Calcaneal Autografts: Indications, Technique, and Complications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Skeletal Foot Structure
Foot Skeletal Structure The disarticulated bones of the left foot, from above (The talus and calcaneus remain articulated) 1 Calcaneus 2 Talus 3 Navicular 4 Medial cuneiform 5 Intermediate cuneiform 6 Lateral cuneiform 7 Cuboid 8 First metatarsal 9 Second metatarsal 10 Third metatarsal 11 Fourth metatarsal 12 Fifth metatarsal 13 Proximal phalanx of great toe 14 Distal phalanx of great toe 15 Proximal phalanx of second toe 16 Middle phalanx of second toe 17 Distal phalanx of second toe Bones of the tarsus, the back part of the foot Talus Calcaneus Navicular bone Cuboid bone Medial, intermediate and lateral cuneiform bones Bones of the metatarsus, the forepart of the foot First to fifth metatarsal bones (numbered from the medial side) Bones of the toes or digits Phalanges -- a proximal and a distal phalanx for the great toe; proximal, middle and distal phalanges for the second to fifth toes Sesamoid bones Two always present in the tendons of flexor hallucis brevis Origin and meaning of some terms associated with the foot Tibia: Latin for a flute or pipe; the shin bone has a fanciful resemblance to this wind instrument. Fibula: Latin for a pin or skewer; the long thin bone of the leg. Adjective fibular or peroneal, which is from the Greek for pin. Tarsus: Greek for a wicker frame; the basic framework for the back of the foot. Metatarsus: Greek for beyond the tarsus; the forepart of the foot. Talus (astragalus): Latin (Greek) for one of a set of dice; viewed from above the main part of the talus has a rather square appearance. -

Medial Lateral Malleolus
Acutrak 2® Headless Compression Screw System 4.7 mm and 5.5 mm Screws Supplemental Use Guide—Medial & Lateral Malleolus Acumed® is a global leader of innovative orthopaedic and medical solutions. We are dedicated to developing products, service methods, and approaches that improve patient care. Acumed® Acutrak 2® Headless Compression Screw System—4.7 mm and 5.5 mm This guide is intended for supplemental use only and is not intended to be used as a stand-alone surgical technique. Reference the Acumed Acutrak 2 Headless Compression Screw System Surgical Technique (SPF00-02) for more information. Definition Indicates critical information about a potential serious outcome to the Warning patient or the user. Indicates instructions that must be followed in order to ensure the proper Caution use of the device. Note Indicates information requiring special attention. Acumed® Acutrak 2® Headless Compression System—Supplemental Use Guide—Medial & Lateral Malleolus Table of Contents System Features ...........................................2 Surgical Techniques ........................................ 4 Fibula Fracture (Weber A and B Fractures) Surgical Technique: Acutrak 2®—5.5 .......................4 Medial Malleolus Surgical Technique: Acutrak 2®—4.7 ......................10 Ordering Information ......................................16 Acumed® Acutrak 2® Headless Compression System—Supplemental Use Guide—Medial & Lateral Malleolus System Features Headless screw design is intended to minimize soft tissue irritation D Acutrak 2 Screws Diameter -

Assessment, Management and Decision Making in the Treatment Of
Pediatric Ankle Fractures Anthony I. Riccio, MD Texas Scottish Rite Hospital for Children Update 07/2016 Pediatric Ankle Fractures The Ankle is the 2nd most Common Site of Physeal Injury in Children 10-25% of all Physeal Injuries Occur About the Ankle Pediatric Ankle Fractures Primary Concerns Are: • Anatomic Restoration of Articular Surface • Restoration of Symmetric Ankle Mortise • Preservation of Physeal Growth • Minimize Iatrogenic Physeal Injury • Avoid Fixation Across Physis in Younger Children Salter Harris Classification Prognosis and Treatment of Pediatric Ankle Fractures is Often Dictated by the Salter Harris Classification of Physeal Fractures Type I and II Fractures: Often Amenable to Closed Tx / Lower Risk of Physeal Arrest Type III and IV: More Likely to Require Operative Tx / Higher Risk of Physeal Arrest Herring JA, ed. Tachdjian’s