Charcot Fracture in the Calcaneus After Total Knee Arthroplasty: a Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Skeletal Foot Structure
Foot Skeletal Structure The disarticulated bones of the left foot, from above (The talus and calcaneus remain articulated) 1 Calcaneus 2 Talus 3 Navicular 4 Medial cuneiform 5 Intermediate cuneiform 6 Lateral cuneiform 7 Cuboid 8 First metatarsal 9 Second metatarsal 10 Third metatarsal 11 Fourth metatarsal 12 Fifth metatarsal 13 Proximal phalanx of great toe 14 Distal phalanx of great toe 15 Proximal phalanx of second toe 16 Middle phalanx of second toe 17 Distal phalanx of second toe Bones of the tarsus, the back part of the foot Talus Calcaneus Navicular bone Cuboid bone Medial, intermediate and lateral cuneiform bones Bones of the metatarsus, the forepart of the foot First to fifth metatarsal bones (numbered from the medial side) Bones of the toes or digits Phalanges -- a proximal and a distal phalanx for the great toe; proximal, middle and distal phalanges for the second to fifth toes Sesamoid bones Two always present in the tendons of flexor hallucis brevis Origin and meaning of some terms associated with the foot Tibia: Latin for a flute or pipe; the shin bone has a fanciful resemblance to this wind instrument. Fibula: Latin for a pin or skewer; the long thin bone of the leg. Adjective fibular or peroneal, which is from the Greek for pin. Tarsus: Greek for a wicker frame; the basic framework for the back of the foot. Metatarsus: Greek for beyond the tarsus; the forepart of the foot. Talus (astragalus): Latin (Greek) for one of a set of dice; viewed from above the main part of the talus has a rather square appearance. -

Rethinking the Evolution of the Human Foot: Insights from Experimental Research Nicholas B
© 2018. Published by The Company of Biologists Ltd | Journal of Experimental Biology (2018) 221, jeb174425. doi:10.1242/jeb.174425 REVIEW Rethinking the evolution of the human foot: insights from experimental research Nicholas B. Holowka* and Daniel E. Lieberman* ABSTRACT presumably owing to their lack of arches and mobile midfoot joints Adaptive explanations for modern human foot anatomy have long for enhanced prehensility in arboreal locomotion (see Glossary; fascinated evolutionary biologists because of the dramatic differences Fig. 1B) (DeSilva, 2010; Elftman and Manter, 1935a). Other studies between our feet and those of our closest living relatives, the great have documented how great apes use their long toes, opposable apes. Morphological features, including hallucal opposability, toe halluces and mobile ankles for grasping arboreal supports (DeSilva, length and the longitudinal arch, have traditionally been used to 2009; Holowka et al., 2017a; Morton, 1924). These observations dichotomize human and great ape feet as being adapted for bipedal underlie what has become a consensus model of human foot walking and arboreal locomotion, respectively. However, recent evolution: that selection for bipedal walking came at the expense of biomechanical models of human foot function and experimental arboreal locomotor capabilities, resulting in a dichotomy between investigations of great ape locomotion have undermined this simple human and great ape foot anatomy and function. According to this dichotomy. Here, we review this research, focusing on the way of thinking, anatomical features of the foot characteristic of biomechanics of foot strike, push-off and elastic energy storage in great apes are assumed to represent adaptations for arboreal the foot, and show that humans and great apes share some behavior, and those unique to humans are assumed to be related underappreciated, surprising similarities in foot function, such as to bipedal walking. -

5Th Metatarsal Fracture
