Pharmaceutical Compounding and Dispensing Compounding and Dispensing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OHAUS New Scout Balance Range
Catalogue OHAUS new Scout Balance Range Touchscreen Page 121 Memmert Ovens & Incubators New bollé German Made Page 140 Rush Plus Small Has Arrived Page 77 Schott-DURAN Youtility Bottles A New Age Page 6 SAVINGS Up to 70% off major brands Bacto Laboratories Feb 2018 BactoIssue Laboratories 7.5 Pty Ltd - Phone (02) 9823-9000Proudly - Email [email protected] Supplying - (prices Science excl GST) Since 1966 1 Contents A Centrifuge 145 Flask, Volumetric Glass 17 Alcohol Wipes 55 Centrifuge Tube, Glass 24 Flask, Volumetric Plastic 29 Analytical Balance 117 Centrifuge Tube, Plastic 44 Forceps 88 Aspirator Bottle, Plastic 42 Chemicals 67 Forceps, Artery 92 Autoclave Indicators 59 Clamps, Bosshead 96 Fridge Thermometers 102 Autoclave Tape 59 Clamps, Burettes 97 Funnel, Glass 15 Autoclave Waste Bags 61 Clamps, Retort 96 Funnel, Plastic 30 Clinical Centrifuge 145 G - H B Coats, Laboratory 74 Gloves, Examination 72 Bacticinerator 82 Cold Bricks 69 Gloves, Safety 71 Bags, Waste 61 Colony Counter 81 Gowns 75 Balance, Moisture 119 Conductivity Meter 109 Hand Wash, Alcohol 55 Balances 116 Conical Measure, Plastic 27 Hand Wash, Cleanser 56 Batteries 102 Contaminated Waste Bags 62 Hand Wash, Sanitiser 55 Beaker, Glass 11 Coplin Jar 53 Hockey Stick 50 Beaker, Plastic 27 Corrosive Cabinets 85 Hotplate 124 Bench Roll 58 Cover Slips, Glass 52 Hotplate Stirrer 124 Biju McCartney Bottle 25 Cryo Vial, Plastic 37 Hygrometers 102 Bins, Broken Glass 61 Culture Media 50 I Bins, Chemotherapy 65 Culture Tube, Glass 24 Incubator 138 Bins, Contaminated Waste 61 Cuvettes, -
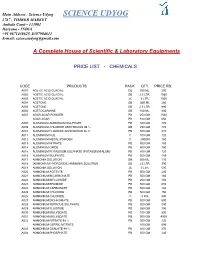
Science Udyog SCIENCE UDYOG 2767 , TIMBER MARKET Ambala Cantt - 133001 Haryana - INDIA +91 9671438625 ,8397904611 E-Mail: [email protected]
Main Address : Science Udyog SCIENCE UDYOG 2767 , TIMBER MARKET Ambala Cantt - 133001 Haryana - INDIA +91 9671438625 ,8397904611 E-mail: [email protected] A Complete House of Scientific & Laboratory Equipments PRICE LIST - CHEMICALS CODE PRODUCTS PACK QTY. PRICE RS. A001 ACETIC ACID GLACIAL GB 500 ML. 200 A002 ACETIC ACID GLACIAL GB 2.5 LTR. 1080 A003 ACETIC ACID GLACIAL JC 5 LTR. 1500 A004 ACETONE GB 500 ML 260 A005 ACETONE GB 2.5 LTR. 990 A006 ACETOCARMINE GB 100 ML. 800 A007 AGAR AGAR POWDER PB 250 GM 1500 AGAR AGAR PB 100 GM 650 A008 ALUMINIUM AMMONIUM SULPHATE PB 500 GM 170 A009 ALUMINIUM CHLORIDE ANHYDROUS 98 % GB 250 GM 170 A010 ALUMINIUM FLUORIDE ANHYDROUS 96 % PB 500 GM 410 A011 ALUMINIUM FOIL C 100 GM 120 A012 ALUMINIUM METAL POWDER C 250GM 180 A013 ALUMINIUM NITRATE PB 500 GM 180 A014 ALUMINIUM OXIDE PB 500 GM 150 A015 ALUMINIUM POTASSIUM SULPHATE (POTASSIUM ALUM) PB 500 GM 120 A016 ALUMINIUM SULPHATE PB 500 GM 148 A017 AMMONIA SOLUTION GB 500 ML. 110 A018 (AMMONIUM HYDROXIDE) AMMONIA SOLUTION GB 2.5 LTR. 390 A019 AMMONIA SOLUTION JC 5 LTR. 590 A020 AMMONIUM ACETATE PB 500 GM 240 A021 AMMONIUM BICARBONATE PB 500 GM 180 A022 AMMONIUM BIFLUORIDE PB 250 GM 156 A023 AMMONIUM BROMIDE PB 500 GM 680 A024 AMMONIUM CARBONATE PB 500 GM 194 A025 AMMONIUM CHLORIDE PB 500 GM 150 A026 AMMONIUM CHLORIDE C 5 KG. 990 A027 AMMONIUM DICHROMATE PB 500 GM 690 A028 AMMONIUM FERROUS SULPHATE PB 500 GM 240 A029 AMMONIUM FLUORIDE PB 250 GM 196 A030 AMMONIUM MOLYBDATE PB 100 GM 890 A031 AMMONIUM MOLYBDATE PB 500 GM 4500 A032 AMMONIUM NITRATE 98 % PB 500 GM 136 AMMONIUM CERRIC NITRATE 100 GM 595 A033 AMMONIUM OXALATE 99 % PB 500 GM 270 A034 AMMONIUM PHOSPHATE PB 500 GM 240 A035 AMMONIUM SULPHATE PB 500GM 142 A036 AMYL ACETATE ISO GB 500 ML. -