Pediatric Orthopaedics, 5th Ed. 2014. Elsevier. Philadelphia, PA. ISOLATED DISTAL FIBULA FRACTURES Distal Fibula Fractures • The Physis is Weaker than the Lateral Ankle Ligaments – Children Often Fracture the Distal Fibula but…. – …ligamentous Injuries are Not Uncommon • Mechanism of Injury = Inversion of a Supinated Foot • SH I and II Fractures are Most Common – SH I Fractures: Average Age = 10 Years – SH II Fractures: Average Age = 12 Years Distal Fibula Fractures Lateral Ankle Tenderness SH I Distal Fibula Fracture vs. Lateral Ligamentous Injury (Sprain) Distal Fibula Fractures • Sankar et al (JPO 2008) – 37 Children – All with Open Physes, Lateral Ankle Tenderness + Normal Films – 18%: Periosteal -

Rethinking the Evolution of the Human Foot: Insights from Experimental Research Nicholas B
© 2018. Published by The Company of Biologists Ltd | Journal of Experimental Biology (2018) 221, jeb174425. doi:10.1242/jeb.174425 REVIEW Rethinking the evolution of the human foot: insights from experimental research Nicholas B. Holowka* and Daniel E. Lieberman* ABSTRACT presumably owing to their lack of arches and mobile midfoot joints Adaptive explanations for modern human foot anatomy have long for enhanced prehensility in arboreal locomotion (see Glossary; fascinated evolutionary biologists because of the dramatic differences Fig. 1B) (DeSilva, 2010; Elftman and Manter, 1935a). Other studies between our feet and those of our closest living relatives, the great have documented how great apes use their long toes, opposable apes. Morphological features, including hallucal opposability, toe halluces and mobile ankles for grasping arboreal supports (DeSilva, length and the longitudinal arch, have traditionally been used to 2009; Holowka et al., 2017a; Morton, 1924). These observations dichotomize human and great ape feet as being adapted for bipedal underlie what has become a consensus model of human foot walking and arboreal locomotion, respectively. However, recent evolution: that selection for bipedal walking came at the expense of biomechanical models of human foot function and experimental arboreal locomotor capabilities, resulting in a dichotomy between investigations of great ape locomotion have undermined this simple human and great ape foot anatomy and function. According to this dichotomy. Here, we review this research, focusing on the way of thinking, anatomical features of the foot characteristic of biomechanics of foot strike, push-off and elastic energy storage in great apes are assumed to represent adaptations for arboreal the foot, and show that humans and great apes share some behavior, and those unique to humans are assumed to be related underappreciated, surprising similarities in foot function, such as to bipedal walking. -

Free Vascularized Fibula Graft with Femoral Allograft Sleeve for Lumbar Spine Defects After Spondylectomy of Malignant Tumors Acasereport
1 COPYRIGHT Ó 2020 BY THE JOURNAL OF BONE AND JOINT SURGERY,INCORPORATED Free Vascularized Fibula Graft with Femoral Allograft Sleeve for Lumbar Spine Defects After Spondylectomy of Malignant Tumors ACaseReport Michiel E.R. Bongers, MD, John H. Shin, MD, Sunita D. Srivastava, MD, Christopher R. Morse, MD, Sang-Gil Lee, MD, and Joseph H. Schwab, MD, MS Investigation performed at Massachusetts General Hospital, Boston, Massachusetts Abstract Case: We present a 65-year-old man with an L4 conventional chordoma. Total en bloc spondylectomy (TES) of the involved vertebral bodies and surrounding soft tissues with reconstruction of the spine using a free vascularized fibula autograft (FVFG) is a proven technique, limiting complications and recurrence. However, graft fracture has occurred only in the lumbar spine in our institutional cases. We used a technique in our patient to ensure extra stability and support, with the addition of a femoral allograft sleeve encasing the FVFG. Conclusions: Our technique for the reconstruction of the lumbar spine after TES of primary malignant spinal disease using a femoral allograft sleeve encasing the FVFG is viable to consider. he treatment of primary malignant neoplasms of the spine mended a magnetic resonance imaging (MRI), but the request currently mainly relies on surgery, often in conjunction with was denied by the insurance company, and the patient T 1-3 radiotherapy .Totalen bloc spondylectomy (TES) is a widely underwent a course of physical therapy with no benefitand accepted surgical technique and has lower reported recurrence rates progression of back pain and radiculopathy. Four months compared with patients who undergo intralesional surgery3,4. -