FIFTH METATARSAL FRACTURES Todd Gothelf MD (USA), FRACS, FAAOS, Dip. ABOS Foot, Ankle, Shoulder Surgeon Orthopaedic You have been diagnosed with a fracture of the fifth metatarsal bone. Surgeons This tyPe of fracture usually occurs when the ankle suddenly rolls inward. When the ankle rolls, a tendon that is attached to the fifth metatarsal bone is J. Goldberg stretched. Because the bone is weaker than the tendon, the bone cracks first. A. Turnbull R. Pattinson A. Loefler All bones heal in a different way when they break. This is esPecially true J. Negrine of the fifth metatarsal bone. In addition, the blood suPPly varies to different I. PoPoff areas, making it a lot harder for some fractures to heal without helP. Below are D. Sher descriPtions of the main Patterns of fractures of the fifth metatarsal fractures T. Gothelf and treatments for each. Sports Physicians FIFTH METATARSAL AVULSION FRACTURE J. Best This fracture Pattern occurs at the tiP of the bone (figure 1). These M. Cusi fractures have a very high rate of healing and require little Protection. Weight P. Annett on the foot is allowed as soon as the Patient is comfortable. While crutches may helP initially, walking without them is allowed. I Prefer to Place Patients in a walking boot, as it allows for more comfortable walking and Protects the foot from further injury. RICE treatment is initiated. Pain should be exPected to diminish over the first four weeks, but may not comPletely go away for several months. Follow-uP radiographs are not necessary if the Pain resolves as exPected. -
EM Cases Digest Vol. 1 MSK & Trauma
THE MAGAZINE SERIES FOR ENHANCED EM LEARNING Vol. 1: MSK & Trauma Copyright © 2015 by Medicine Cases Emergency Medicine Cases by Medicine Cases is copyrighted as “All Rights Reserved”. This eBook is Creative Commons Attribution-NonCommercial- NoDerivatives 3.0 Unsupported License. Upon written request, however, we may be able to share our content with you for free in exchange for analytic data. For permission requests, write to the publisher, addressed “Attention: Permissions Coordinator,” at the address below. Medicine Cases 216 Balmoral Ave Toronto, ON, M4V 1J9 www.emergencymedicinecases.com This book has been authored with care to reflect generally accepted practices. As medicine is a rapidly changing field, new diagnostic and treatment modalities are likely to arise. It is the responsibility of the treating physician, relying on his/her experience and the knowledge of the patient, to determine the best management plan for each patient. The author(s) and publisher of this book are not responsible for errors or omissions or for any consequences from the application of the information in this book and disclaim any liability in connection with the use of this information. This book makes no guarantee with respect to the completeness or accuracy of the contents within. OUR THANKS TO... EDITORS IN CHIEF Anton Helman Taryn Lloyd PRODUCTION EDITOR Michelle Yee PRODUCTION MANAGER Garron Helman CHAPTER EDITORS Niran Argintaru Michael Misch PODCAST SUMMARY EDITORS Lucas Chartier Keerat Grewal Claire Heslop Michael Kilian PODCAST GUEST EXPERTS Andrew Arcand Natalie Mamen Brian Steinhart Mike Brzozowski Hossein Mehdian Arun Sayal Ivy Cheng Sanjay Mehta Laura Tate Walter Himmel Jonathan Pirie Rahim Valani Dave MacKinnon Jennifer Riley University of Toronto, Faculty of Medicine EM Cases is a venture of the Schwartz/ Reisman Emergency Medicine Institute. -

Comparison of Diagnostic Accuracy of Bedside Ultrasonography and Radiography for Calcaneal Fractures in the Emergency Department
Open Access http://jept.ir Publish Free doi 10.34172/jept.2020.36 Journal of Emergency Practice and Trauma Original Article Volume 7, Issue 1, 2021, 2020, p. 17-21 Comparison of diagnostic accuracy of bedside ultrasonography and radiography for calcaneal fractures in the emergency department Majid Zamani ID , Maliheh Mazaheri ID , Farhad Heydari* ID , Babak Masoumi ID Department of Emergency Medicine, Faculty of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran Received: 1 June 2020 Abstract Accepted: 14 September 2020 Objective: Ultrasonography (US) is not the method of choice for the diagnosis of calcaneal Published online: 24 September fractures. The aim of this study was to compare the diagnostic accuracy of US with plain 2020 radiography in the diagnosis of calcaneus fractures following blunt ankle and foot trauma. *Corresponding author: Methods: In this cross-sectional study, 214 patients (over 18 years) presenting to the Farhad heydari; Emergency emergency department (ED) with suspicion of traumatic calcaneus fracture following acute Medicine Specialist; Department of Emergency Medicine, Faculty blunt trauma, were enrolled. Bedside ultrasonography was performed and interpreted by of Medicine, Isfahan University of emergency physicians. After that, plain radiography was performed. Furthermore, all the Medical Sciences, Isfahan, Iran patients were assessed by computed tomography (CT) scan as the gold standard. Alzahra Hospital, Sofeh Ave, Keshvari Results: Finally, 193 patients were enrolled with a mean age of 29.4 ± 15.7 years (85.5% Blvd., Isfahan, Iran. male). Fractures in the calcaneus were detected in 49 patients. The sensitivity and specificity Tel: +989131367643; Email: [email protected] of ultrasonography in the detection of calcaneal fractures were 83.6%, (confidence interval (CI), 69.7 –92.2) and 100% (95% CI, 96.7 –100), while the sensitivity and specificity of X-ray Competing interests: None. -

