Patell O Medical Term
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Knee Flow Chart Acute
Symptom chart for acute knee pain START HERE Did the knee pain begin Does the knee joint You may have a fracture or Stop what you are doing immediately and go to a hospital emergency room YES YES suddenly, with an injury, appear deformed, or dislocated patella. or an orthopedic surgeon specializing in knee problems. slip, fall, or collision? out of position? If possible, splint the leg to limit the movement of the knee until you reach NO the doctor. Do not put any weight on the knee. Use a wheelchair, a cane, or NO crutch to prevent putting any weight on the leg, which might cause further damage to the joint. GO TO FLOW CHART #2 Go to an orthopedic surgeon Stop what you are doing. Continuing activity despite the feeling that the knee ON CHRONIC KNEE Did you hear a “pop” YES immediately, you may have is unstable can cause additional damage to other ligaments, meniscus , and PROBLEMS THAT DEVELOP and does your knee feel torn your anterior cruciate, or cartilage. Try ice on the knee to control swelling. Take anti-in ammatories OR WORSEN OVER TIME. unstable or wobbly? other ligaments in the knee. like Advil or Nuprin until your doctor’s appointment. About a third of ligament tears get better with exercises, a third may need a brace, and a third may need sur gery. NO Use R•I•C•E for sore knees Does your knee hurt YES You may have damaged the articular Try anti-in ammatories, as directed on the bottle, for two days to reduce R: Rest as you bend it? cartilage on the bottom of the the chronic in ammation. -

Patellofemoral Syndrome: Evaluation & Management Scott Sevinsky MSPT
Patellofemoral Syndrome: Evaluation & Management Scott Sevinsky MSPT What is Patellofemoral Syndrome? Patellofemoral syndrome (PFS) is a term commonly used to describe a condition where the patella ‘tracks’ or glides improperly between the femoral condyles. This improper tracking causes pain in the anterior knee and may lead to degenerative changes or dislocation of the knee cap. To be more precise the term ‘anterior knee pain’ is suggested to encompass all pain-related problems of the anterior part of the knee. By excluding anterior knee pain due to intra-articular pathology, peripatellar tendinitis or bursitis, plica syndromes, Sinding Larsen’s disease, Osgood Schlatter’s disease, neuromas and other rarely occurring pathologies it is suggested that remaining patients with a clinical presentation of anterior knee pain could be diagnosed with PFPS. The term ‘patellofemoral’ is used as no distinction can be made as to which specific structure of the patella or femur is affected. The term ‘chondromalacia patellae’, defined at the beginning of the 20th century to describe pathological changes of the retropatellar cartilage,7,8 was for half a century, used as a synonym for the syndrome of patellofemoral pain. However, several studies during the last 2 decades have shown a poor correlation between articular cartilage damage and the still not well-defined pain mechanism of retropatellar pain. Review of Knee Anatomy 1. Femur – thigh bone; longest bone in the body. · Lateral femoral condyle larger than medial condyle & projects farther anteriorly. · Medial femoral condyle longer anterior to posterior · Distal surfaces are convex · Intercondylar (trochlear) notch: groove in which the patella glides or ‘tracks’ 2. -

Autologous Matrix-Induced Chondrogenesis and Generational Development of Autologous Chondrocyte Implantation
Autologous Matrix-Induced Chondrogenesis and Generational Development of Autologous Chondrocyte Implantation Hajo Thermann, MD, PhD,* Christoph Becher, MD,† Francesca Vannini, MD, PhD,‡ and Sandro Giannini, MD‡ The treatment of osteochondral defects of the talus is still controversial. Matrix-guided treatment options for covering of the defect with a scaffold have gained increasing popularity. Cellular-based autologous chondrocyte implantation (ACI) has undergone a generational development overcoming the surgical drawbacks related to the use of the periosteal flap over time. As ACI is associated with high costs and limited in availability, autologous matrix-induced chondrogenesis, a single-step procedure combining microfracturing of the subchondral bone to release bone marrow mesenchymal stem cells in combination with the coverage of an acellular matrix, has gained increasing popularity. The purposes of this report are to present the arthroscopic approach of the matrix-guided autologous matrix-induced chondrogenesis technique and generational development of ACI in the treatment of chondral and osteochon- dral defects of the talus. Oper Tech Orthop 24:210-215 C 2014 Elsevier Inc. All rights reserved. KEYWORDS cartilage, defect, ankle, talus, AMIC, ACI Introduction Cartilage repair may be obtained by cartilage replacement: (OATS, mosaicplasty) or with techniques aimed to generate a hondral and osteochondral lesions are defects of the newly formed cartilage such as microfracture or autologous Ccartilaginous surface and underlying subchondral bone of chondrocyte implantation (ACI).9-17 the talar dome. These defects are often caused by a single or Arthroscopic debridement and bone marrow stimulation multiple traumatic events, mostly inversion or eversion ankle using the microfracture technique has proven to be an 1,2 sprains in young, active patients. -