5Th Metatarsal Fracture
FIFTH METATARSAL FRACTURES Todd Gothelf MD (USA), FRACS, FAAOS, Dip. ABOS Foot, Ankle, Shoulder Surgeon Orthopaedic You have been diagnosed with a fracture of the fifth metatarsal bone. Surgeons This tyPe of fracture usually occurs when the ankle suddenly rolls inward. When the ankle rolls, a tendon that is attached to the fifth metatarsal bone is J. Goldberg stretched. Because the bone is weaker than the tendon, the bone cracks first. A. Turnbull R. Pattinson A. Loefler All bones heal in a different way when they break. This is esPecially true J. Negrine of the fifth metatarsal bone. In addition, the blood suPPly varies to different I. PoPoff areas, making it a lot harder for some fractures to heal without helP. Below are D. Sher descriPtions of the main Patterns of fractures of the fifth metatarsal fractures T. Gothelf and treatments for each. Sports Physicians FIFTH METATARSAL AVULSION FRACTURE J. Best This fracture Pattern occurs at the tiP of the bone (figure 1). These M. Cusi fractures have a very high rate of healing and require little Protection. Weight P. Annett on the foot is allowed as soon as the Patient is comfortable. While crutches may helP initially, walking without them is allowed. I Prefer to Place Patients in a walking boot, as it allows for more comfortable walking and Protects the foot from further injury. RICE treatment is initiated. Pain should be exPected to diminish over the first four weeks, but may not comPletely go away for several months. Follow-uP radiographs are not necessary if the Pain resolves as exPected. -

Common Stress Fractures BRENT W
COVER ARTICLE PRACTICAL THERAPEUTICS Common Stress Fractures BRENT W. SANDERLIN, LCDR, MC, USNR, Naval Branch Medical Clinic, Fort Worth, Texas ROBERT F. RASPA, CAPT, MC, USN, Naval Hospital Jacksonville, Jacksonville, Florida Lower extremity stress fractures are common injuries most often associated with partic- ipation in sports involving running, jumping, or repetitive stress. The initial diagnosis can be made by identifying localized bone pain that increases with weight bearing or repet- itive use. Plain film radiographs are frequently unrevealing. Confirmation of a stress frac- ture is best made using triple phase nuclear medicine bone scan or magnetic resonance imaging. Prevention of stress fractures is most effectively accomplished by increasing the level of exercise slowly, adequately warming up and stretching before exercise, and using cushioned insoles and appropriate footwear. Treatment involves rest of the injured bone, followed by a gradual return to the sport once free of pain. Recent evidence sup- ports the use of air splinting to reduce pain and decrease the time until return to full par- ticipation or intensity of exercise. (Am Fam Physician 2003;68:1527-32. Copyright© 2003 American Academy of Family Physicians) tress fractures are among the involving repetitive use of the arms, such most common sports injuries as baseball or tennis. Stress fractures of and are frequently managed the ribs occur in sports such as rowing. by family physicians. A stress Upper extremity and rib stress fractures fracture should be suspected in are far less common than lower extremity Sany patient presenting with localized stress fractures.1 bone or periosteal pain, especially if he or she recently started an exercise program Etiology and Pathophysiology or increased the intensity of exercise. -

Foot and Ankle Systems Coding Reference Guide