Talo-Calcaneal Distraction Ilizarov Frame: an Ergonomic Method to Manage Intra-Articular Fractures of Calcaneum
ORIGINAL ARTICLE ASIAN JOURNAL OF MEDICAL SCIENCES Talo-calcaneal distraction Ilizarov frame: an ergonomic method to manage intra-articular fractures of calcaneum Anoop Raj Singh1, Javed Ahmad 2, Vivek Kumar Shrivastava3, Pavneesh Kumar4 1Assistant Professor, Department of Orthopedics, SMMH Medical College, Saharanpur, Uttar Pradesh, India, 2,3Assistant Professor, Department of Orthopedics, Mahamaya Rajkiya Allopathic Medical College, Ambedkar Nagar, Uttar Pradesh, India, SMMH Medical College, Saharanpur, Uttar Pradesh, India, 4Assistant Professor, Department of Orthopedics, Government Doon Medical College Dehradun, India Submission: 07-03-2021 Revision: 27-05-2021 Publication: 01-07-2021 ABSTRACT Background: Principle of distraction and an indirect reduction was used to promote healing of Access this article online fractures and adequate regeneration of cartilage at the subtalar joint. Aims and Objectives: The Website: study was aimed to elaborate and develop role of Ilizarov as an alternative biological method to manage intraarticular fracture calcaneum with minimal chances of infection. http://nepjol.info/index.php/AJMS Materials and Methods: Twenty-one patients were studied and the mean age of patients DOI: 10.3126/ajms.v12i7.35459 was 40.7 years (span: 20 to 65 years). Sanders CT classification was used to divide into E-ISSN: 2091-0576 type II, 11 (52.38%); type III, 7 (33.33%) and type IV, 3 (14.28%). The average follow-up P-ISSN: 2467-9100 was 17.2 months (range: 6 to 24 months). AOFAS scale for ankle and hindfoot was used for assessment of patients- 7 (33.33%) excellent, 7 (33.33%) good, 3 (14.28%) fair, and 4 Copyright (c) 2021 Asian Journal of (19.04%) poor results. -

Calcaneal Fracture and Rehabilitation
1 Calcaneal Fracture and Rehabilitation Surgical Indications and Considerations Anatomic Considerations: The calcaneus articulates with the talus superiorly at the subtalar joint. The three articulating surfaces of the subtalar joint are the: anterior, middle, and posterior facets, with the posterior facet representing the major weight-bearing surface. The subtalar joint is responsible for the majority of foot inversion/eversion (or pronation/supination). The interosseous ligament and medial, lateral, and posterior talocalcaneal ligaments provide additional support for the joint. The tibial artery, nerve, posterior tibial tendon, and flexor hallucis longus tendon are located medially to the calcaneus and are at risk for impingement with a calcaneal fracture, as are the peroneal tendons located on the lateral aspect of the calcaneus. The calcaneus serves three major functions: 1) acts as a foundation and support for the body’s weight, 2) supports the lateral column of the foot and acts as the main articulation for inversion/eversion, and 3) acts as a lever arm for the gastrocnemius muscle complex. Pathogenesis: Fractures of the calcaneal body, anterior process, sustentaculum tali, and superior tuberosity are known as extra-articular fractures and usually occur as a result of blunt force or sudden twisting. Fractures involving any of the three subtalar articulating surfaces are known as intra-articular fractures and are common results of: a fall from a height usually 6 feet or more, a motor vehicle accident (MVA), or an impact on a hard surface while running or jumping. Intra-articular fractures are commonly produced by axial loading; a combination of shearing and compression forces produce both the primary and secondary fracture lines. -

Radiographic Evaluation of Calcaneal Fractures; to Measure Or Not to Measure T
