Birth Defects Surveillance Training Facilitator's Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetics of Congenital Hand Anomalies
G. C. Schwabe1 S. Mundlos2 Genetics of Congenital Hand Anomalies Die Genetik angeborener Handfehlbildungen Original Article Abstract Zusammenfassung Congenital limb malformations exhibit a wide spectrum of phe- Angeborene Handfehlbildungen sind durch ein breites Spektrum notypic manifestations and may occur as an isolated malforma- an phänotypischen Manifestationen gekennzeichnet. Sie treten tion and as part of a syndrome. They are individually rare, but als isolierte Malformation oder als Teil verschiedener Syndrome due to their overall frequency and severity they are of clinical auf. Die einzelnen Formen kongenitaler Handfehlbildungen sind relevance. In recent years, increasing knowledge of the molecu- selten, besitzen aber aufgrund ihrer Häufigkeit insgesamt und lar basis of embryonic development has significantly enhanced der hohen Belastung für Betroffene erhebliche klinische Rele- our understanding of congenital limb malformations. In addi- vanz. Die fortschreitende Erkenntnis über die molekularen Me- tion, genetic studies have revealed the molecular basis of an in- chanismen der Embryonalentwicklung haben in den letzten Jah- creasing number of conditions with primary or secondary limb ren wesentlich dazu beigetragen, die genetischen Ursachen kon- involvement. The molecular findings have led to a regrouping of genitaler Malformationen besser zu verstehen. Der hohe Grad an malformations in genetic terms. However, the establishment of phänotypischer Variabilität kongenitaler Handfehlbildungen er- precise genotype-phenotype correlations for limb malforma- schwert jedoch eine Etablierung präziser Genotyp-Phänotyp- tions is difficult due to the high degree of phenotypic variability. Korrelationen. In diesem Übersichtsartikel präsentieren wir das We present an overview of congenital limb malformations based Spektrum kongenitaler Malformationen, basierend auf einer ent- 85 on an anatomic and genetic concept reflecting recent molecular wicklungsbiologischen, anatomischen und genetischen Klassifi- and developmental insights. -

Unilateral Proximal Focal Femoral Deficiency, Fibular Aplasia, Tibial
The Egyptian Journal of Medical Human Genetics (2014) 15, 299–303 Ain Shams University The Egyptian Journal of Medical Human Genetics www.ejmhg.eg.net www.sciencedirect.com CASE REPORT Unilateral proximal focal femoral deficiency, fibular aplasia, tibial campomelia and oligosyndactyly in an Egyptian child – Probable FFU syndrome Rabah M. Shawky a,*, Heba Salah Abd Elkhalek a, Shaimaa Gad a, Shaimaa Abdelsattar Mohammad b a Pediatric Department, Genetics Unit, Ain Shams University, Egypt b Radio Diagnosis Department, Ain Shams University, Egypt Received 2 March 2014; accepted 18 March 2014 Available online 30 April 2014 KEYWORDS Abstract We report a fifteen month old Egyptian male child, the third in order of birth of healthy Short femur; non consanguineous parents, who has normal mentality, normal upper limbs and left lower limb. Limb anomaly; The right lower limb has short femur, and tibia with anterior bowing, and an overlying skin dimple. FFU syndrome; The right foot has also oligosyndactyly (three toes), and the foot is in vulgus position. There is lim- Proximal focal femoral ited abduction at the hip joint, full flexion and extension at the knee, limited dorsiflexion and plan- deficiency; tar flexion at the ankle joint. The X-ray of the lower limb and pelvis shows proximal focal femoral Fibular aplasia; deficiency, absent right fibula with shortening of the right tibia and anterior bowing of its distal Tibial campomelia; third. The acetabulum is shallow. He has a family history of congenital cyanotic heart disease. Oligosyndactyly Our patient represents most probably the first case of femur fibula ulna syndrome (FFU) in Egypt with unilateral right leg affection. -

