Femur Fractures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Patellofemoral Syndrome: Evaluation & Management Scott Sevinsky MSPT
Patellofemoral Syndrome: Evaluation & Management Scott Sevinsky MSPT What is Patellofemoral Syndrome? Patellofemoral syndrome (PFS) is a term commonly used to describe a condition where the patella ‘tracks’ or glides improperly between the femoral condyles. This improper tracking causes pain in the anterior knee and may lead to degenerative changes or dislocation of the knee cap. To be more precise the term ‘anterior knee pain’ is suggested to encompass all pain-related problems of the anterior part of the knee. By excluding anterior knee pain due to intra-articular pathology, peripatellar tendinitis or bursitis, plica syndromes, Sinding Larsen’s disease, Osgood Schlatter’s disease, neuromas and other rarely occurring pathologies it is suggested that remaining patients with a clinical presentation of anterior knee pain could be diagnosed with PFPS. The term ‘patellofemoral’ is used as no distinction can be made as to which specific structure of the patella or femur is affected. The term ‘chondromalacia patellae’, defined at the beginning of the 20th century to describe pathological changes of the retropatellar cartilage,7,8 was for half a century, used as a synonym for the syndrome of patellofemoral pain. However, several studies during the last 2 decades have shown a poor correlation between articular cartilage damage and the still not well-defined pain mechanism of retropatellar pain. Review of Knee Anatomy 1. Femur – thigh bone; longest bone in the body. · Lateral femoral condyle larger than medial condyle & projects farther anteriorly. · Medial femoral condyle longer anterior to posterior · Distal surfaces are convex · Intercondylar (trochlear) notch: groove in which the patella glides or ‘tracks’ 2. -

Delayed Massive Hemothorax Requiring
Clin Exp Emerg Med 2018;5(1):60-65 https://doi.org/10.15441/ceem.16.190 Case Report Delayed massive hemothorax requiring eISSN: 2383-4625 surgery after blunt thoracic trauma over a 5-year period: complicating rib fracture with sharp edge associated with diaphragm injury Received: 26 September 2017 Revised: 28 January 2018 Sung Wook Chang, Kyoung Min Ryu, Jae-Wook Ryu Accepted: 20 February 2018 Trauma Center, Department of Thoracic and Cardiovascular Surgery, Dankook University Hospital, Cheonan, Korea Correspondence to: Jae-Wook Ryu Department of Thoracic and Cardiovascular Surgery, Dankook Delayed massive hemothorax requiring surgery is relatively uncommon and can potentially be University Hospital, 201 Manghyang-ro, Dongnam-gu, Cheonan 31116, Korea life-threatening. Here, we aimed to describe the nature and cause of delayed massive hemotho- E-mail: [email protected] rax requiring immediate surgery. Over 5 years, 1,278 consecutive patients were admitted after blunt trauma. Delayed hemothorax is defined as presenting with a follow-up chest radiograph and computed tomography showing blunting or effusion. A massive hemothorax is defined as blood drainage >1,500 mL after closed thoracostomy and continuous bleeding at 200 mL/hr for at least four hours. Five patients were identified all requiring emergency surgery. Delayed mas- sive hemothorax presented 63.6±21.3 hours after blunt chest trauma. All patients had superfi- cial diaphragmatic lacerations caused by the sharp edge of a broken rib. The mean preoperative chest tube drainage was 3,126±463 mL. We emphasize the high-risk of massive hemothorax in patients who have a broken rib with sharp edges. -

