Unilateral Proximal Focal Femoral Deficiency, Fibular Aplasia, Tibial
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Patellofemoral Syndrome: Evaluation & Management Scott Sevinsky MSPT
Patellofemoral Syndrome: Evaluation & Management Scott Sevinsky MSPT What is Patellofemoral Syndrome? Patellofemoral syndrome (PFS) is a term commonly used to describe a condition where the patella ‘tracks’ or glides improperly between the femoral condyles. This improper tracking causes pain in the anterior knee and may lead to degenerative changes or dislocation of the knee cap. To be more precise the term ‘anterior knee pain’ is suggested to encompass all pain-related problems of the anterior part of the knee. By excluding anterior knee pain due to intra-articular pathology, peripatellar tendinitis or bursitis, plica syndromes, Sinding Larsen’s disease, Osgood Schlatter’s disease, neuromas and other rarely occurring pathologies it is suggested that remaining patients with a clinical presentation of anterior knee pain could be diagnosed with PFPS. The term ‘patellofemoral’ is used as no distinction can be made as to which specific structure of the patella or femur is affected. The term ‘chondromalacia patellae’, defined at the beginning of the 20th century to describe pathological changes of the retropatellar cartilage,7,8 was for half a century, used as a synonym for the syndrome of patellofemoral pain. However, several studies during the last 2 decades have shown a poor correlation between articular cartilage damage and the still not well-defined pain mechanism of retropatellar pain. Review of Knee Anatomy 1. Femur – thigh bone; longest bone in the body. · Lateral femoral condyle larger than medial condyle & projects farther anteriorly. · Medial femoral condyle longer anterior to posterior · Distal surfaces are convex · Intercondylar (trochlear) notch: groove in which the patella glides or ‘tracks’ 2. -

Birth Defects Surveillance Training Facilitator's Guide
BIRTH DEFECTS SURVEILLANCE TRAINING FACILITATOR’S GUIDE Birth defects surveillance training: facilitator’s guide i WHO I CDC I ICBDSR WHO I CDC I ICBDSR ii Birth defects surveillance training: facilitator’s guide BIRTH DEFECTS SURVEILLANCE TRAINING FACILITATOR’S GUIDE Birth defects surveillance training: facilitator’s guide i WHO I CDC I ICBDSR WHO Library Cataloguing-in-Publication Data Birth defects surveillance training: facilitator’s guide 1.Congenital Abnormalities – prevention and control. 2.Neural Tube Defects. 3.Public Health Surveillance. 4.Teaching Materials. I.World Health Organization. II.Centers for Disease Control and Prevention (U.S.). III.International Clearinghouse for Birth Defects Surveillance and Research. ISBN 978 92 4 154928 8 (NLM classification: QS 675) © World Health Organization 2015 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for non-commercial distribution – should be addressed to WHO Press through the WHO website (www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Genetics of Congenital Hand Anomalies
G. C. Schwabe1 S. Mundlos2 Genetics of Congenital Hand Anomalies Die Genetik angeborener Handfehlbildungen Original Article Abstract Zusammenfassung Congenital limb malformations exhibit a wide spectrum of phe- Angeborene Handfehlbildungen sind durch ein breites Spektrum notypic manifestations and may occur as an isolated malforma- an phänotypischen Manifestationen gekennzeichnet. Sie treten tion and as part of a syndrome. They are individually rare, but als isolierte Malformation oder als Teil verschiedener Syndrome due to their overall frequency and severity they are of clinical auf. Die einzelnen Formen kongenitaler Handfehlbildungen sind relevance. In recent years, increasing knowledge of the molecu- selten, besitzen aber aufgrund ihrer Häufigkeit insgesamt und lar basis of embryonic development has significantly enhanced der hohen Belastung für Betroffene erhebliche klinische Rele- our understanding of congenital limb malformations. In addi- vanz. Die fortschreitende Erkenntnis über die molekularen Me- tion, genetic studies have revealed the molecular basis of an in- chanismen der Embryonalentwicklung haben in den letzten Jah- creasing number of conditions with primary or secondary limb ren wesentlich dazu beigetragen, die genetischen Ursachen kon- involvement. The molecular findings have led to a regrouping of genitaler Malformationen besser zu verstehen. Der hohe Grad an malformations in genetic terms. However, the establishment of phänotypischer Variabilität kongenitaler Handfehlbildungen er- precise genotype-phenotype correlations for limb malforma- schwert jedoch eine Etablierung präziser Genotyp-Phänotyp- tions is difficult due to the high degree of phenotypic variability. Korrelationen. In diesem Übersichtsartikel präsentieren wir das We present an overview of congenital limb malformations based Spektrum kongenitaler Malformationen, basierend auf einer ent- 85 on an anatomic and genetic concept reflecting recent molecular wicklungsbiologischen, anatomischen und genetischen Klassifi- and developmental insights. -