Pharmaceutical Compounding and Dispensing Sample Chapter
Copyright Pharmaceutical Press www.pharmpress.com 6 Solutions Introduction and overview 101 Gargles and mouthwashes 105 General principles of solution preparation 103 Enemas and douches 105 Solubility 103 External solutions 105 Stability 103 Lotions 105 General method 103 Liniments 105 Oral solutions 104 Applications 105 Elixirs 104 Collodions 106 Linctuses 105 Worked examples 106 Syrups 105 Summary of essential principles relating to solutions 112 Mixtures 105 Packaging 112 Draughts 105 Discard dates 112 Spirits 105 Labelling 113 Paediatric drops 105 Introduction and overview Essentially a solution is a homogeneous liquid preparation that contains one or more dissolved med- Solutions are one of the oldest dosage forms used in the icaments. Since, by definition, active ingredients are treatment of patients and afford rapid and high dissolved within the vehicle, uniform doses by volume absorption of soluble medicinal products. Therefore, may be obtained without any need to shake the for- the compounding of solutions retains an important mulation. This is an advantage over some other for- place in therapeutics today. Owing to the simplicity mulation types (e.g. suspensions, see Chapter 7). and hence the speed of preparation of an ad hoc for- In general, water is chosen as the vehicle in which mulation, they are of particular use for individuals medicaments are dissolved, as it is non-toxic, non- who have difficulty in swallowing solid dosage forms irritant, tasteless, relatively cheap, and many drugs (for example paediatric, geriatric, intensive care and are water soluble. Problems may be encountered psychiatric patients), where compliance needs to be where active drugs are not particularly water soluble checked on administration (for example in prisons or or suffer from hydrolysis in aqueous solution. -

OHAUS New Scout Balance Range
Catalogue OHAUS new Scout Balance Range Touchscreen Page 121 Memmert Ovens & Incubators New bollé German Made Page 140 Rush Plus Small Has Arrived Page 77 Schott-DURAN Youtility Bottles A New Age Page 6 SAVINGS Up to 70% off major brands Bacto Laboratories June 2017 BactoIssue Laboratories 6.8 Pty Ltd - Phone (02) 9823-9000Proudly - Email [email protected] Supplying - (prices Science excl GST) Since 1966 1 Contents A Centrifuge 145 Flask, Volumetric Glass 17 Alcohol Wipes 55 Centrifuge Tube, Glass 24 Flask, Volumetric Plastic 29 Analytical Balance 117 Centrifuge Tube, Plastic 44 Forceps 88 Aspirator Bottle, Plastic 42 Chemicals 67 Forceps, Artery 92 Autoclave Indicators 59 Clamps, Bosshead 96 Fridge Thermometers 102 Autoclave Tape 59 Clamps, Burettes 97 Funnel, Glass 15 Autoclave Waste Bags 61 Clamps, Retort 96 Funnel, Plastic 30 Clinical Centrifuge 145 G - H B Coats, Laboratory 74 Gloves, Examination 72 Bacticinerator 82 Cold Bricks 69 Gloves, Safety 71 Bags, Waste 61 Colony Counter 81 Gowns 75 