Case Report Upper Limb Meromelia with Oligodactyly and Brachymesophalangy of the Foot: an Unusual Association
Hindawi Case Reports in Radiology Volume 2019, Article ID 3419383, 5 pages https://doi.org/10.1155/2019/3419383 Case Report Upper Limb Meromelia with Oligodactyly and Brachymesophalangy of the Foot: An Unusual Association Meltem Özdemir , Rasime Pelin Kavak , and Önder Eraslan University of Health Sciences, Dıs¸kapı Yıldırım Beyazıt Training and Research Hospital, Department of Radiology, Ankara, Turkey Correspondence should be addressed to Meltem Ozdemir;¨ [email protected] Received 1 May 2019; Accepted 7 June 2019; Published 24 June 2019 Academic Editor: Ravi Bhargava Copyright © 2019 Meltem Ozdemir¨ et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Meromelia is a rare skeletal abnormality characterized by the partial absence of at least one limb. Several mechanisms have been postulated to explain the etiopathogenesis of the disorder. Most of the cases of meromelia are reported to be sporadic. It can occur either in isolation or with other congenital malformations. VACTERL association, gastroschisis, atrial septal defect, proximal femoral focal defciency, and fbular hemimelia are the congenital abnormalities reported to be in association with meromelia. However, no other congenital abnormalities in association with meromelia have been recorded to date. We herein present an unusual case of bilateral upper limb meromelia accompanied by unilateral oligodactyly and brachymesophalangy of the foot. 1. Introduction herein present an unusual case of meromelia accompanied by congenital deformity of the foot. Amelia refers to the complete absence of at least one limb, and meromelia is characterized by the partial absence of at least one limb. -

Ultrasound Anomaly Details
Appendix 2. Association of Copy Number Variants With Specific Ultrasonographically Detected Fetal Anomalies Ultrasound Anomaly Details Abdominal wall Bladder exstrophy Body-stalk anomaly Cloacal exstrophy Gastroschisis Omphalocele Other: free text box CNS Absent cerebellar vermis Agenesis of corpus collosum Anencephaly Arachnoid cyst Cerebellar hypoplasia Chiari malformation Dandy-Walker malformation Encephalocele Anterior Posterior Holoprosencephaly Hydranencephaly Iniencephaly Lissencephaly Parenchymal defect Posterior fossa cyst Spina bifida Vascular anomaly Ventriculomegaly/Hydrocephaly Unilateral Mild (10-12mm) Moderate (13-15mm) Severe (>15mm) Bilateral Mild (10-12mm) Moderate (13-15mm) Severe (>15mm) Other: free text box Ear Outer ear malformation Unilateral Bilateral Other: free text box Effusion Hydrops Single effusion only Ascites Pericardial effusion Pleural effusion Skin edema Donnelly JC, Platt LD, Rebarber A, Zachary J, Grobman WA, and Wapner RJ. Association of copy number variants with specific ultrasonographically detected fetal anomalies. Obstet Gynecol 2014;124. The authors provided this information as a supplement to their article. © Copyright 2014 American College of Obstetricians and Gynecologists. Page 1 of 6 Other: free text box Fac Eye anomalies Cyclopia Hypertelorism Hypotelorism Microphthalmia Other: free text box Facial tumor Lip - Cleft Unilateral Midline Bilateral Nose Absent / hypoplastic nose bone Depressed nasal bridge Palate – Cleft Profile -