Luxating Patella
LUXATING PATELLA What is a luxating patella? The patella, or kneecap, is normally located in the center of the knee joint. The term luxating means, “out of place” or “dislocated”. Therefore, a luxating patella is a kneecap that moves out of its normal location. What causes this? The muscles of the thigh attach to the top of the kneecap. There is a ligament, the patellar ligament, running from the bottom of the kneecap to a point on the tibia just below the knee joint. When the thigh muscles contract, force is transmitted through the patella and patellar ligament to a point on the top of the tibia. This results in extension or straightening of the knee. The patella stays in the center of the leg because the point of attachment of the patellar ligament is on the midline and because the patella slides in a groove on the lower end of the femur (the bone between the knee and the hip). The patella luxates because the point of attachment of the patellar ligament is not on the midline of the tibia. It is almost always located too far medial (toward the middle of the body). As the thigh muscles contract, the force is pulled medial. After several months or years of this abnormal movement, the inner side of the groove in the femur wears down. Once the side of the groove wears down, the patella is then free to dislocate. When this occurs, the dog has difficulty bearing weight on the leg. It may learn how to kick the leg and snap the patella back into its normal location. -
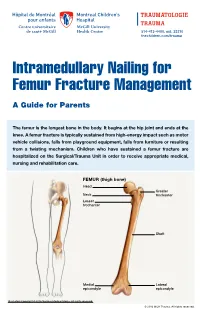
Intramedullary Nailing for Femur Fracture Management a Guide for Parents
514-412-4400, ext. 23310 thechildren.com/trauma Intramedullary Nailing for Femur Fracture Management A Guide for Parents The femur is the longest bone in the body. It begins at the hip joint and ends at the knee. A femur fracture is typically sustained from high-energy impact such as motor vehicle collisions, falls from playground equipment, falls from furniture or resulting from a twisting mechanism. Children who have sustained a femur fracture are hospitalized on the Surgical/Trauma Unit in order to receive appropriate medical, nursing and rehabilitation care. FEMUR (thigh bone) Head Greater Neck trochanter Lesser trochanter Shaft Medial Lateral epicondyle epicondyle Illustration Copyright © 2016 Nucleus Medical Media, All rights reserved. © 2016 MCH Trauma. All rights reserved. FEMUR FRACTURE MANAGEMENT The pediatric Orthopedic Surgeon will assess your child in order to determine the optimal treatment method. Treatment goals include: achieving proper bone realignment, rapid healing, and the return to normal daily activities. The treatment method chosen is primarily based on the child’s age but also taken into consideration are: fracture type, location and other injuries sustained if applicable. Prior to the surgery, your child may be placed in skin traction. This will ensure the bone is in an optimal healing position until it is surgically repaired. Occasionally, traction may be used for a longer period of time. The surgeon will determine if this management is needed based on the specific fracture type and/or location. ELASTIC/FLEXIBLE INTRAMEDULLARY NAILING This surgery is performed by the Orthopedic Surgeon in the Operating Room under general anesthesia. The surgeon will usually make two small incisions near the knee joint in order to insert two flexible titanium rods (intramedullary nails) Flexible through the femur. -
Multiple Hereditary Exostoses
Multiple Hereditary Exostoses Dror Paley MD, FRCSC Medical Director, Paley Orthopedic and spine Institute, St. Mary’s Medical Center, West palm Beach, FL David Feldman, MD Director, Spinal deformity center, Paley Orthopedic and spine Institute, St. Mary’s Medical Center, West palm Beach, FL Multiple hereditary exostoses (MHE), also known as multiple osteochondromas (MO), is an autosomal dominant skeletal disorder. Approximately 10–20% of individuals are a result of a spontaneous mutation while the rest are familial. The prevalence of MHE/MO is 1/50 000. There are two known genes found to cause MHE/MO, EXT1 located on chromosome 8q23-q24 and EXT2 located on chromosome 11p11-p12. In 10–15% of the patients, no mutation can be located by current methods of genetic testing.1–7 These mutations are scattered across both genes. EXT1/EXT2 is essential for the biosynthesis of heparan sulfate (HS). HS production in patients’ cells is reduced by 50% or more.8–19 MHE/MO is associated with characteristic progressive skeletal deformities of the extremities and shortening of one or both the sides, leading to limb length discrepancy (LLD) and short stature.20–28 Two bone segments, such as the lower leg or forearm, are at greater risk of problems due to either osteochondromas (OCs) from one or both bones impinging on or deforming the other bone or a primary issue of altered growth causing one bone to grow at a faster or slower rate. OCs can also affect joint motion due to impingement of an OC with the opposite side of the joint or subluxation/dislocation related to deformity, impingement, and incongruity.20,24,26,29,30 OCs can also cause nerve or vessel entrapment and/or compression, including the spinal cord and nerve roots. -

