Optimal Starting Point for Fifth Metatarsal Zone
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Patellofemoral Syndrome: Evaluation & Management Scott Sevinsky MSPT
Patellofemoral Syndrome: Evaluation & Management Scott Sevinsky MSPT What is Patellofemoral Syndrome? Patellofemoral syndrome (PFS) is a term commonly used to describe a condition where the patella ‘tracks’ or glides improperly between the femoral condyles. This improper tracking causes pain in the anterior knee and may lead to degenerative changes or dislocation of the knee cap. To be more precise the term ‘anterior knee pain’ is suggested to encompass all pain-related problems of the anterior part of the knee. By excluding anterior knee pain due to intra-articular pathology, peripatellar tendinitis or bursitis, plica syndromes, Sinding Larsen’s disease, Osgood Schlatter’s disease, neuromas and other rarely occurring pathologies it is suggested that remaining patients with a clinical presentation of anterior knee pain could be diagnosed with PFPS. The term ‘patellofemoral’ is used as no distinction can be made as to which specific structure of the patella or femur is affected. The term ‘chondromalacia patellae’, defined at the beginning of the 20th century to describe pathological changes of the retropatellar cartilage,7,8 was for half a century, used as a synonym for the syndrome of patellofemoral pain. However, several studies during the last 2 decades have shown a poor correlation between articular cartilage damage and the still not well-defined pain mechanism of retropatellar pain. Review of Knee Anatomy 1. Femur – thigh bone; longest bone in the body. · Lateral femoral condyle larger than medial condyle & projects farther anteriorly. · Medial femoral condyle longer anterior to posterior · Distal surfaces are convex · Intercondylar (trochlear) notch: groove in which the patella glides or ‘tracks’ 2. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Luxating Patella
LUXATING PATELLA What is a luxating patella? The patella, or kneecap, is normally located in the center of the knee joint. The term luxating means, “out of place” or “dislocated”. Therefore, a luxating patella is a kneecap that moves out of its normal location. What causes this? The muscles of the thigh attach to the top of the kneecap. There is a ligament, the patellar ligament, running from the bottom of the kneecap to a point on the tibia just below the knee joint. When the thigh muscles contract, force is transmitted through the patella and patellar ligament to a point on the top of the tibia. This results in extension or straightening of the knee. The patella stays in the center of the leg because the point of attachment of the patellar ligament is on the midline and because the patella slides in a groove on the lower end of the femur (the bone between the knee and the hip). The patella luxates because the point of attachment of the patellar ligament is not on the midline of the tibia. It is almost always located too far medial (toward the middle of the body). As the thigh muscles contract, the force is pulled medial. After several months or years of this abnormal movement, the inner side of the groove in the femur wears down. Once the side of the groove wears down, the patella is then free to dislocate. When this occurs, the dog has difficulty bearing weight on the leg. It may learn how to kick the leg and snap the patella back into its normal location. -
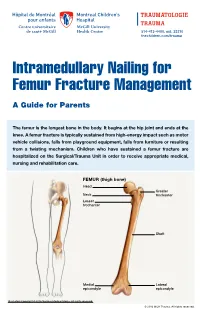
Intramedullary Nailing for Femur Fracture Management a Guide for Parents
514-412-4400, ext. 23310 thechildren.com/trauma Intramedullary Nailing for Femur Fracture Management A Guide for Parents The femur is the longest bone in the body. It begins at the hip joint and ends at the knee. A femur fracture is typically sustained from high-energy impact such as motor vehicle collisions, falls from playground equipment, falls from furniture or resulting from a twisting mechanism. Children who have sustained a femur fracture are hospitalized on the Surgical/Trauma Unit in order to receive appropriate medical, nursing and rehabilitation care. FEMUR (thigh bone) Head Greater Neck trochanter Lesser trochanter Shaft Medial Lateral epicondyle epicondyle Illustration Copyright © 2016 Nucleus Medical Media, All rights reserved. © 2016 MCH Trauma. All rights reserved. FEMUR FRACTURE MANAGEMENT The pediatric Orthopedic Surgeon will assess your child in order to determine the optimal treatment method. Treatment goals include: achieving proper bone realignment, rapid healing, and the return to normal daily activities. The treatment method chosen is primarily based on the child’s age but also taken into consideration are: fracture type, location and other injuries sustained if applicable. Prior to the surgery, your child may be placed in skin traction. This will ensure the bone is in an optimal healing position until it is surgically repaired. Occasionally, traction may be used for a longer period of time. The surgeon will determine if this management is needed based on the specific fracture type and/or location. ELASTIC/FLEXIBLE INTRAMEDULLARY NAILING This surgery is performed by the Orthopedic Surgeon in the Operating Room under general anesthesia. The surgeon will usually make two small incisions near the knee joint in order to insert two flexible titanium rods (intramedullary nails) Flexible through the femur. -

