Normative Values for Femoral Length, Tibial Length, Andthe Femorotibial
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Blount, Anteversion and Torsion: What's It All About?
Blount, Anteversion and Torsion: What’s it all about? Arthur B. Meyers, MD Assistant Professor of Radiology Children’s Hospital of WisConsin/ MediCal College of WisConsin Disclosures • Author for Amirsys/Elsevier, reCeiving royalGes Lower Extremity Alignment in Children • Lower extremity rotaGon – Femoral version / Gbial torsion – Normal values & CliniCal indiCaGons – Imaging • Blount disease – Physiologic bowing – Blount disease Lower Extremity RotaGonal Alignment Primarily determined by: 1. Femoral version 2. Tibial torsion 3. PosiGon of the foot Rosenfeld SB. Approach to the Child with in-toeing. Up-to-date. 2/2014 Lower Extremity RotaGonal Alignment Primarily determined by: 1. Femoral version 2. Tibial torsion 3. PosiGon of the foot Rosenfeld SB. Approach to the Child with in-toeing. Up-to-date. 2/2014 Femoral Version The rotaGon of the femoral neCk in relaGon to the long axis of the femur (posterior Condylar axis of the distal femur) Femoral Version The rotaGon of the femoral neCk in relaGon to the long axis of the femur (posterior Condylar axis of the distal femur) Femoral Version The rotaGon of the femoral neCk in relaGon to the long axis of the femur (posterior Condylar axis of the distal femur) Femoral Version The rotaGon of the femoral neCk in relaGon to the long axis of the femur (posterior Condylar axis of the distal femur) Femoral Version The rotaGon of the femoral neCk in relaGon to the long axis of the femur (posterior Condylar axis of the distal femur) Femoral Version The rotaGon of the femoral neCk in relaGon to the long -
Arthroscopic and Open Anatomy of the Hip 11
CHAPTER Arthroscopic and o'pen Anatomy of the Hip Michael B. Gerhardt, Kartik Logishetty, Morteza lV1eftah, and Anil S. Ranawat INTRODUCTION movements that they induce at the joint: 1) flexors; 2) extensors; 3) abductors; 4) adductors; 5) external rotators; and 6) interI12 I The hip joint is defined by the articulation between the head rotators. Although some muscles have dual roles, their primary of the femur and the aeetahulum of the pelvis. It is covered by functions define their group placem(:)nt, and they all have ullique :l large soft-tissue envelope and a complex array of neurovascu- neurovascular supplies (TIt ble 2-1). lar and musculotendinous structures. The joint's morphology The vascular supply of tbe hip stems from the external and anu orientation are complex, and there are wide anatomi c varia- internal iLiac ancries. An understanding of the course of these tions seen among individuals. The joint's deep location makes vessels is critical fo r ,lVo iding catasu"ophic vascular injury. fn both arthroscopic and open access challenging. To avoid iatro- addition, the blood supply to the fel11()ra l head is vulnerahle to genic injury while establishing functional and efficient access, both traumatic and iatrogenic injury; the disruption of this sup- the hip surgeon should possess a sound ana tomic knowledge of ply can result in avascular necrosis (Figure 2-2). the hip. T he human "hip" can be subdivided into three categories: I) the superficial surface anatomy; 2) the deep femoroacetabu- la r Joint and capsule; and 3) the associated structures, including the muscles, nerves, and vasculature, all of which directly affeet HIP MUSCULATURE its function. -

Patellofemoral Syndrome: Evaluation & Management Scott Sevinsky MSPT
Patellofemoral Syndrome: Evaluation & Management Scott Sevinsky MSPT What is Patellofemoral Syndrome? Patellofemoral syndrome (PFS) is a term commonly used to describe a condition where the patella ‘tracks’ or glides improperly between the femoral condyles. This improper tracking causes pain in the anterior knee and may lead to degenerative changes or dislocation of the knee cap. To be more precise the term ‘anterior knee pain’ is suggested to encompass all pain-related problems of the anterior part of the knee. By excluding anterior knee pain due to intra-articular pathology, peripatellar tendinitis or bursitis, plica syndromes, Sinding Larsen’s disease, Osgood Schlatter’s disease, neuromas and other rarely occurring pathologies it is suggested that remaining patients with a clinical presentation of anterior knee pain could be diagnosed with PFPS. The term ‘patellofemoral’ is used as no distinction can be made as to which specific structure of the patella or femur is affected. The term ‘chondromalacia patellae’, defined at the beginning of the 20th century to describe pathological changes of the retropatellar cartilage,7,8 was for half a century, used as a synonym for the syndrome of patellofemoral pain. However, several studies during the last 2 decades have shown a poor correlation between articular cartilage damage and the still not well-defined pain mechanism of retropatellar pain. Review of Knee Anatomy 1. Femur – thigh bone; longest bone in the body. · Lateral femoral condyle larger than medial condyle & projects farther anteriorly. · Medial femoral condyle longer anterior to posterior · Distal surfaces are convex · Intercondylar (trochlear) notch: groove in which the patella glides or ‘tracks’ 2. -