Four Unusual Cases of Congenital Forelimb Malformations in Dogs
animals Article Four Unusual Cases of Congenital Forelimb Malformations in Dogs Simona Di Pietro 1 , Giuseppe Santi Rapisarda 2, Luca Cicero 3,* , Vito Angileri 4, Simona Morabito 5, Giovanni Cassata 3 and Francesco Macrì 1 1 Department of Veterinary Sciences, University of Messina, Viale Palatucci, 98168 Messina, Italy; [email protected] (S.D.P.); [email protected] (F.M.) 2 Department of Veterinary Prevention, Provincial Health Authority of Catania, 95030 Gravina di Catania, Italy; [email protected] 3 Institute Zooprofilattico Sperimentale of Sicily, Via G. Marinuzzi, 3, 90129 Palermo, Italy; [email protected] 4 Veterinary Practitioner, 91025 Marsala, Italy; [email protected] 5 Ospedale Veterinario I Portoni Rossi, Via Roma, 57/a, 40069 Zola Predosa (BO), Italy; [email protected] * Correspondence: [email protected] Simple Summary: Congenital limb defects are sporadically encountered in dogs during normal clinical practice. Literature concerning their diagnosis and management in canine species is poor. Sometimes, the diagnosis and description of congenital limb abnormalities are complicated by the concurrent presence of different malformations in the same limb and the lack of widely accepted classification schemes. In order to improve the knowledge about congenital limb anomalies in dogs, this report describes the clinical and radiographic findings in four dogs affected by unusual congenital forelimb defects, underlying also the importance of reviewing current terminology. Citation: Di Pietro, S.; Rapisarda, G.S.; Cicero, L.; Angileri, V.; Morabito, Abstract: Four dogs were presented with thoracic limb deformity. After clinical and radiographic S.; Cassata, G.; Macrì, F. Four Unusual examinations, a diagnosis of congenital malformations was performed for each of them. -

Malformation Syndromes: a Review of Mouse/Human Homology
J Med Genet: first published as 10.1136/jmg.25.7.480 on 1 July 1988. Downloaded from Joalrn(ll of Medical Genetics 1988, 25, 480-487 Malformation syndromes: a review of mouse/human homology ROBIN M WINTER Fromii the Kennetivdy Galton Centre, Clinlicail Research Centre, Northiwick Park Hospital, Harrow, Middlesex HAI 3UJ. SUMMARY The purpose of this paper is to review the known and possible homologies between mouse and human multiple congenital anomaly syndromes. By identifying single gene defects causing similar developmental abnormalities in mouse and man, comparative gene mapping can be carried out, and if the loci in mouse and man are situated in homologous chromosome segments, further molecular studies can be performed to show that the loci are identical. This paper puts forward tentative homologies in the hope that some will be investigated and shown to be true homologies at the molecular level, thus providing mouse models for complex developmental syndromes. The mouse malformation syndromes are reviewed according to their major gene effects. X linked syndromes are reviewed separately because of the greater ease of establishing homology for these conditions. copyright. The purpose of this paper is to review the known even phenotypic similarity would be no guarantee and possible homologies between mouse and human that such genes in man and mouse are homologous". genetic malformation syndromes. Lalley and By identifying single gene defects causing similar following criteria for developmental abnormalities in mouse and man, McKusick' recommend the http://jmg.bmj.com/ identifying gene homologies between species: comparative gene mapping can be carried out, and if (1) Similar nucleotide or amino acid sequence. -

Appendix 3.1 Birth Defects Descriptions for NBDPN Core, Recommended, and Extended Conditions Updated March 2017
Appendix 3.1 Birth Defects Descriptions for NBDPN Core, Recommended, and Extended Conditions Updated March 2017 Participating members of the Birth Defects Definitions Group: Lorenzo Botto (UT) John Carey (UT) Cynthia Cassell (CDC) Tiffany Colarusso (CDC) Janet Cragan (CDC) Marcia Feldkamp (UT) Jamie Frias (CDC) Angela Lin (MA) Cara Mai (CDC) Richard Olney (CDC) Carol Stanton (CO) Csaba Siffel (GA) Table of Contents LIST OF BIRTH DEFECTS ................................................................................................................................................. I DETAILED DESCRIPTIONS OF BIRTH DEFECTS ...................................................................................................... 1 FORMAT FOR BIRTH DEFECT DESCRIPTIONS ................................................................................................................................. 1 CENTRAL NERVOUS SYSTEM ....................................................................................................................................... 2 ANENCEPHALY ........................................................................................................................................................................ 2 ENCEPHALOCELE ..................................................................................................................................................................... 3 HOLOPROSENCEPHALY............................................................................................................................................................. -