Accuracy of Diagnosis of Distal Radial Fractures by Ultrasound Ahmad Saladdin Sultan, Muddather Abdul Aziz, Yakdhan Z
The Egyptian Journal of Hospital Medicine (October 2017) Vol. 69 (8), Page 3115-3122 Accuracy of Diagnosis of Distal Radial Fractures by Ultrasound Ahmad Saladdin Sultan, Muddather Abdul Aziz, Yakdhan Z. Alsaleem Mosul Teaching Hospital, Emergency Medicine Department, Mosul, Iraq Corresponding author: Ahmad Saladdin <[email protected] ABSTRACT Background: although distal radial fracture account up to 20% of all fractures, it forms the most common fracture in upper extremities. Distal radial fracture has six types the most common one is Colle's fracture. The gold standard for diagnosis of distal radial fracture is conventional radiograph. Despite using ultrasound in tendon rupture, localizing foreign bodies, ultrasound started to be used for diagnosing bone fracture especially distal radius. Aim of the work: this study aimed to detect the accuracy of ultrasound in the diagnosis of distal radial fracture. Patients and methods: this was a selective prospective case series study in the Emergency Department, Al-Jumhoori Teaching Hospital,78 patients were included in this study, their age ranged between 6-45 years with mean age 17.1. 59 were males and 19 females. Duration of the study was one year (January2013 - January 2014). Results: by analyzing data of 78 patients for distal radial fracture ultrasound and comparing the results with the gold standard conventional radiograph we found that sensitivity of ultrasound in detecting fracture was 95.5%, specificity 100%, accuracy 96.15%, positive predictive value 100% and negative predictive value 80%. Conclusion: results of the current work demonstrated that ultrasound can be considered as a promising alternative to routine radiograph in diagnosis of the distal radial fractures and the horizon still open for further studies of use of ultrasound in diagnosis of other types of fractures. -

Compression Garments for Leg Lymphoedema
Compression garments for leg lymphoedema You have been fitted with a compression garment to help reduce the lymphoedema in your leg. Compression stockings work by limiting the amount of fluid building up in your leg. They provide firm support, enabling the muscles to pump fluid away more effectively. They provide most pressure at the foot and less at the top of the leg so fluid is pushed out of the limb where it will drain away more easily. How do I wear it? • Wear your garment every day to control the swelling in your leg. • Put your garment on as soon as possible after getting up in the morning. This is because as soon as you stand up and start to move around extra fluid goes into your leg and it begins to swell. • Take the garment off before bedtime unless otherwise instructed by your therapist. We appreciate that in hot weather garments can be uncomfortable, but unfortunately this is when it is important to wear it as the heat can increase the swelling. If you would like to leave off your garment for a special occasion please ask the clinic for advice. What should I look out for? Your garment should feel firm but not uncomfortable: • If you notice the garment is rubbing or cutting in, adjust the garment or remove it and reapply it. • If your garment feels tight during the day, try and think about what may have caused this. If you have been busy, sit down and elevate your leg and rest for at least 30 minutes. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Treatment of Common Hip Fractures: Evidence Report/Technology
This report is based on research conducted by the Minnesota Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. HHSA 290 2007 10064 1). The findings and conclusions in this document are those of the authors, who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help clinicians, employers, policymakers, and others make informed decisions about the provision of health care services. This report is intended as a reference and not as a substitute for clinical judgment. This report may be used, in whole or in part, as the basis for the development of clinical practice guidelines and other quality enhancement tools, or as a basis for reimbursement and coverage policies. AHRQ or U.S. Department of Health and Human Services endorsement of such derivative products may not be stated or implied. Evidence Report/Technology Assessment Number 184 Treatment of Common Hip Fractures Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. HHSA 290 2007 10064 1 Prepared by: Minnesota Evidence-based Practice Center, Minneapolis, Minnesota Investigators Mary Butler, Ph.D., M.B.A. Mary Forte, D.C. Robert L. Kane, M.D. Siddharth Joglekar, M.D. Susan J. Duval, Ph.D. Marc Swiontkowski, M.D. -

Sports Ankle Injuries Assessment and Management
FOCUS Sports injuries Sports ankle injuries Drew Slimmon Peter Brukner Assessment and management Background Case study Lucia is a female, 16 years of age, who plays netball with the Sports ankle injuries present commonly in the general state under 17s netball team. She presents with an ankle injury practice setting. The majority of these injuries are inversion sustained at training the previous night. She is on crutches and plantar flexion injuries that result in damage to the and is nonweight bearing. Examination raises the possibility of lateral ligament complex. a fracture, but X-ray is negative. You diagnose a severe lateral Objective ligament sprain and manage Lucia with ice, a compression The aim of this article is to review the assessment and bandage and a backslab initially. She then progresses through management of sports ankle injuries in the general practice a 6 week rehabilitation program and you recommend she wear setting. an ankle brace for at least 6 months. Discussion Assessment of an ankle injury begins with a detailed history to determine the severity, mechanism and velocity of the injury, what happened immediately after and whether there is a past history of inadequately rehabilitated ankle injury. Examination involves assessment of weight bearing, inspection, palpation, movement, and application of special examination tests. Plain X-rays may be helpful to exclude a fracture. If the diagnosis is uncertain, consider second The majority of ankle injuries are inversion and plantar line investigations including bone scan, computerised flexion injuries that result in damage to the lateral tomography or magnetic resonance imaging, and referral to a ligament complex (Figure 1). -