Skier Tibia (Leg) Fractures
Skier Tibia (Leg) Fractures In years past, the prototypical ski fracture was sustained at the lower part of the outside of the leg in the region of the ankle. However, in the past 10 years, with the advent of the modern ski boots and improvements in binding, the most commonly seen lower leg skier fracture is the tibia (or shinbone) fracture. 10% of these fractures are associated with a collision. Thus, 90 % are associated with an isolated fall or noncontact type of injury, which is generally the result of binding malfunctions and inappropriate release. The most common mechanism leading to a tibia (leg) fracture is a forward fall. Risk factors for sustaining a skier tibia fracture include: beginners or novice skiers, less than 20 years of age, higher outdoor temperatures, and increased snow depth. Non-risk factors include ski lengths, icy conditions, and male versus female sex. The modern ski boot very closely resembles an extremely well padded short leg cast in the treatment of many orthopaedic lower extremity fractures. It of course goes to a much higher level than the former shorter boot top-level varieties. The binding release and designs have been based on the fracture strength of the adult tibia (shin) bone at the top of the modern ski boot. The treatment of most skier leg fractures includes a closed reduction and cast application for variable periods of time, with or without weight bearing allowed. However, severe misalignments of the bones can lead to later bony prominences that may be incompatible with snug, rigid, high fitting ski boots. -

Assessment, Management and Decision Making in the Treatment Of
Pediatric Ankle Fractures Anthony I. Riccio, MD Texas Scottish Rite Hospital for Children Update 07/2016 Pediatric Ankle Fractures The Ankle is the 2nd most Common Site of Physeal Injury in Children 10-25% of all Physeal Injuries Occur About the Ankle Pediatric Ankle Fractures Primary Concerns Are: • Anatomic Restoration of Articular Surface • Restoration of Symmetric Ankle Mortise • Preservation of Physeal Growth • Minimize Iatrogenic Physeal Injury • Avoid Fixation Across Physis in Younger Children Salter Harris Classification Prognosis and Treatment of Pediatric Ankle Fractures is Often Dictated by the Salter Harris Classification of Physeal Fractures Type I and II Fractures: Often Amenable to Closed Tx / Lower Risk of Physeal Arrest Type III and IV: More Likely to Require Operative Tx / Higher Risk of Physeal Arrest Herring JA, ed. Tachdjian’s Pediatric Orthopaedics, 5th Ed. 2014. Elsevier. Philadelphia, PA. ISOLATED DISTAL FIBULA FRACTURES Distal Fibula Fractures • The Physis is Weaker than the Lateral Ankle Ligaments – Children Often Fracture the Distal Fibula but…. – …ligamentous Injuries are Not Uncommon • Mechanism of Injury = Inversion of a Supinated Foot • SH I and II Fractures are Most Common – SH I Fractures: Average Age = 10 Years – SH II Fractures: Average Age = 12 Years Distal Fibula Fractures Lateral Ankle Tenderness SH I Distal Fibula Fracture vs. Lateral Ligamentous Injury (Sprain) Distal Fibula Fractures • Sankar et al (JPO 2008) – 37 Children – All with Open Physes, Lateral Ankle Tenderness + Normal Films – 18%: Periosteal -