Foot and Ankle Systems Coding Reference Guide Physician CPT® Code Description Arthrodesis 27870 Arthrodesis, ankle, open 27871 Arthrodesis, tibiofibular joint, proximal or distal 28705 Arthrodesis; pantalar 28715 Arthrodesis; triple 28725 Arthrodesis; subtalar 28730 Arthrodesis, midtarsal or tarsometatarsal, multiple or transverse 28735 Arthrodesis, midtarsal or tarsometatarsal, multiple or transverse; with osteotomy (eg, flatfoot correction) 28737 Arthrodesis, with tendon lengthening and advancement, midtarsal, tarsal navicular-cuneiform (eg, miller type procedure) 28740 Arthrodesis, midtarsal or tarsometatarsal, single joint 28750 Arthrodesis, great toe; metatarsophalangeal joint 28755 Arthrodesis, great toe; interphalangeal joint 28760 Arthrodesis, with extensor hallucis longus transfer to first metatarsal neck, great toe, interphalangeal joint (eg, jones type procedure) Bunionectomy 28292 Correction, hallux valgus (bunionectomy), with sesamoidectomy, when performed; with resection of proximal phalanx base, when performed, any method 28295 Correction, hallux valgus (bunionectomy), with sesamoidectomy, when performed; with proximal metatarsal osteotomy, any method 28296 Correction, hallux valgus (bunionectomy), with sesamoidectomy, when performed; with distal metatarsal osteotomy, any method 28297 Correction, hallux valgus (bunionectomy), with sesamoidectomy, when performed; with first metatarsal and medial cuneiform joint arthrodesis, any method 28298 Correction, hallux valgus (bunionectomy), with sesamoidectomy, when performed; with -
Bones of the Upper and Lower Limb Musculoskeletal Block - Lecture 1
Bones of the Upper and Lower limb Musculoskeletal Block - Lecture 1 Objective: Classify the bones of the three regions of the lower limb (Thigh, leg and foot). Memorize the main features of the – Bones of the thigh (femur & patella) – Bones of the leg (tibia & Fibula) – Bones of the foot (tarsals, metatarsals and phalanges) Recognize the side of the bone. Color index: Important In male’s slides only In female’s slides only Extra information, explanation Editing file Click here for Contact us: useful videos [email protected] Please make sure that you’re familiar with these terms Terms Meaning Example Ridge The long and narrow upper edge, angle, or crest of something The supracondylar ridges (in the distal part of the humerus) Notch An indentation, (incision) on an edge or surface The trochlear notch (in the proximal part of the ulna) Tubercles A nodule or a small rounded projection on the bone (Dorsal tubercle in the distal part of the radius) Fossa A hollow place (The Notch is not complete but the fossa is Subscapular fossa (in the concave part of complete and both of them act as the lock of the joint the scapula) Tuberosity A large prominence on a bone usually serving for Deltoid tuberosity (in the humorous) and it the attachment of muscles or ligaments ( is a bigger projection connects the deltoid muscle than the Tubercle ) Processes A V-shaped indentation (act as the key of the joint) Coracoid process ( in the scapula ) Groove A channel, a long narrow depression sure Spiral (Radial) groove (in the posterior aspect of (the humerus -
Analysis of the Talus and Calcaneus Bones from the Poole-Rose Ossuary
Louisiana State University LSU Digital Commons LSU Master's Theses Graduate School 2005 Analysis of the talus and calcaneus bones from the Poole-Rose Ossuary: a Late Woodland burial site in Ontario, Canada Adrienne Elizabeth Penney Louisiana State University and Agricultural and Mechanical College, [email protected] Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_theses Part of the Social and Behavioral Sciences Commons Recommended Citation Penney, Adrienne Elizabeth, "Analysis of the talus and calcaneus bones from the Poole-Rose Ossuary: a Late Woodland burial site in Ontario, Canada" (2005). LSU Master's Theses. 3114. https://digitalcommons.lsu.edu/gradschool_theses/3114 This Thesis is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Master's Theses by an authorized graduate school editor of LSU Digital Commons. For more information, please contact [email protected]. ANALYSIS OF THE TALUS AND CALCANEUS BONES FROM THE POOLE-ROSE OSSUARY: A LATE WOODLAND BURIAL SITE IN ONTARIO, CANADA A Thesis Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the requirements for the degree of Master of Arts in The Department of Geography and Anthropology by Adrienne Elizabeth Penney B.A. University of Evansville, 2003 August 2005 ACKNOWLEDGEMENTS I appreciate the cooperation of the Alderville First Nation, and especially Nora Bothwell, for allowing the study of the valuable Poole-Rose collection. I would like to thank Ms. Mary H. Manhein, my advisor, for all of her time, encouragement, and assistance. -