Knee Joint Distraction Compared with Total Knee Arthroplasty a RANDOMISED CONTROLLED TRIAL
KNEE Knee joint distraction compared with total knee arthroplasty A RANDOMISED CONTROLLED TRIAL J. A. D. van der Woude, Aims K. Wiegant, Knee joint distraction (KJD) is a relatively new, knee-joint preserving procedure with the R. J. van Heerwaarden, goal of delaying total knee arthroplasty (TKA) in young and middle-aged patients. We S. Spruijt, present a randomised controlled trial comparing the two. P. J. E m ans , Patients and Methods S. C. Mastbergen, The 60 patients ≤ 65 years with end-stage knee osteoarthritis were randomised to either F. P. J. G. Lafeber KJD (n = 20) or TKA (n = 40). Outcomes were assessed at baseline, three, six, nine, and 12 months. In the KJD group, the joint space width (JSW) was radiologically assessed, From UMC Utrecht, representing a surrogate marker of cartilage thickness. Utrecht, The Netherlands Results In total 56 patients completed their allocated treatment (TKA = 36, KJD = 20). All patient reported outcome measures improved significantly over one year (p < 0.02) in both groups. J. A. D. van der Woude, MD, At one year, the TKA group showed a greater improvement in only one of the 16 patient- PhD, Resident in Orthopaedic Surgery, Limb and Knee related outcome measures assessed (p = 0.034). Outcome Measures in Rheumatology- Reconstruction Unit, Department of Orthopaedic Osteoarthritis Research Society International clinical response was 83% after TKA and 80% Surgery after KJD. A total of 12 patients (60%) in the KJD group sustained pin track infections. In the R. J. van Heerwaarden, MD, PhD, Orthopaedic Surgeon, KJD group both mean minimum (0.9 mm, standard deviation (SD) 1.1) and mean JSW (1.2 mm, Limb and Knee Reconstruction Unit, Department of SD 1.1) increased significantly (p = 0.004 and p = 0.0003). -

Medical Terminology Abbreviations Medical Terminology Abbreviations
34 MEDICAL TERMINOLOGY ABBREVIATIONS MEDICAL TERMINOLOGY ABBREVIATIONS The following list contains some of the most common abbreviations found in medical records. Please note that in medical terminology, the capitalization of letters bears significance as to the meaning of certain terms, and is often used to distinguish terms with similar acronyms. @—at A & P—anatomy and physiology ab—abortion abd—abdominal ABG—arterial blood gas a.c.—before meals ac & cl—acetest and clinitest ACLS—advanced cardiac life support AD—right ear ADL—activities of daily living ad lib—as desired adm—admission afeb—afebrile, no fever AFB—acid-fast bacillus AKA—above the knee alb—albumin alt dieb—alternate days (every other day) am—morning AMA—against medical advice amal—amalgam amb—ambulate, walk AMI—acute myocardial infarction amt—amount ANS—automatic nervous system ant—anterior AOx3—alert and oriented to person, time, and place Ap—apical AP—apical pulse approx—approximately aq—aqueous ARDS—acute respiratory distress syndrome AS—left ear ASA—aspirin asap (ASAP)—as soon as possible as tol—as tolerated ATD—admission, transfer, discharge AU—both ears Ax—axillary BE—barium enema bid—twice a day bil, bilateral—both sides BK—below knee BKA—below the knee amputation bl—blood bl wk—blood work BLS—basic life support BM—bowel movement BOW—bag of waters B/P—blood pressure bpm—beats per minute BR—bed rest MEDICAL TERMINOLOGY ABBREVIATIONS 35 BRP—bathroom privileges BS—breath sounds BSI—body substance isolation BSO—bilateral salpingo-oophorectomy BUN—blood, urea, nitrogen -

