges to develop multilayer films. The present work incorporates cationic antimicrobial agents into the positively-charged layers of LbL assemblies. When these thin films are exposed to a humid environment, the antimicrobial molecules readily diffuse out and prevent bacterial growth. The influence of exposure time, testing temperature, secondary ingredients and number of bilayers on antimicrobial efficacy is evaluated here. Additionally, film growth and microstructure are analyzed to better understand the behavior of these films. -
ANTT Guidelines
www.antt.org ANTT Guidelines The ANTT Clinical Guideline for the Preparation & Administration of Peripheral and Central Intravenous Medications (IV Therapy) Rationale and supporting evidence ANTT IV Prep and Administration V3 .0 2013 The Association for Safe Aseptic Technique (ASAP) www.antt.org www.antt .org ® © 2013 Aseptic Non Touch Technique (ANTT) This document is a publication of The-ASAP and all rights of copyright, intellectual property and Trademark are reserved. ANTT is protected to prevent dilution and misrepresentation of the practice framework so as to avoid ANTT becoming another unhelpful generic term for aseptic technique that is variably interpreted. For guidance see [email protected]. This document may however, be freely reviewed, copied and translated, in part, or in whole, for LOCAL, SINGLE ORGANIZATION educational use. It must not be published via the www/internet or its content used for production and publication of dedicated ANTT e-learning resources. ANTT is not for sale or for use in conjunction with commercial purposes. The-ASAP provide a number of free core ANTT resources to help disseminate and train healthcare staff. The- ASAP requests that the balance it determines between free dissemination and protection of the standard is respected in the interests of patient safety. Disclaimer: The-ASAP provides the ANTT Clinical Practice Framework and ANTT Clinical Guidelines to healthcare organizations in good faith in a collaboration to promote effective aseptic technique. It is the responsibility of healthcare organizations to implement ANTT effectively. No guarantee or responsibility for the application or outcome of clinical practice can be, or is, assumed or accepted by The-ASAP/ANTT. -

FDA-2015-N-0101; and FDA-2016-N-0124
DE PARTMENT OF HEALTH AND HUMAN SERVICES Food and Drug Administration Silver Spring MD 20993 November 18, 2020 Docket Nos. FDA-1975-N-0012; FDA-2015-N-0101; and FDA-2016-N-0124 The American Cleaning Institute Attention: James Kim, PhD Vice President, Science and Regulatory Affairs 1401 H Street, N.W. Suite 700 Washington, D.C. 20005 Re: Benzalkonium Chloride, Benzethonium Chloride, Chloroxylenol, Ethanol, and Povidone-Iodine Dear Dr. Kim: This letter responds to The American Cleaning Institute’s (ACI’s) July 14, 2020 communication regarding the deferral from final rulemaking under the over-the-counter (OTC) Drug Review on benzalkonium chloride, benzethonium chloride, chloroxylenol, ethanol, and povidone-iodine for use in nonprescription (often referred to as over-the-counter or OTC) consumer antiseptic wash, health care antiseptic, and consumer antiseptic rub drug products. In March 2016, FDA issued letters granting requests to defer three active ingredients— benzalkonium chloride, benzethonium chloride, and chloroxylenol—from inclusion in the final rulemaking for the December 2013 proposed rule for OTC consumer antiseptic washes (78 FR 76444). Similarly, in January 2017, FDA issued letters granting requests to defer six active ingredients—benzalkonium chloride, benzethonium chloride, chloroxylenol, ethanol, povidone- iodine, and isopropyl alcohol—from inclusion in the final rulemaking for the May 2015 proposed rule for OTC health care antiseptics (80 FR 25166). In October 2017, FDA issued letters granting requests to defer three active -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Reseptregisteret 2013–2017 the Norwegian Prescription Database
LEGEMIDDELSTATISTIKK 2018:2 Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Christian Berg Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Utgitt av Folkehelseinstituttet/Published by Norwegian Institute of Public Health Område for Helsedata og digitalisering Avdeling for Legemiddelstatistikk Juni 2018 Tittel/Title: Legemiddelstatistikk 2018:2 Reseptregisteret 2013–2017 / The Norwegian Prescription Database 2013–2017 Forfattere/Authors: Christian Berg, redaktør/editor Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Acknowledgement: Julie D. W. Johansen (English text) Bestilling/Order: Rapporten kan lastes ned som pdf på Folkehelseinstituttets nettsider: www.fhi.no The report can be downloaded from www.fhi.no Grafisk design omslag: Fete Typer Ombrekking: Houston911 Kontaktinformasjon/Contact information: Folkehelseinstituttet/Norwegian Institute of Public Health Postboks 222 Skøyen N-0213 Oslo Tel: +47 21 07 70 00 ISSN: 1890-9647 ISBN: 978-82-8082-926-9 Sitering/Citation: Berg, C (red), Reseptregisteret 2013–2017 [The Norwegian Prescription Database 2013–2017] Legemiddelstatistikk 2018:2, Oslo, Norge: Folkehelseinstituttet, 2018. Tidligere utgaver / Previous editions: 2008: Reseptregisteret 2004–2007 / The Norwegian Prescription Database 2004–2007 2009: Legemiddelstatistikk 2009:2: Reseptregisteret 2004–2008 / The Norwegian Prescription Database 2004–2008 2010: Legemiddelstatistikk 2010:2: Reseptregisteret 2005–2009. Tema: Vanedannende legemidler / The Norwegian Prescription Database 2005–2009.