Luxating Patella
LUXATING PATELLA What is a luxating patella? The patella, or kneecap, is normally located in the center of the knee joint. The term luxating means, “out of place” or “dislocated”. Therefore, a luxating patella is a kneecap that moves out of its normal location. What causes this? The muscles of the thigh attach to the top of the kneecap. There is a ligament, the patellar ligament, running from the bottom of the kneecap to a point on the tibia just below the knee joint. When the thigh muscles contract, force is transmitted through the patella and patellar ligament to a point on the top of the tibia. This results in extension or straightening of the knee. The patella stays in the center of the leg because the point of attachment of the patellar ligament is on the midline and because the patella slides in a groove on the lower end of the femur (the bone between the knee and the hip). The patella luxates because the point of attachment of the patellar ligament is not on the midline of the tibia. It is almost always located too far medial (toward the middle of the body). As the thigh muscles contract, the force is pulled medial. After several months or years of this abnormal movement, the inner side of the groove in the femur wears down. Once the side of the groove wears down, the patella is then free to dislocate. When this occurs, the dog has difficulty bearing weight on the leg. It may learn how to kick the leg and snap the patella back into its normal location. -
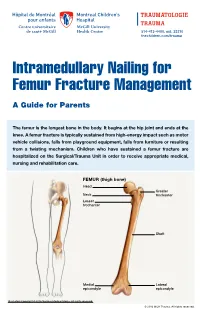
Intramedullary Nailing for Femur Fracture Management a Guide for Parents
514-412-4400, ext. 23310 thechildren.com/trauma Intramedullary Nailing for Femur Fracture Management A Guide for Parents The femur is the longest bone in the body. It begins at the hip joint and ends at the knee. A femur fracture is typically sustained from high-energy impact such as motor vehicle collisions, falls from playground equipment, falls from furniture or resulting from a twisting mechanism. Children who have sustained a femur fracture are hospitalized on the Surgical/Trauma Unit in order to receive appropriate medical, nursing and rehabilitation care. FEMUR (thigh bone) Head Greater Neck trochanter Lesser trochanter Shaft Medial Lateral epicondyle epicondyle Illustration Copyright © 2016 Nucleus Medical Media, All rights reserved. © 2016 MCH Trauma. All rights reserved. FEMUR FRACTURE MANAGEMENT The pediatric Orthopedic Surgeon will assess your child in order to determine the optimal treatment method. Treatment goals include: achieving proper bone realignment, rapid healing, and the return to normal daily activities. The treatment method chosen is primarily based on the child’s age but also taken into consideration are: fracture type, location and other injuries sustained if applicable. Prior to the surgery, your child may be placed in skin traction. This will ensure the bone is in an optimal healing position until it is surgically repaired. Occasionally, traction may be used for a longer period of time. The surgeon will determine if this management is needed based on the specific fracture type and/or location. ELASTIC/FLEXIBLE INTRAMEDULLARY NAILING This surgery is performed by the Orthopedic Surgeon in the Operating Room under general anesthesia. The surgeon will usually make two small incisions near the knee joint in order to insert two flexible titanium rods (intramedullary nails) Flexible through the femur. -