Unilateral Proximal Focal Femoral Deficiency, Fibular Aplasia, Tibial
The Egyptian Journal of Medical Human Genetics (2014) 15, 299–303 Ain Shams University The Egyptian Journal of Medical Human Genetics www.ejmhg.eg.net www.sciencedirect.com CASE REPORT Unilateral proximal focal femoral deficiency, fibular aplasia, tibial campomelia and oligosyndactyly in an Egyptian child – Probable FFU syndrome Rabah M. Shawky a,*, Heba Salah Abd Elkhalek a, Shaimaa Gad a, Shaimaa Abdelsattar Mohammad b a Pediatric Department, Genetics Unit, Ain Shams University, Egypt b Radio Diagnosis Department, Ain Shams University, Egypt Received 2 March 2014; accepted 18 March 2014 Available online 30 April 2014 KEYWORDS Abstract We report a fifteen month old Egyptian male child, the third in order of birth of healthy Short femur; non consanguineous parents, who has normal mentality, normal upper limbs and left lower limb. Limb anomaly; The right lower limb has short femur, and tibia with anterior bowing, and an overlying skin dimple. FFU syndrome; The right foot has also oligosyndactyly (three toes), and the foot is in vulgus position. There is lim- Proximal focal femoral ited abduction at the hip joint, full flexion and extension at the knee, limited dorsiflexion and plan- deficiency; tar flexion at the ankle joint. The X-ray of the lower limb and pelvis shows proximal focal femoral Fibular aplasia; deficiency, absent right fibula with shortening of the right tibia and anterior bowing of its distal Tibial campomelia; third. The acetabulum is shallow. He has a family history of congenital cyanotic heart disease. Oligosyndactyly Our patient represents most probably the first case of femur fibula ulna syndrome (FFU) in Egypt with unilateral right leg affection. -

Bones Can Tell Us More Compiled By: Nancy Volk
Bones Can Tell Us More Compiled By: Nancy Volk Strong Bones Sometimes only a few bones are found in a location in an archeological dig. VOCABULARY A few bones can tell about the height of a person. This is possible due to the Femur ratios of the bones. It has been determined that there are relationships between the femur, tibia, humerus, and radius and a person’s height. Humerus Radius Here is a little help to identify these four bones and formulas to assist with Tibia determining the height of a person based on bone length. Humerus Femur: Humerus: The thigh is the region of the femur. The arm bone most people call the From the hip bone to the knee bone. upper arm. It is found from the elbow to the shoulder joints. Inside This Packet Radius Strong Bones 1 New York State Standards 1 Activity: Bone Relationships 2 Information for the Teacher 4 Tibia: Radius: The larger and stronger of the two bones The bone found in the forearm that New York State Standards in the leg below the knee bone. extends from the side of the elbow to Middle School In vertebrates It is recognized as the the wrist. Standard 4: Living Environment strongest weight bearing bone in the Idea 1: 1.2a, 1.2b, 1.2e, 1.2f body. Life Sciences - Post Module 3 Middle School Page 1 Activity: Bone Relationships MATERIALS NEEDED Skeleton Formulas: Tape Measure Bone relationship is represented by the following formulas: Directions and formulas P represents the person’s height. The last letter of each formula stands for the Calculator known length of the bone (femur, tibia, humerus, or radius) through measurement. -

Normative Values for Femoral Length, Tibial Length, Andthe Femorotibial
Article Normative Values for Femoral Length, Tibial Length, and the Femorotibial Ratio in Adults Using Standing Full-Length Radiography Stuart A Aitken MaineGeneral Medical Center, 35 Medical Center Parkway, Augusta, ME 04330, USA; [email protected] Abstract: Knowledge of the normal length and skeletal proportions of the lower limb is required as part of the evaluation of limb length discrepancy. When measuring limb length, modern standing full-length digital radiographs confer a level of clinical accuracy interchangeable with that of CT imaging. This study reports a set of normative values for lower limb length using the standing full-length radiographs of 753 patients (61% male). Lower limb length, femoral length, tibial length, and the femorotibial ratio were measured in 1077 limbs. The reliability of the measurement method was tested using the intra-class correlation (ICC) of agreement between three observers. The mean length of 1077 lower limbs was 89.0 cm (range 70.2 to 103.9 cm). Mean femoral length was 50.0 cm (39.3 to 58.4 cm) and tibial length was 39.0 cm (30.8 to 46.5 cm). The median side-to-side difference was 0.4 cm (0.2 to 0.7, max 1.8 cm) between 324 paired limbs. The mean ratio of femoral length to tibial length for the study population was 1.28:1 (range 1.16 to 1.39). A moderately strong inverse linear relationship (r = −0.35, p < 0.001, Pearson’s) was identified between tibial length and the Citation: Aitken, S.A. Normative corresponding femorotibial ratio. -