Femur Pelvis HIP JOINT Femoral Head in Acetabulum Acetabular
Anatomy of the Hip Joint Overview The hip joint is one of the largest weight-bearing HIP JOINT joints in the body. This ball-and-socket joint allows the leg to move and rotate while keeping the body Femoral head in stable and balanced. Let's take a closer look at the acetabulum main parts of the hip joint's anatomy. Pelvis Bones Two bones meet at the hip joint, the femur and the pelvis. The femur, commonly called the "thighbone," is the longest and heaviest bone of the body. At the top of the femur, positioned on the femoral neck, is the femoral head. This is the "ball" of the hip joint. The other part of the joint – the Femur "socket" – is found in the pelvis. The pelvis is a bone made of three sections: the ilium, the ischium and the pubis. The socket is located where these three sections fuse. The proper name of the socket is the "acetabulum." The head of the femur fits tightly into this cup-shaped cavity. Articular Cartilage The femoral head and the acetabulum are covered Acetabular with a layer of articular cartilage. This tough, smooth tissue protects the bones. It allows them to labrum glide smoothly against each other as the ball moves in the socket. Soft Tissues Several soft tissue structures work together to hold the femoral head securely in place. The acetabulum is surrounded by a ring of cartilage called the "acetabular labrum." This deepens the socket and helps keep the ball from slipping out of alignment. It also acts as a shock absorber. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Luxating Patella
LUXATING PATELLA What is a luxating patella? The patella, or kneecap, is normally located in the center of the knee joint. The term luxating means, “out of place” or “dislocated”. Therefore, a luxating patella is a kneecap that moves out of its normal location. What causes this? The muscles of the thigh attach to the top of the kneecap. There is a ligament, the patellar ligament, running from the bottom of the kneecap to a point on the tibia just below the knee joint. When the thigh muscles contract, force is transmitted through the patella and patellar ligament to a point on the top of the tibia. This results in extension or straightening of the knee. The patella stays in the center of the leg because the point of attachment of the patellar ligament is on the midline and because the patella slides in a groove on the lower end of the femur (the bone between the knee and the hip). The patella luxates because the point of attachment of the patellar ligament is not on the midline of the tibia. It is almost always located too far medial (toward the middle of the body). As the thigh muscles contract, the force is pulled medial. After several months or years of this abnormal movement, the inner side of the groove in the femur wears down. Once the side of the groove wears down, the patella is then free to dislocate. When this occurs, the dog has difficulty bearing weight on the leg. It may learn how to kick the leg and snap the patella back into its normal location. -
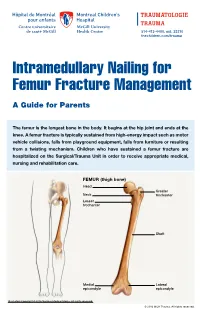
Intramedullary Nailing for Femur Fracture Management a Guide for Parents
514-412-4400, ext. 23310 thechildren.com/trauma Intramedullary Nailing for Femur Fracture Management A Guide for Parents The femur is the longest bone in the body. It begins at the hip joint and ends at the knee. A femur fracture is typically sustained from high-energy impact such as motor vehicle collisions, falls from playground equipment, falls from furniture or resulting from a twisting mechanism. Children who have sustained a femur fracture are hospitalized on the Surgical/Trauma Unit in order to receive appropriate medical, nursing and rehabilitation care. FEMUR (thigh bone) Head Greater Neck trochanter Lesser trochanter Shaft Medial Lateral epicondyle epicondyle Illustration Copyright © 2016 Nucleus Medical Media, All rights reserved. © 2016 MCH Trauma. All rights reserved. FEMUR FRACTURE MANAGEMENT The pediatric Orthopedic Surgeon will assess your child in order to determine the optimal treatment method. Treatment goals include: achieving proper bone realignment, rapid healing, and the return to normal daily activities. The treatment method chosen is primarily based on the child’s age but also taken into consideration are: fracture type, location and other injuries sustained if applicable. Prior to the surgery, your child may be placed in skin traction. This will ensure the bone is in an optimal healing position until it is surgically repaired. Occasionally, traction may be used for a longer period of time. The surgeon will determine if this management is needed based on the specific fracture type and/or location. ELASTIC/FLEXIBLE INTRAMEDULLARY NAILING This surgery is performed by the Orthopedic Surgeon in the Operating Room under general anesthesia. The surgeon will usually make two small incisions near the knee joint in order to insert two flexible titanium rods (intramedullary nails) Flexible through the femur. -

Unilateral Proximal Focal Femoral Deficiency, Fibular Aplasia, Tibial
The Egyptian Journal of Medical Human Genetics (2014) 15, 299–303 Ain Shams University The Egyptian Journal of Medical Human Genetics www.ejmhg.eg.net www.sciencedirect.com CASE REPORT Unilateral proximal focal femoral deficiency, fibular aplasia, tibial campomelia and oligosyndactyly in an Egyptian child – Probable FFU syndrome Rabah M. Shawky a,*, Heba Salah Abd Elkhalek a, Shaimaa Gad a, Shaimaa Abdelsattar Mohammad b a Pediatric Department, Genetics Unit, Ain Shams University, Egypt b Radio Diagnosis Department, Ain Shams University, Egypt Received 2 March 2014; accepted 18 March 2014 Available online 30 April 2014 KEYWORDS Abstract We report a fifteen month old Egyptian male child, the third in order of birth of healthy Short femur; non consanguineous parents, who has normal mentality, normal upper limbs and left lower limb. Limb anomaly; The right lower limb has short femur, and tibia with anterior bowing, and an overlying skin dimple. FFU syndrome; The right foot has also oligosyndactyly (three toes), and the foot is in vulgus position. There is lim- Proximal focal femoral ited abduction at the hip joint, full flexion and extension at the knee, limited dorsiflexion and plan- deficiency; tar flexion at the ankle joint. The X-ray of the lower limb and pelvis shows proximal focal femoral Fibular aplasia; deficiency, absent right fibula with shortening of the right tibia and anterior bowing of its distal Tibial campomelia; third. The acetabulum is shallow. He has a family history of congenital cyanotic heart disease. Oligosyndactyly Our patient represents most probably the first case of femur fibula ulna syndrome (FFU) in Egypt with unilateral right leg affection. -