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Erasmus University Digital Repository Radiographic evaluation of calcaneal fractures; To measure or not to measure T. Schepers, A.Z. Ginai, P.G.H. Mulder, P. Patka Skeletal Radiol 2007;36(9):847-852 Abstract Objective The aim of this study was to correlate the functional outcome after treatment for displaced intra-articular calcaneal fracture with plain radiography. Design Prognostic study of a retrospective cohort with concurrent follow-up. Patients A total of 33 patients with a unilateral calcaneal fracture and a minimum follow-up of 13 months participated. Patients filled in three disease-specific questionnaires, graded their satisfaction and the indication for an arthrodesis was noted. Standardised radiographs were made of the previously injured side and the normal (control) side. Different angles and distances were measured on these radiographs and compared with values described in the literature. The differences in values in angles and distances between the injured and uninjured (control) foot were correlated with the outcome of the questionnaires, and the indication for an arthrodesis. Results None of the angles correlated with the disease-specific outcome scores. Of the angles only the tibiotalar angle correlated with the VAS (r=0.35, p=0.045) and only the absolute foot height correlated with the indication for an arthrodesis (odds=0.70, CI=0.50–0.99). Conclusions In this study the radiographic evaluation correlated poorly with the final outcome. Measurements on plain radiographs seem not to be useful in determining outcome after intra-articular calcaneal fractures. -
Analysis of the Talus and Calcaneus Bones from the Poole-Rose Ossuary
Louisiana State University LSU Digital Commons LSU Master's Theses Graduate School 2005 Analysis of the talus and calcaneus bones from the Poole-Rose Ossuary: a Late Woodland burial site in Ontario, Canada Adrienne Elizabeth Penney Louisiana State University and Agricultural and Mechanical College, [email protected] Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_theses Part of the Social and Behavioral Sciences Commons Recommended Citation Penney, Adrienne Elizabeth, "Analysis of the talus and calcaneus bones from the Poole-Rose Ossuary: a Late Woodland burial site in Ontario, Canada" (2005). LSU Master's Theses. 3114. https://digitalcommons.lsu.edu/gradschool_theses/3114 This Thesis is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Master's Theses by an authorized graduate school editor of LSU Digital Commons. For more information, please contact [email protected]. ANALYSIS OF THE TALUS AND CALCANEUS BONES FROM THE POOLE-ROSE OSSUARY: A LATE WOODLAND BURIAL SITE IN ONTARIO, CANADA A Thesis Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the requirements for the degree of Master of Arts in The Department of Geography and Anthropology by Adrienne Elizabeth Penney B.A. University of Evansville, 2003 August 2005 ACKNOWLEDGEMENTS I appreciate the cooperation of the Alderville First Nation, and especially Nora Bothwell, for allowing the study of the valuable Poole-Rose collection. I would like to thank Ms. Mary H. Manhein, my advisor, for all of her time, encouragement, and assistance. -

Management of Intra-Articular Fractures of the Calcaneus: Introducing a New Locking Plate
Shafa Ortho J. 2018 November; 5(4):e7991. doi: 10.5812/soj.7991. Published online 2018 October 9. Letter Management of Intra-Articular Fractures of the Calcaneus: Introducing a New Locking Plate Bijan Valiollahi 1, * and Mostafa Salariyeh 1 1Bone and Joint Reconstruction Research Center, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran *Corresponding author: Bone and Joint Reconstruction Research Center, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran. Email: [email protected] Received 2016 October 31; Revised 2018 September 22; Accepted 2018 September 27. Keywords: Calcaneus Fracture, New Plate, Sinus Tarsal Approach Dear Editor, displaced intra-articular fractures involving the posterior Fracture of the calcaneus is usually a challenging prob- facet and is ideally performed within three weeks of in- lem for orthopedic surgeons and patients. Calcaneal frac- jury. Beyond this time, separation of the fragments be- tures are the most common of tarsal bone fractures, and comes more challenging. To achieve an adequate reduc- most of them are displaced intra-articular (nearly 75%) frac- tion, surgery must be performed