Balance, Moisture 119 Conductivity Meter 109 Hand Wash, Alcohol 55 Balances 116 Conical Measure, Plastic 27 Hand Wash, Cleanser 56 Batteries 102 Contaminated Waste Bags 62 Hand Wash, Sanitiser 55 Beaker, Glass 11 Coplin Jar 53 Hockey Stick 50 Beaker, Plastic 27 Corrosive Cabinets 85 Hotplate 124 Bench Roll 58 Cover Slips, Glass 52 Hotplate Stirrer 124 Biju McCartney Bottle 25 Cryo Vial, Plastic 37 Hygrometers 102 Bins, Broken Glass 61 Culture Media 50 I Bins, Chemotherapy 65 Culture Tube, Glass 24 Incubator 138 Bins, Contaminated Waste 61 Cuvettes, -

OHAUS Balances Navigator Range
Catalogue OHAUS Balances Navigator Range Has Landed Page 120 Parafilm M New Frontier Up to 60% Off Page 4 Centrifuges German Made Page 148 Bollé Safety Schott-DURAN Rush Plus Small Has Arrived Youtility B ottles Page 77 A New Age SAVINGS Up to 70% off major brands Bacto Laboratories Nov 2020 BactoIssue Laboratories 15.0 Pty Ltd - Phone (02) 9823-9000Proudly - Email [email protected] Supplying - (prices Science excl GST) Since 1966 1 Contents A Centrifuge 145 Flask, Volumetric Glass 17 Alcohol Wipes 55 Centrifuge Tube, Glass 24 Flask, Volumetric Plastic 29 Analytical Balance 117 Centrifuge Tube, Plastic 44 Forceps 88 Aspirator Bottle, Plastic 42 Chemicals 67 Forceps, Artery 92 Autoclave Indicators 59 Clamps, Bosshead 96 Fridge Thermometers 102 Autoclave Tape 59 Clamps, Burettes 97 Funnel, Glass 15 Autoclave Waste Bags 61 Clamps, Retort 96 Funnel, Plastic 30 Clinical Centrifuge 145 G - H B Coats, Laboratory 74 Gloves, Examination 72 Bacticinerator 82 Cold Bricks 69 Gloves, Safety 71 Bags, Waste 61 Colony Counter 81 Gowns 75 Balance, Moisture 119 Conductivity Meter 109 Hand Wash, Alcohol 55 Balances 116 Conical Measure, Plastic 27 Hand Wash, Cleanser 56 Batteries 102 Contaminated Waste Bags 62 Hand Wash, Sanitiser 55 Beaker, Glass 11 Coplin Jar 53 Hockey Stick 50 Beaker, Plastic 27 Corrosive Cabinets 85 Hotplate 124 Bench Roll 58 Cover Slips, Glass 52 Hotplate Stirrer 124 Biju McCartney Bottle 25 Cryo Vial, Plastic 37 Hygrometers 102 Bins, Broken Glass 61 Culture Media 50 I Bins, Chemotherapy 65 Culture Tube, Glass 24 Incubator 138 Bins, -
I Experiments and Scientific Methods
Davorka Rujevčan English for Food Technology Students – part I VELEUČILIŠTE U KARLOVCU KARLOVAC, 2014. Autor: Davorka Rujevčan, mag.educ.philol.angl. Recenzenti: Vesna Vyroubal, mag.educ. Dubravka Vuljanić, prof. Mr.sc.Vesna Cigan Nakladnik: Veleučilište u Karlovcu Za nakladnika: dr.sc. Branko Wasserbauer ISBN 978-953-7343-73-6 Copyright © Veleučilište u Karlovcu Contents Unit I Experiments and Scientific Methods 1.1 Experiments: Basic Terms – text 1.2 Text comprehension and vocabulary exercises 1.3 Extracting iron from breakfast cereals (an example of an experiment)-gap filling exercise 1.4 Grammar Present Simple tense active and passive 1.5 The Invention of Coca Cola 1.6 Speaking exercises Unit II Laboratory glassware 2.1 Laboratory Glassware – text 2.2 Text comprehension and vocabulary exercise 2.3 Grammar – word formation (prefixes and suffixes) 2.4 Cleaning Laboratory Glassware – gap filling exercise 2.5 Vocabulary exercises – matching words to definitions 2.6 Speaking exercises Unit III Elements, periodic table of elements and states of matter 3.1 Elements, Periodic Table of Elements – text 3.2 Vocabulary exercise – matching elements to symbols and descriptions 3.3 Matter and States of Matter - physical and chemical changes 3.4 Grammar – adjective noun transformation 3.5 Speaking exercises Unit IV Food packaging 4.1 Food packaging – text 4.2 Text comprehension 4.3 Vocabulary exercises 4.4 Grammar – countable and uncountable nouns 4.5 Speaking and discussion Unit V Nutritional information 5.1 Nutritional labelling in the USA and in the UK - text 5.2 Text comprehension and vocabulary exercises 5.3 Grammar – comparison of adjectives 5.4 Speaking and discussion exercises Appendices Irregular verbs Symbols, expressions and formulae Conversions Unit I Experiments and scientific methods Pre-reading exercise: Do you know who Barnett Rosenberg is? What did he discover? What is an experiment? How would you define and describe it? Have you ever done any experiments? Experiments – basic terms An experiment is a test or a trial. -

Testing of Metal Volumetric Standards
3. t/ •/ ; Science Docs. NBS MONOGRAPH 62 Testing of Metal Volumetric Standards U.S. DEPARTMENT OF COMMERCE NATIONAL BUREAU OF STANDARDS THE NATIONAL BUREAU OF STANDARDS Functions and Activities The functions of the National Bureau of Standards are set forth in the Act of Congress, March 3, 1901, as amended by Congress in Public Law 619, 1950. These include the develop ment and maintenance of the national standards of measurement and the provision of means and methods for making measurements consistent with these standards; the determination of physical constants and properties of materials; the development of methods and instruments for testing materials, devices, and structures; advisory services to government agencies on scientific and technical problems; invention and development of devices to serve special needs of the Government; and the development of standard practices, codes, and specifications. The work includes basic and applied research, development, engineering, instrumentation, testing, evaluation, calibration services, and various consultation and information services. Research projects are also performed for other government agencies when the work relates to and supplements the basic program of the Bureau or when the Bureau's unique competence is required. The scope of activities is suggested by the listing of divisions and sections on the inside of the back cover. Publications The results of the Bureau's research are published either in the Bureau's own series of publications or in the journals of professional and scientific societies. The Bureau itself publishes three periodicals available from the Government Printing Office: The Journal of Research, published in four separate sections, presents complete scientific and technical papers; the Technical News Bulletin presents summary and preliminary reports on work in progress; and CRPL Ionospheric Predictions provides data for determining the best frequencies to use for radio communications throughout the world. -

POLYLAB PRICE LIST 2019 Kundli, Distt Sonipat, Haryana-131028 (INDIA)