About Your Knee
OrthoInfo Basics About Your Knee What are the parts of the knee? Your knee is Your knee is made up of four main things: bones, cartilage, ligaments, the largest joint and tendons. in your body Bones. Three bones meet to form your knee joint: your thighbone and one of the (femur), shinbone (tibia), and kneecap (patella). Your patella sits in most complex. front of the joint and provides some protection. It is also vital Articular cartilage. The ends of your thighbone and shinbone are covered with articular cartilage. This slippery substance to movement. helps your knee bones glide smoothly across each other as you bend or straighten your leg. Because you use it so Two wedge-shaped pieces of meniscal cartilage act as much, it is vulnerable to Meniscus. “shock absorbers” between your thighbone and shinbone. Different injury. Because it is made from articular cartilage, the meniscus is tough and rubbery to help up of so many parts, cushion and stabilize the joint. When people talk about torn cartilage many different things in the knee, they are usually referring to torn meniscus. can go wrong. Knee pain or injury Femur is one of the most (thighbone) common reasons people Patella (kneecap) see their doctors. Most knee problems can be prevented or treated with simple measures, such as exercise or Articular cartilage training programs. Other problems require surgery Meniscus to correct. Tibia (shinbone) 1 OrthoInfo Basics — About Your Knee What are ligaments and tendons? Ligaments and tendons connect your thighbone Collateral ligaments. These are found on to the bones in your lower leg. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Luxating Patella
LUXATING PATELLA What is a luxating patella? The patella, or kneecap, is normally located in the center of the knee joint. The term luxating means, “out of place” or “dislocated”. Therefore, a luxating patella is a kneecap that moves out of its normal location. What causes this? The muscles of the thigh attach to the top of the kneecap. There is a ligament, the patellar ligament, running from the bottom of the kneecap to a point on the tibia just below the knee joint. When the thigh muscles contract, force is transmitted through the patella and patellar ligament to a point on the top of the tibia. This results in extension or straightening of the knee. The patella stays in the center of the leg because the point of attachment of the patellar ligament is on the midline and because the patella slides in a groove on the lower end of the femur (the bone between the knee and the hip). The patella luxates because the point of attachment of the patellar ligament is not on the midline of the tibia. It is almost always located too far medial (toward the middle of the body). As the thigh muscles contract, the force is pulled medial. After several months or years of this abnormal movement, the inner side of the groove in the femur wears down. Once the side of the groove wears down, the patella is then free to dislocate. When this occurs, the dog has difficulty bearing weight on the leg. It may learn how to kick the leg and snap the patella back into its normal location. -

GLOSSARY of MEDICAL and ANATOMICAL TERMS
GLOSSARY of MEDICAL and ANATOMICAL TERMS Abbreviations: • A. Arabic • abb. = abbreviation • c. circa = about • F. French • adj. adjective • G. Greek • Ge. German • cf. compare • L. Latin • dim. = diminutive • OF. Old French • ( ) plural form in brackets A-band abb. of anisotropic band G. anisos = unequal + tropos = turning; meaning having not equal properties in every direction; transverse bands in living skeletal muscle which rotate the plane of polarised light, cf. I-band. Abbé, Ernst. 1840-1905. German physicist; mathematical analysis of optics as a basis for constructing better microscopes; devised oil immersion lens; Abbé condenser. absorption L. absorbere = to suck up. acervulus L. = sand, gritty; brain sand (cf. psammoma body). acetylcholine an ester of choline found in many tissue, synapses & neuromuscular junctions, where it is a neural transmitter. acetylcholinesterase enzyme at motor end-plate responsible for rapid destruction of acetylcholine, a neurotransmitter. acidophilic adj. L. acidus = sour + G. philein = to love; affinity for an acidic dye, such as eosin staining cytoplasmic proteins. acinus (-i) L. = a juicy berry, a grape; applied to small, rounded terminal secretory units of compound exocrine glands that have a small lumen (adj. acinar). acrosome G. akron = extremity + soma = body; head of spermatozoon. actin polymer protein filament found in the intracellular cytoskeleton, particularly in the thin (I-) bands of striated muscle. adenohypophysis G. ade = an acorn + hypophyses = an undergrowth; anterior lobe of hypophysis (cf. pituitary). adenoid G. " + -oeides = in form of; in the form of a gland, glandular; the pharyngeal tonsil. adipocyte L. adeps = fat (of an animal) + G. kytos = a container; cells responsible for storage and metabolism of lipids, found in white fat and brown fat. -
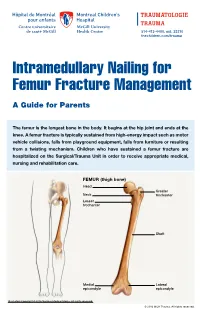
Intramedullary Nailing for Femur Fracture Management a Guide for Parents
514-412-4400, ext. 23310 thechildren.com/trauma Intramedullary Nailing for Femur Fracture Management A Guide for Parents The femur is the longest bone in the body. It begins at the hip joint and ends at the knee. A femur fracture is typically sustained from high-energy impact such as motor vehicle collisions, falls from playground equipment, falls from furniture or resulting from a twisting mechanism. Children who have sustained a femur fracture are hospitalized on the Surgical/Trauma Unit in order to receive appropriate medical, nursing and rehabilitation care. FEMUR (thigh bone) Head Greater Neck trochanter Lesser trochanter Shaft Medial Lateral epicondyle epicondyle Illustration Copyright © 2016 Nucleus Medical Media, All rights reserved. © 2016 MCH Trauma. All rights reserved. FEMUR FRACTURE MANAGEMENT The pediatric Orthopedic Surgeon will assess your child in order to determine the optimal treatment method. Treatment goals include: achieving proper bone realignment, rapid healing, and the return to normal daily activities. The treatment method chosen is primarily based on the child’s age but also taken into consideration are: fracture type, location and other injuries sustained if applicable. Prior to the surgery, your child may be placed in skin traction. This will ensure the bone is in an optimal healing position until it is surgically repaired. Occasionally, traction may be used for a longer period of time. The surgeon will determine if this management is needed based on the specific fracture type and/or location. ELASTIC/FLEXIBLE INTRAMEDULLARY NAILING This surgery is performed by the Orthopedic Surgeon in the Operating Room under general anesthesia. The surgeon will usually make two small incisions near the knee joint in order to insert two flexible titanium rods (intramedullary nails) Flexible through the femur. -