after soft tissue swelling tures, usually resulting from falling or motor vehicle acci- diminishes (2). dents (1). Full diminishing of soft tissue edema is demonstrated Most patients with calcaneal fractures are usually by a positive wrinkle test, indicating that surgical interven- young men in their prime working years, which results in tion may be performed safely. For the extensile lateral ap- a significant loss of economic productivity. Although sur- proach, a good skin with positive wrinkle test is needed. gical techniques and fixation implants have generally im- Concerns about high wound complication rates in the ex- proved functional outcomes, there is vast controversy as to tensile lateral approach have prompted some to improve the management of these highly complex injuries. -

Paget's Disease of Bone Affecting Peripheral Limb
J Bone Metab 2020;27(1):71-75 https://doi.org/10.11005/jbm.2020.27.1.71 pISSN 2287-6375 eISSN 2287-7029 Case Report Paget’s Disease of Bone Affecting Peripheral Limb: Difficulties in Diagnosis: A Case Report Jun-Ku Lee1, Yun Kyung Kang2, Pei Wei Wang1, Soo Min Hong3 1Department of Orthopaedic Surgery, Seoul Paik Hospital, Inje University College of Medicine, Seoul; 2Department of Pathology, Seoul Paik Hospital, Inje University College of Medicine, Seoul; 3Department of Internal Medicine, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea Corresponding author In terms of management of Paget’s disease of bone (PDB), early diagnosis and proper Soo Min Hong management achieving remission is essential with lifelong specialist follow-up. We pres- Department of Internal Medicine, Seoul Paik ent the case of a 40-year-old woman with PDB affecting mainly the distal extremities Hospital, Inje University College of Medicine, (ankle and wrist). The patient visited our hospital in 2012 with heel pain. Plain radiogra- Mareunnae-ro 9, Jung-gu, Seoul 04551, Korea phy revealed osteoporosis, and a bone scan revealed hot uptake. Initial laboratory inves- Tel: +82-2-2270-0001 tigations showed normal serum calcium, 25-hydroxy-vitamin D, and parathyroid hor- Fax: +82-2-2270-5289 mone levels; however, osteocalcin, C-terminal telopeptide of type I collagen, and bone E-mail: [email protected] alkaline phosphatase levels were elevated. A bone mineral density scan showed T- and Z-scores of -2.5 and -2.7, respectively, and bisphosphonate treatment was initiated. Bi- Received: December 25, 2019 opsy performed on the calcaneal lateral wall revealed inconclusive findings. -
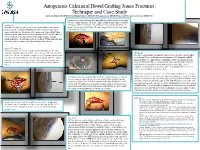
Autogenous Calcaneal Dowel Grafting Jones Fractures: Technique and Case Study Edward G
Autogenous Calcaneal Dowel Grafting Jones Fractures: Technique and Case Study Edward G. Blahous JR, DPM, FACFAS, Richard T. Bouché, DPM, FACFAS, Amol Saxena, DPM, FACFAS, FAAPSM, Chad Seidenstricker, DPM, PGY-3 A trephine is now used to obtain a bone graft plug, which will be used as an inlay graft to be placed into reamed hole. To assure a tight custom fit trephine diameter should be Introduction 1 mm greater than the reamer size. The authors’ prefer use of bone graft procured Many foot and ankle surgeons elect to treat the proximal fifth metatarsal base from the lateral calcaneal wall (Fig 6). The bone plug graft is then gently aligned and fractures near the metaphyseal-diaphyseal junction by surgical repair due to tamped into place (Fig 8). unpredictable outcomes with nonoperative management. Intramedullary fixation (IM) is the current “gold standard” and has high union rate [1]. However, there are several reports of complications with the IM technique. Notably, refracture, prominent hardware, and slow time to fracture healing [2-5]. This publication aims to describe a novel technique to treat the problematic Jones fracture. Figure 10. Intraoperative anteroposterior fluoroscopic Figure 11. Intraoperative lateral fluoroscopic view Figure 6. Incision placement with trephine in Figure 5. Visualization of recipient hole view of fracture site with graft and fixation in place. of fracture site with graft and fixation in place. Surgical Technique [6] place for safe exposure of lateral calcaneal through fracture site. The patient is placed in a lateral decubitus position with ipsilateral side facing wall. superiorly. A dorsolateral incision is made centered over the fifth metatarsal base Discussion fracture site.