Arthrodiastasis for Treatment of Avascular Necrosis of Lesser Metatarsal Heads
QUICK START GUIDE QUICK START GUIDE (THIS SIDEBAR WILL NOT PRINT) Arthrodiastasis for Treatment of Avascular Necrosis of Lesser Metatarsal Heads (THIS SIDEBAR WILL NOT PRINT) This PowerPoint template produces a 42”x90" presentation poster. You can use it to create your research poster by placing your title, subtitle, text, tables, charts and How to change the template colors photos. You can change the overall template color theme by clicking on the COLORS Stephanie Wu, DPM¹, Jones Thomas, DPM², Hummira Abawi, DPM, FACFAS³ dropdown menu under the DESIGN tab. You can see a tutorial here: We provide a series of online tutorials that will guide you through the poster design ¹ PGY-1, VA Maryland Healthcare System and Sinai Hospital, Baltimore, Rubin Institute for Advanced Orthopedics https://www.posterpresentations.com/how-to-change-the-research-poster-template-colors.h process and answer your poster production questions. For complete template tml tutorials, go online to PosterPresentations.com and click on the HELP DESK tab. ² PGY-2, VA Maryland Healthcare System and Sinai Hospital, Baltimore, Rubin Institute for Advanced Orthopedics You can also manually change the color of individual elements by going to VIEW > ³ Assistant Director, VA Maryland Healthcare System and Sinai Hospital, Baltimore, Rubin Institute for Advanced Orthopedics To print your poster using our same-day professional printing service, go online to SLIDE MASTER. On the left side of your screen select the background master where PosterPresentations.com and click on "Order your poster". you can change the template background, column sizes, etc. After you finish working on the SLIDE MASTER, it is important that you go to VIEW > NORMAL to continue working on your poster. -

Osteonecrosis of the Femoral Head. Surgical Technique Free
This is an enhanced PDF from The Journal of Bone and Joint Surgery The PDF of the article you requested follows this cover page. Free Vascularized Fibular Grafting for the Treatment of Postcollapse Osteonecrosis of the Femoral Head. Surgical Technique J. Mack Aldridge, III, Keith R. Berend, Eunice E. Gunneson and James R. Urbaniak J Bone Joint Surg Am. 2004;86:87-101. This information is current as of August 9, 2009 Reprints and Permissions Click here to order reprints or request permission to use material from this article, or locate the article citation on jbjs.org and click on the [Reprints and Permissions] link. Publisher Information The Journal of Bone and Joint Surgery 20 Pickering Street, Needham, MA 02492-3157 www.jbjs.org COPYRIGHT © 2004 BY THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED Free Vascularized Fibular Grafting for the Treatment of Postcollapse Osteonecrosis of the Femoral Head Surgical Technique By J. Mack Aldridge III, MD, Keith R. Berend, MD, Eunice E. Gunneson, PA-C, and James R. Urbaniak, MD Investigation performed at Duke University Medical Center, Durham, North Carolina The original scientific article in which the surgical technique was presented was published in JBJS Vol. 85-A, pp. 987-993, June 2003 SURGICAL TECHNIQUE ABSTRACT Overview In its early stages, free vascularized fibular grafting of the femoral BACKGROUND: head required two teams of surgeons and an operative time of six Osteonecrosis of the femoral hours or more. Today, thanks in large part to the development of tech- head, a disease primarily affect- nical shortcuts, customized instrumentation, and an operative sup- ing young adults, is often associ- port staff familiar with the nuances of the surgery, free vascularized ated with collapse of the articular fibular grafting of the femoral head can easily be performed in be- surface and subsequent arthro- tween two and one-half and three hours, with two surgeons and one sis.