ANTERIOR KNEE PAIN Home Exercises
ANTERIOR KNEE PAIN Home Exercises Anterior knee pain is pain that occurs at the front and center of the knee. It can be caused by many different problems, including: • Weak or overused muscles • Chondromalacia of the patella (softening and breakdown of the cartilage on the underside of the kneecap) • Inflammations and tendon injury (bursitis, tendonitis) • Loose ligaments with instability of the kneecap • Articular cartilage damage (chondromalacia patella) • Swelling due to fluid buildup in the knee joint • An overload of the extensor mechanism of the knee with or without malalignment of the patella You may feel pain after exercising or when you sit too long. The pain may be a nagging ache or an occasional sharp twinge. Because the pain is around the front of your knee, treatment has traditionally focused on the knee itself and may include taping or bracing the kneecap, or patel- la, and/ or strengthening the thigh muscle—the quadriceps—that helps control your kneecap to improve the contact area between the kneecap and the thigh bone, or femur, beneath it. Howev- er, recent evidence suggests that strengthening your hip and core muscles can also help. The control of your knee from side to side comes from the glutes and core control; that is why those areas are so important in management of anterior knee pain. The exercises below will work on a combination of flexibility and strength of your knee, hip, and core. Although some soreness with exercise is expected, we do not want any sharp pain–pain that gets worse with each rep of an exercise or any increased soreness for more than 24 hours. -

Unilateral Proximal Focal Femoral Deficiency, Fibular Aplasia, Tibial
The Egyptian Journal of Medical Human Genetics (2014) 15, 299–303 Ain Shams University The Egyptian Journal of Medical Human Genetics www.ejmhg.eg.net www.sciencedirect.com CASE REPORT Unilateral proximal focal femoral deficiency, fibular aplasia, tibial campomelia and oligosyndactyly in an Egyptian child – Probable FFU syndrome Rabah M. Shawky a,*, Heba Salah Abd Elkhalek a, Shaimaa Gad a, Shaimaa Abdelsattar Mohammad b a Pediatric Department, Genetics Unit, Ain Shams University, Egypt b Radio Diagnosis Department, Ain Shams University, Egypt Received 2 March 2014; accepted 18 March 2014 Available online 30 April 2014 KEYWORDS Abstract We report a fifteen month old Egyptian male child, the third in order of birth of healthy Short femur; non consanguineous parents, who has normal mentality, normal upper limbs and left lower limb. Limb anomaly; The right lower limb has short femur, and tibia with anterior bowing, and an overlying skin dimple. FFU syndrome; The right foot has also oligosyndactyly (three toes), and the foot is in vulgus position. There is lim- Proximal focal femoral ited abduction at the hip joint, full flexion and extension at the knee, limited dorsiflexion and plan- deficiency; tar flexion at the ankle joint. The X-ray of the lower limb and pelvis shows proximal focal femoral Fibular aplasia; deficiency, absent right fibula with shortening of the right tibia and anterior bowing of its distal Tibial campomelia; third. The acetabulum is shallow. He has a family history of congenital cyanotic heart disease. Oligosyndactyly Our patient represents most probably the first case of femur fibula ulna syndrome (FFU) in Egypt with unilateral right leg affection.