Congenital Abnormalities of the Femur
Arch Dis Child: first published as 10.1136/adc.36.188.410 on 1 August 1961. Downloaded from CONGENITAL ABNORMALITIES OF THE FEMUR BY P. A. RING From the Royal College of Surgeons (RECEIVED FOR PUBLICATION NOVEMBER 25, 1960) Congenital defects of the femur vary from simple tion of its incidence is difficult to obtain, but it hypoplasia of the bone to complete absence. appears to be the commonest congenital defect Classification of these defects has been suggested causing major abnormalities of limb growth. by Nilsonne (1928) and by Mouchet and Ibos (1928), but neither has met with general acceptance. In more recent years Golding (1939, 1948) has demon- Clinical Features strated the close association of the short femur with There is no evidence that this is a familial disorder, congenital coxa vara, and has emphasized that and careful inquiry of the parents has revealed no these are variations of the same underlying abnor- evidence of other congenital disorders within the mality. The clinical distinction between the various immediate family. The history of the pregnancy types of femoral defect is important as a guide to and delivery has failed to indicate any significant the prognosis of limb development. infection or abnormality at this time. In most From an examination of patients with congenital patients the abnormality is apparent at birth, but abnormalities of the femur the following classifica- where the inequality of leg length is slight, the by copyright. tion is suggested: diagnosis may not be made until the child begins to 1. Simple femoral hypoplasia. walk. To ordinary clinical testing the abnormality 2. -

Case Report: Atypical Metatarsal Fracture in a Patient on Long- Term Bisphosphonate Therapy
November 2019. Volume 6. Number 4 Case Report: ATypical Metatarsal Fracture in a Patient on Long- Term Bisphosphonate Therapy Bijan Valiollahi1 , Mostafa Salehpour1 , Hamidreza Bashari1 , Shoeib Majdi1 , Mehdi Mohammadpour1 * 1. Bone and Joint Reconstruction Research Center, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran. Use your device to scan and read the article online Citation Valiollahi B, Salehpour M, Bashari H, Majdi Sh, Mohammadpour M. ATypical Metatarsal Fracture in a Patient on Long-Term Bisphosphonate Therapy. Journal of Research in Orthopedic Science. 2019; 6(4):25-30. http://dx.doi.org/10.32598/ JROSJ.6.4.67 : http://dx.doi.org/10.32598/JROSJ.6.4.67 A B S T R A C T Bisphosphonates, more particularly alendronate, are a popular category of drugs in the treatment Article info: of postmenopausal and corticosteroid-induced osteoporosis. The present study contends that the Received: 13 May 2019 long-term consumption of bisphosphonates causes not only subtrochanteric and femoral shaft Revised: 27 May 2019 fractures but also pathological fractures at other musculoskeletal sites. This report presents a Accepted: 16 Sep 2019 rare case of alendronate-induced pathological metatarsal fracture in a 59-year-old female with a Available Online: 01 Nov 2019 history of cuboid fracture following a twisting with abnormal Bone Mineral Density (BMD) (T score: −3.5; lumbar spine and −2.6; proximal femur). Keywords: Alendronate, Pathologic Fracture, Metatarsal 1. Introduction ally, drugs such as bisphosphonates contribute to devel- oping bone fractures. tress fractures occur as a result of repetitive loading and unloading of a bone [1]. In- Bisphosphonates are preferred drugs in postmenopaus- creased strain or frequency of compression al and corticosteroid-induced osteoporosis [6]. -