The Baller-Gerold Syndrome
26626 Med Genet 1992; 29: 266-268 The Baller-Gerold syndrome L Van Maldergem, A Verloes, L Lejeune, Y Gillerot Abstract grandmothers, bearing the same name, origin- A case of severe craniosynostosis-radial ated from the same small village and called aplasia (Baller-Gerold) syndrome is de- each other 'cousin'. The pregnancy was scribed in a newborn male, following a uneventful until 7 months of gestation when pregnancy complicated by polyhydram- intrauterine growth retardation (IUGR) was nios and intrauterine growth retard- first detected on echography. Fetal weight cal- ation. Death occurred after two hours culated from abdominal measurement and owing to a prolonged apnoeic spell. Ex- femur length decreased from the 50th to the tensive agenesis of the frontal and 3rd centile. At 8 months, major malformations parietal bones, resulting in a very large of the cranial vault could be seen. The limbs fontanelle, in addition to coronal bilat- could not be visualised clearly because of the eral craniosynostosis was observed at lack of amniotic fluid owing to advanced gesta- necropsy. There was also bilateral radial tional age. Diabetes mellitus screening tests agenesis, oligodactyly of the hands and were negative. Birth occurred at 37 weeks with feet, a midline facial angioma, and a breech presentation. The baby weighed Humaine, Institut de scrotally positioned anus, all of which 2250 g, length 43 cm, and head circumference Morphologie have been described in some of the 10 35 cm. Apgar score were 10 and 7 at one and Pathologique, Allee previously reported cases. Microcephaly, five minutes. A severe malformation complex des Templiers 41, erythroblastosis of the liver, and pan- B-6280 Gerpinnes was obvious and included the following: turri- (Loverval), Belgium. -

Miller Syndrome (Postaxial Acrofacial Dysostosis): and Expansion of The
J Med Genet: first published as 10.1136/jmg.28.10.695 on 1 October 1991. Downloaded from J Med Genet 1991; 28: 695-700 695 Miller syndrome (postaxial acrofacial dysostosis): further evidence for autosomal recessive inheritance and expansion of the phenotype A L Ogilvy-Stuart, A C Parsons Abstract Case reports A sibship with postaxial acrofacial dysostosis CASE 1 syndrome (Miller syndrome) is reported. In This girl is the second daughter born to unrelated addition to the characteristic facial and limb Caucasian parents. The first child is apparently defects, previously undescribed anomalies, entirely normal. At the time of delivery the mother including midgut malrotation, gastric volvu- was 26 years old, and the father 29 years. The lus, and renal anomalies, are recorded. pregancy was uncomplicated and no drugs were taken. She was born at term by lower section caesar- ian section for failure to progress. The Apgar score Miller syndrome is a rare, well defined malformation at one and five minutes was 8. No resuscitation was syndrome. The craniofacial abnormalities are simi- required. At birth her weight was 3160 g (25th lar to those of the Treacher Collins syndrome. The centile), length 46cm (less than the 10th centile), limb defects predominantly involve the postaxial and the head circumference 34 cm (25th centile). ray, with a wide range of severity, and to a lesser The following facial abnormalities were noted: extent the preaxial ray. micrognathia, malar hypoplasia, small shallow orbits copyright. The syndrome was first described as a complete with bilateral proptosis, downward slanting palpe- clinical entity by Miller et all in 1979. -
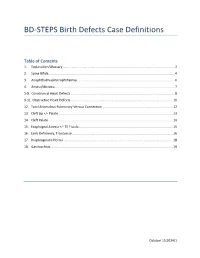
BD-STEPS Birth Defects Case Definitions
BD-STEPS Birth Defects Case Definitions Table of Contents 1. Explanation/Glossary ............................................................................................................................ 2 2. Spina Bifida............................................................................................................................................ 4 3. Anophthalmia/microphthalmia ............................................................................................................ 6 4. Anotia/Microtia ..................................................................................................................................... 7 5-8. Conotruncal Heart Defects ................................................................................................................... 8 9-11. Obstructive Heart Defects ................................................................................................................. 10 12. Total Anomalous Pulmonary Venous Connection .............................................................................. 12 13. Cleft Lip +/- Palate ............................................................................................................................... 13 14. Cleft Palate .......................................................................................................................................... 14 15. Esophageal Atresia +/- TE Fistula ........................................................................................................ 15 16. Limb -