Case Report Upper Limb Meromelia with Oligodactyly and Brachymesophalangy of the Foot: an Unusual Association
Hindawi Case Reports in Radiology Volume 2019, Article ID 3419383, 5 pages https://doi.org/10.1155/2019/3419383 Case Report Upper Limb Meromelia with Oligodactyly and Brachymesophalangy of the Foot: An Unusual Association Meltem Özdemir , Rasime Pelin Kavak , and Önder Eraslan University of Health Sciences, Dıs¸kapı Yıldırım Beyazıt Training and Research Hospital, Department of Radiology, Ankara, Turkey Correspondence should be addressed to Meltem Ozdemir;¨ [email protected] Received 1 May 2019; Accepted 7 June 2019; Published 24 June 2019 Academic Editor: Ravi Bhargava Copyright © 2019 Meltem Ozdemir¨ et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Meromelia is a rare skeletal abnormality characterized by the partial absence of at least one limb. Several mechanisms have been postulated to explain the etiopathogenesis of the disorder. Most of the cases of meromelia are reported to be sporadic. It can occur either in isolation or with other congenital malformations. VACTERL association, gastroschisis, atrial septal defect, proximal femoral focal defciency, and fbular hemimelia are the congenital abnormalities reported to be in association with meromelia. However, no other congenital abnormalities in association with meromelia have been recorded to date. We herein present an unusual case of bilateral upper limb meromelia accompanied by unilateral oligodactyly and brachymesophalangy of the foot. 1. Introduction herein present an unusual case of meromelia accompanied by congenital deformity of the foot. Amelia refers to the complete absence of at least one limb, and meromelia is characterized by the partial absence of at least one limb. -

Management of Fibular Hemimelia (Congenital Absence of Fibula) Using Ilizarov Method in Sulaimani
European Scientific Journal October 2015 edition vol.11, No.30 ISSN: 1857 – 7881 (Print) e - ISSN 1857- 7431 MANAGEMENT OF FIBULAR HEMIMELIA (CONGENITAL ABSENCE OF FIBULA) USING ILIZAROV METHOD IN SULAIMANI Ass. Prof. Dr. Omer Ali Rafiq Barawi, Ass. Lecturer Zmnako J. Amen School of Medicine, University of Sulaimani, Kurdistan Region, Iraq Abstract Background: Fibular hemimelia is the most common congenital deficiency of long bones. Therefore, it is characterized by a wide spectrum of manifestations ranging from mild limb length inequality to sever shortening with foot and ankle deformities and associated anomalies. Objectives: To evaluate the results of ankle and foot reconstruction and limb length equalization in patients with Fibular Hemimelia. Patients and Methods: A prospective study was carried out on 40 limbs in 32 patients with fibular hemimelia during the periods of March 2010 to January 2014. Male to female ratio was 24:8. Their age ranged at an average between 2-16 years (9 years). The reconstruction of ankle and foot was done. Also, the equalization of the limb was done also using Ilizarov frame. Results: The result of this study was assessed using the Association for the Study of Applications of Methods of Ilizarov (ASAMI) scoring system. Therefore, the final results were: Failure rate with 2 limbs 5%, Poor with 2 limbs 5%, Fair with 2 limbs 5%, Good with 8 limbs 20%, and Excellent with 26 limbs 65%. Conclusion: In conclusion, the Ilizarov method is an attractive alternative method used for the management of selected fibular hemimelic patients having three or more toes who are refusing amputation. -