Periprosthetic Fractures
Periprosthetic Fractures SRS 2017 Stephen R Smith Orthopaedic Surgeon Northeast Nebraska Orthopaedics P C Norfolk Nebraska SRS 2017 Periprosthetic Fractures Fractures around Joint Replacements Mostly Lower Limb Knee Arthroplasty 700,000/ yr. Hip Arthroplasty 350,000/yr. Shoulder Arthroplasty ? 60,000/yr. Elbow Arthroplasty ? 20,000/yr. Periprosthetic Fractures Incidence Increasing due Increasing Demand and High Demands of Older Patients Projections 2025 2,000,000 (2 million) Knee Replacements 750,000 Total Hip Replacements Periprosthetic Fractures Risk Factors Mechanical Patient Factors Implant Loosening Rheumatoid Arthritis Chronic Steroid Use Neurologic Osteolysis Disease/Disorders Osteoporosis Osteopenia Femoral Notching Female Gender (Above TKA) Increasing Age SRS 2017 Periprosthetic Fractures Incidence Hip Intraoperative Acetabulum Cemented 0.2% Uncemented 0.4% During Impaction Under reaming> 2mm, Osteoporosis, Dysplasia Radiation Periprosthetic Fractures Incidence Hip Intraoperative Primary 0.1-5% Classification Osteoporosis,Cementless, Technique, Revision, Minimally Invasive, Revision 3-21% Periprosthetic Fractures Risk Factors DON’T FALL Remove Loose Rugs Minimize Stair Use Rail Stay Home in Bad Weather!!! Use Common Sense SRS 2017 Periprosthetic Fractures Risk Factors This Is Ice DON’T FALL Remove Loose Rugs Minimize Stair Use Rail Stay Home in Bad Weather!!! Use Common Sense SRS 2017 Periprosthetic Fractures Incidence Knee Intraoperative ?? Occasional Medial Femoral Condyle Often Tibial Crack after Stem Impaction Postoperative -

Fracture of the Lesser Trochanter As a Sign of Undiagnosed Tumor Disease in Adults Christian Herren*, Christian D
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Springer - Publisher Connector Herren et al. Eur J Med Res (2015) 20:72 DOI 10.1186/s40001-015-0167-8 CASE REPORT Open Access Fracture of the lesser trochanter as a sign of undiagnosed tumor disease in adults Christian Herren*, Christian D. Weber, Miguel Pishnamaz, Thomas Dienstknecht, Philipp Kobbe, Frank Hildebrand and Hans‑Christoph Pape Abstract Isolated avulsion fractures of the pelvic ring are rare and occur predominantly in adolescent athletes. Isolated fractures of the lesser trochanter are reported to be pathognomic for tumor diseases in adults. We present a case of a female patient with an isolated avulsion of the lesser trochanter after treatment by her chiropractor. After staging exami‑ nation, we determine the diagnosis of a left-sided carcinoma of the mamma. Additional imaging shows multiple metastases in liver, spine and pelvis. Palliative therapy has started over the course of time. We suggest, on suspicion of a malignant metastatic process, further investigation. Keywords: Fracture, Lesser trochanter, Metastatic, Tumor disease Background described unexplained weight loss of 5 kg in 4 months. Isolated fractures of the lesser trochanter are uncommon Sporadic onset of night sweats was also reported. She had and have been reported predominantly in adolescent ath- no other musculoskeletal or constitutional diseases in her letes [1]. This injury is caused by severe impact, usually medical history. Physical examination showed tenderness in context of contact sports and following a forceful and in the right groin, almost preserved passive mobility of sudden muscle contraction of the iliopsoas with avulsion the right hip joint in the full range of motion. -

Supplementary Table 1: Description of All Clinical Tests Test Protocol
Supplementary Table 1: Description of all clinical tests Test Protocol description Tibiofemoral • Palpate & mark tibial tuberosity & midpoint over the talus neck frontal plane • Ask participant to stand on footprint map with foot at 10° external rotation, feet shoulder width, looking alignment forward, 50% weightbearing • Place callipers of inclinometer in alignment with the the two landmarks • Record varus/valgus direction in degrees Herrington test • Participant supine on plinth, knee positioned and supported in 20° of knee flexion (to place the patella within the trochlea groove) • With knee in position, place a piece of 1” Leukotape (or similar) across the knee joint, and mark the medial and lateral epicondyles of the femur and mid-point of the patella. Be sure to make note of medial and lateral end of tape • Repeat 3 times, attaching tape to this document for measuring later 30 second chair • Shoes on, middle of chair, feet ~ shoulder width apart and slightly behind knees with feet flat on floor, stand test arms crossed on chest • Instructions “stand up keeping arms across chest, and ensure you stand completely up so hips and knees are fully extended; then sit completely back down, so that the bottom fully touches the seat, as many times as possible in 30 seconds,” • 1-2 practice repetitions for technique • One 30-second test trial • Record number of correctly performed full stands (if more than ½ of way up at end of the test, counted as a full stand) Repetitive single • Shoes on, seated on edge of plinth, foot placed with heel 10 cm forward from a plumb line at edge of leg rise test plinth, other leg held at side of body, arms across chest.