Craniosynostosis and Multiple Skeletal Anomalies in Humans and Zebrafish Result from a Defect in the Localized Degradation of Retinoic Acid
ARTICLE Craniosynostosis and Multiple Skeletal Anomalies in Humans and Zebrafish Result from a Defect in the Localized Degradation of Retinoic Acid Kathrin Laue,1,12 Hans-Martin Pogoda,1 Philip B. Daniel,2 Arie van Haeringen,3 Yasemin Alanay,4,13 Simon von Ameln,5 Martin Rachwalski,5,6 Tim Morgan,2 Mary J. Gray,2 Martijn H. Breuning,3 Gregory M. Sawyer,7 Andrew J. Sutherland-Smith,7 Peter G. Nikkels,8 Christian Kubisch,5,9,10 Wilhelm Bloch,9,11 Bernd Wollnik,5,6,9 Matthias Hammerschmidt,1,6,9,14,* and Stephen P. Robertson2,14,* Excess exogenous retinoic acid (RA) has been well documented to have teratogenic effects in the limb and craniofacial skeleton. Malfor- mations that have been observed in this context include craniosynostosis, a common developmental defect of the skull that occurs in 1 in 2500 individuals and results from premature fusion of the cranial sutures. Despite these observations, a physiological role for RA during suture formation has not been demonstrated. Here, we present evidence that genetically based alterations in RA signaling inter- fere with human development. We have identified human null and hypomorphic mutations in the gene encoding the RA-degrading enzyme CYP26B1 that lead to skeletal and craniofacial anomalies, including fusions of long bones, calvarial bone hypoplasia, and cra- niosynostosis. Analyses of murine embryos exposed to a chemical inhibitor of Cyp26 enzymes and zebrafish lines with mutations in cyp26b1 suggest that the endochondral bone fusions are due to unrestricted chondrogenesis at the presumptive sites of joint formation within cartilaginous templates, whereas craniosynostosis is induced by a defect in osteoblastic differentiation. -

EUROCAT Syndrome Guide
JRC - Central Registry european surveillance of congenital anomalies EUROCAT Syndrome Guide Definition and Coding of Syndromes Version July 2017 Revised in 2016 by Ingeborg Barisic, approved by the Coding & Classification Committee in 2017: Ester Garne, Diana Wellesley, David Tucker, Jorieke Bergman and Ingeborg Barisic Revised 2008 by Ingeborg Barisic, Helen Dolk and Ester Garne and discussed and approved by the Coding & Classification Committee 2008: Elisa Calzolari, Diana Wellesley, David Tucker, Ingeborg Barisic, Ester Garne The list of syndromes contained in the previous EUROCAT “Guide to the Coding of Eponyms and Syndromes” (Josephine Weatherall, 1979) was revised by Ingeborg Barisic, Helen Dolk, Ester Garne, Claude Stoll and Diana Wellesley at a meeting in London in November 2003. Approved by the members EUROCAT Coding & Classification Committee 2004: Ingeborg Barisic, Elisa Calzolari, Ester Garne, Annukka Ritvanen, Claude Stoll, Diana Wellesley 1 TABLE OF CONTENTS Introduction and Definitions 6 Coding Notes and Explanation of Guide 10 List of conditions to be coded in the syndrome field 13 List of conditions which should not be coded as syndromes 14 Syndromes – monogenic or unknown etiology Aarskog syndrome 18 Acrocephalopolysyndactyly (all types) 19 Alagille syndrome 20 Alport syndrome 21 Angelman syndrome 22 Aniridia-Wilms tumor syndrome, WAGR 23 Apert syndrome 24 Bardet-Biedl syndrome 25 Beckwith-Wiedemann syndrome (EMG syndrome) 26 Blepharophimosis-ptosis syndrome 28 Branchiootorenal syndrome (Melnick-Fraser syndrome) 29 CHARGE