ANTERIOR KNEE PAIN Home Exercises
ANTERIOR KNEE PAIN Home Exercises Anterior knee pain is pain that occurs at the front and center of the knee. It can be caused by many different problems, including: • Weak or overused muscles • Chondromalacia of the patella (softening and breakdown of the cartilage on the underside of the kneecap) • Inflammations and tendon injury (bursitis, tendonitis) • Loose ligaments with instability of the kneecap • Articular cartilage damage (chondromalacia patella) • Swelling due to fluid buildup in the knee joint • An overload of the extensor mechanism of the knee with or without malalignment of the patella You may feel pain after exercising or when you sit too long. The pain may be a nagging ache or an occasional sharp twinge. Because the pain is around the front of your knee, treatment has traditionally focused on the knee itself and may include taping or bracing the kneecap, or patel- la, and/ or strengthening the thigh muscle—the quadriceps—that helps control your kneecap to improve the contact area between the kneecap and the thigh bone, or femur, beneath it. Howev- er, recent evidence suggests that strengthening your hip and core muscles can also help. The control of your knee from side to side comes from the glutes and core control; that is why those areas are so important in management of anterior knee pain. The exercises below will work on a combination of flexibility and strength of your knee, hip, and core. Although some soreness with exercise is expected, we do not want any sharp pain–pain that gets worse with each rep of an exercise or any increased soreness for more than 24 hours. -

Unilateral Proximal Focal Femoral Deficiency, Fibular Aplasia, Tibial
The Egyptian Journal of Medical Human Genetics (2014) 15, 299–303 Ain Shams University The Egyptian Journal of Medical Human Genetics www.ejmhg.eg.net www.sciencedirect.com CASE REPORT Unilateral proximal focal femoral deficiency, fibular aplasia, tibial campomelia and oligosyndactyly in an Egyptian child – Probable FFU syndrome Rabah M. Shawky a,*, Heba Salah Abd Elkhalek a, Shaimaa Gad a, Shaimaa Abdelsattar Mohammad b a Pediatric Department, Genetics Unit, Ain Shams University, Egypt b Radio Diagnosis Department, Ain Shams University, Egypt Received 2 March 2014; accepted 18 March 2014 Available online 30 April 2014 KEYWORDS Abstract We report a fifteen month old Egyptian male child, the third in order of birth of healthy Short femur; non consanguineous parents, who has normal mentality, normal upper limbs and left lower limb. Limb anomaly; The right lower limb has short femur, and tibia with anterior bowing, and an overlying skin dimple. FFU syndrome; The right foot has also oligosyndactyly (three toes), and the foot is in vulgus position. There is lim- Proximal focal femoral ited abduction at the hip joint, full flexion and extension at the knee, limited dorsiflexion and plan- deficiency; tar flexion at the ankle joint. The X-ray of the lower limb and pelvis shows proximal focal femoral Fibular aplasia; deficiency, absent right fibula with shortening of the right tibia and anterior bowing of its distal Tibial campomelia; third. The acetabulum is shallow. He has a family history of congenital cyanotic heart disease. Oligosyndactyly Our patient represents most probably the first case of femur fibula ulna syndrome (FFU) in Egypt with unilateral right leg affection. -
How to Self-Bandage Your Leg(S) and Feet to Reduce Lymphedema (Swelling)
Form: D-8519 How to Self-Bandage Your Leg(s) and Feet to Reduce Lymphedema (Swelling) For patients with lower body lymphedema who have had treatment for cancer, including: • Removal of lymph nodes in the pelvis • Removal of lymph nodes in the groin, or • Radiation to the pelvis Read this resource to learn: • Who needs self-bandaging • Why self-bandaging is important • How to do self-bandaging Disclaimer: This pamphlet is for patients with lymphedema. It is a guide to help patients manage leg swelling with bandages. It is only to be used after the patient has been taught bandaging by a clinician at the Cancer Rehabilitation and Survivorship (CRS) Clinic at Princess Margaret Cancer Centre. Do not self-bandage if you have an infection in your abdomen, leg(s) or feet. Signs of an infection may include: • Swelling in these areas and redness of the skin (this redness can quickly spread) • Pain in your leg(s) or feet • Tenderness and/or warmth in your leg(s) or feet • Fever, chills or feeling unwell If you have an infection or think you have an infection, go to: • Your Family Doctor • Walk-in Clinic • Urgent Care Clinic If no Walk-in clinic is open, go to the closest hospital Emergency Department. 2 What is the lymphatic system? Your lymphatic system removes extra fluid and waste from your body. It plays an important role in how your immune system works. Your lymphatic system is made up of lymph nodes that are linked by lymph vessels. Your lymph nodes are bean-shaped organs that are found all over your body.