Bones Can Tell Us More Compiled By: Nancy Volk
Bones Can Tell Us More Compiled By: Nancy Volk Strong Bones Sometimes only a few bones are found in a location in an archeological dig. VOCABULARY A few bones can tell about the height of a person. This is possible due to the Femur ratios of the bones. It has been determined that there are relationships between the femur, tibia, humerus, and radius and a person’s height. Humerus Radius Here is a little help to identify these four bones and formulas to assist with Tibia determining the height of a person based on bone length. Humerus Femur: Humerus: The thigh is the region of the femur. The arm bone most people call the From the hip bone to the knee bone. upper arm. It is found from the elbow to the shoulder joints. Inside This Packet Radius Strong Bones 1 New York State Standards 1 Activity: Bone Relationships 2 Information for the Teacher 4 Tibia: Radius: The larger and stronger of the two bones The bone found in the forearm that New York State Standards in the leg below the knee bone. extends from the side of the elbow to Middle School In vertebrates It is recognized as the the wrist. Standard 4: Living Environment strongest weight bearing bone in the Idea 1: 1.2a, 1.2b, 1.2e, 1.2f body. Life Sciences - Post Module 3 Middle School Page 1 Activity: Bone Relationships MATERIALS NEEDED Skeleton Formulas: Tape Measure Bone relationship is represented by the following formulas: Directions and formulas P represents the person’s height. The last letter of each formula stands for the Calculator known length of the bone (femur, tibia, humerus, or radius) through measurement. -

Normative Values for Femoral Length, Tibial Length, Andthe Femorotibial
Article Normative Values for Femoral Length, Tibial Length, and the Femorotibial Ratio in Adults Using Standing Full-Length Radiography Stuart A Aitken MaineGeneral Medical Center, 35 Medical Center Parkway, Augusta, ME 04330, USA; [email protected] Abstract: Knowledge of the normal length and skeletal proportions of the lower limb is required as part of the evaluation of limb length discrepancy. When measuring limb length, modern standing full-length digital radiographs confer a level of clinical accuracy interchangeable with that of CT imaging. This study reports a set of normative values for lower limb length using the standing full-length radiographs of 753 patients (61% male). Lower limb length, femoral length, tibial length, and the femorotibial ratio were measured in 1077 limbs. The reliability of the measurement method was tested using the intra-class correlation (ICC) of agreement between three observers. The mean length of 1077 lower limbs was 89.0 cm (range 70.2 to 103.9 cm). Mean femoral length was 50.0 cm (39.3 to 58.4 cm) and tibial length was 39.0 cm (30.8 to 46.5 cm). The median side-to-side difference was 0.4 cm (0.2 to 0.7, max 1.8 cm) between 324 paired limbs. The mean ratio of femoral length to tibial length for the study population was 1.28:1 (range 1.16 to 1.39). A moderately strong inverse linear relationship (r = −0.35, p < 0.001, Pearson’s) was identified between tibial length and the Citation: Aitken, S.A. Normative corresponding femorotibial ratio. -

A CLINICAL STUDY of 25 CASES of CONGENITAL KEY WORDS: Ectromelia, Hemimelia, Dysmelia, Axial, Inter- LIMB DEFICIENCIES Calary
PARIPEX - INDIAN JOURNAL OF RESEARCH Volume-7 | Issue-1 | January-2018 | PRINT ISSN No 2250-1991 ORIGINAL RESEARCH PAPER Medical Science A CLINICAL STUDY OF 25 CASES OF CONGENITAL KEY WORDS: Ectromelia, Hemimelia, Dysmelia, Axial, Inter- LIMB DEFICIENCIES calary M.B.B.S., D.N.B (PMR), M.N.A.M.S Medical officer, D.P.M.R., K.G Medical Dr Abhiman Singh University Lucknow (UP) An Investigation of 25 patients from congenital limb deficient patients who went to D. P. M. R. , K.G Medical University Lucknow starting with 2010 with 2017. This study represents the congenital limb deficient insufficient number of the India. Commonest deficiencies were Adactylia Also mid Ectromelia (below knee/ below elbow deficiency).Below knee might have been basic in male same time The following elbow for female Youngsters. No conclusive reason for the deformity might be isolated, however, A large number guardians accepted that possible exposure to the eclipse throughout pregnancy might have been those reason for ABSTRACT those deficiency. INTRODUCTION Previous Treatment Only 15 patients had taken some D. P. M. R., K.G Medical University Lucknow (UP) may be a greatest treatment, 5 underwent some surgical treatment and only 4 Also its identity or sort of Rehabilitation Centre in India. Thusly the patients used prosthesis. This indicates the ignorance or lack of limb deficient children attending this department can easily be facilities to deal with the limb deficient children. accepted as a representative sample of the total congenital limb deficiency population in the India. DEFICIENCIES The deficiencies are classified into three categories:- MATERIAL AND METHODS This study incorporates 25 patients congenital limb deficiency for 1) Axial Dysmelia where medial or lateral portion is missing lack who originated for medicine at D.