Management of Intra-Articular Fractures of the Calcaneus: Introducing a New Locking Plate
Shafa Ortho J. 2018 November; 5(4):e7991. doi: 10.5812/soj.7991. Published online 2018 October 9. Letter Management of Intra-Articular Fractures of the Calcaneus: Introducing a New Locking Plate Bijan Valiollahi 1, * and Mostafa Salariyeh 1 1Bone and Joint Reconstruction Research Center, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran *Corresponding author: Bone and Joint Reconstruction Research Center, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran. Email: [email protected] Received 2016 October 31; Revised 2018 September 22; Accepted 2018 September 27. Keywords: Calcaneus Fracture, New Plate, Sinus Tarsal Approach Dear Editor, displaced intra-articular fractures involving the posterior Fracture of the calcaneus is usually a challenging prob- facet and is ideally performed within three weeks of in- lem for orthopedic surgeons and patients. Calcaneal frac- jury. Beyond this time, separation of the fragments be- tures are the most common of tarsal bone fractures, and comes more challenging. To achieve an adequate reduc- most of them are displaced intra-articular (nearly 75%) frac- tion, surgery must be performed after soft tissue swelling tures, usually resulting from falling or motor vehicle acci- diminishes (2). dents (1). Full diminishing of soft tissue edema is demonstrated Most patients with calcaneal fractures are usually by a positive wrinkle test, indicating that surgical interven- young men in their prime working years, which results in tion may be performed safely. For the extensile lateral ap- a significant loss of economic productivity. Although sur- proach, a good skin with positive wrinkle test is needed. gical techniques and fixation implants have generally im- Concerns about high wound complication rates in the ex- proved functional outcomes, there is vast controversy as to tensile lateral approach have prompted some to improve the management of these highly complex injuries. -
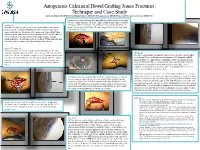
Autogenous Calcaneal Dowel Grafting Jones Fractures: Technique and Case Study Edward G
Autogenous Calcaneal Dowel Grafting Jones Fractures: Technique and Case Study Edward G. Blahous JR, DPM, FACFAS, Richard T. Bouché, DPM, FACFAS, Amol Saxena, DPM, FACFAS, FAAPSM, Chad Seidenstricker, DPM, PGY-3 A trephine is now used to obtain a bone graft plug, which will be used as an inlay graft to be placed into reamed hole. To assure a tight custom fit trephine diameter should be Introduction 1 mm greater than the reamer size. The authors’ prefer use of bone graft procured Many foot and ankle surgeons elect to treat the proximal fifth metatarsal base from the lateral calcaneal wall (Fig 6). The bone plug graft is then gently aligned and fractures near the metaphyseal-diaphyseal junction by surgical repair due to tamped into place (Fig 8). unpredictable outcomes with nonoperative management. Intramedullary fixation (IM) is the current “gold standard” and has high union rate [1]. However, there are several reports of complications with the IM technique. Notably, refracture, prominent hardware, and slow time to fracture healing [2-5]. This publication aims to describe a novel technique to treat the problematic Jones fracture. Figure 10. Intraoperative anteroposterior fluoroscopic Figure 11. Intraoperative lateral fluoroscopic view Figure 6. Incision placement with trephine in Figure 5. Visualization of recipient hole view of fracture site with graft and fixation in place. of fracture site with graft and fixation in place. Surgical Technique [6] place for safe exposure of lateral calcaneal through fracture site. The patient is placed in a lateral decubitus position with ipsilateral side facing wall. superiorly. A dorsolateral incision is made centered over the fifth metatarsal base Discussion fracture site.