PolyLab Industries Pvt. Ltd. Plot No 13 , HSIIDC , Phase-1, Industrial Area, POLYLAB PRICE LIST 2019 Kundli, Distt Sonipat, Haryana-131028 (INDIA) PACKING Price Price HSN CODE NO. PARTICULARS (Per (Pcs) (Per Pc) Pack) CODE 11101 Beaker 50 ml 12 8.00 96.00 39269099 11102 Beaker 100 ml 12 9.00 108.00 39269099 11104 Beaker 250 ml 12 20.00 240.00 39269099 11105 Beaker 500 ml 12 27.00 324.00 39269099 11106 Beaker 1000 ml 6 46.00 276.00 39269099 11107 Beaker 2000 ml 6 90.00 540.00 39269099 11110 Beaker (Euro Design) 25 ml 12 9.00 108.00 39269099 11111 Beaker (Euro Design) 50 ml 12 9.00 108.00 39269099 11112 Beaker (Euro Design) 100 ml 12 10.50 126.00 39269099 11113 Beaker (Euro Design) 250 ml 12 18.00 216.00 39269099 11114 Beaker (Euro Design) 500 ml 12 27.00 324.00 39269099 11115 Beaker (Euro Design) 1000 ml 6 46.00 276.00 39269099 11116 Beaker (Euro Design) 2000 ml 6 80.00 480.00 39269099 11117 Beaker (Euro Design) 5000 ml 2 230.00 460.00 39269099 11151 Beaker (Printed Graduation) 50 ml 12 14.00 168.00 39269099 11152 Beaker (Printed Graduation) 100 ml 12 16.00 192.00 39269099 11153 Beaker (Printed Graduation) 250 ml 12 27.00 324.00 39269099 11154 Beaker (Printed Graduation) 500 ml 12 42.00 504.00 39269099 11155 Beaker (Printed Graduation) 1000 ml 6 80.00 480.00 39269099 11156 Beaker (Printed Graduation) 2000 ml 6 140.00 840.00 39269099 11157 Beaker (Printed Graduation) 5000 ml 2 300.00 600.00 39269099 11158 Beaker (Printed Graduation) 10000 ml 2 600.00 1200.00 39269099 11501 Burette 25 ml 10 220.00 2200.00 39269099 11502 Burette 50 ml 10 -

1455189355674.Pdf
THE STORYTeller’S THESAURUS FANTASY, HISTORY, AND HORROR JAMES M. WARD AND ANNE K. BROWN Cover by: Peter Bradley LEGAL PAGE: Every effort has been made not to make use of proprietary or copyrighted materi- al. Any mention of actual commercial products in this book does not constitute an endorsement. www.trolllord.com www.chenaultandgraypublishing.com Email:[email protected] Printed in U.S.A © 2013 Chenault & Gray Publishing, LLC. All Rights Reserved. Storyteller’s Thesaurus Trademark of Cheanult & Gray Publishing. All Rights Reserved. Chenault & Gray Publishing, Troll Lord Games logos are Trademark of Chenault & Gray Publishing. All Rights Reserved. TABLE OF CONTENTS THE STORYTeller’S THESAURUS 1 FANTASY, HISTORY, AND HORROR 1 JAMES M. WARD AND ANNE K. BROWN 1 INTRODUCTION 8 WHAT MAKES THIS BOOK DIFFERENT 8 THE STORYTeller’s RESPONSIBILITY: RESEARCH 9 WHAT THIS BOOK DOES NOT CONTAIN 9 A WHISPER OF ENCOURAGEMENT 10 CHAPTER 1: CHARACTER BUILDING 11 GENDER 11 AGE 11 PHYSICAL AttRIBUTES 11 SIZE AND BODY TYPE 11 FACIAL FEATURES 12 HAIR 13 SPECIES 13 PERSONALITY 14 PHOBIAS 15 OCCUPATIONS 17 ADVENTURERS 17 CIVILIANS 18 ORGANIZATIONS 21 CHAPTER 2: CLOTHING 22 STYLES OF DRESS 22 CLOTHING PIECES 22 CLOTHING CONSTRUCTION 24 CHAPTER 3: ARCHITECTURE AND PROPERTY 25 ARCHITECTURAL STYLES AND ELEMENTS 25 BUILDING MATERIALS 26 PROPERTY TYPES 26 SPECIALTY ANATOMY 29 CHAPTER 4: FURNISHINGS 30 CHAPTER 5: EQUIPMENT AND TOOLS 31 ADVENTurer’S GEAR 31 GENERAL EQUIPMENT AND TOOLS 31 2 THE STORYTeller’s Thesaurus KITCHEN EQUIPMENT 35 LINENS 36 MUSICAL INSTRUMENTS -

LISTA DE PRECIOS KARTELL 2017 Catalogo Num
LISTA DE PRECIOS KARTELL 2017 Catalogo Num. Parte Descripcion Precio de Lista MN 130 0013000 TEST TUBE RACK 10 PLACES 112.47 131 0013100 TEST TUBE RACK 9 PLACES 120.40 134 0013400 TEST TUBE RACK HOLDER 141.93 135 0013500 TEST TUBE RACK 8 PLACES 132.94 139 0013900 BURETTE HOLDER 1 PLACE 337.61 140 0014000 BURETTE HOLDER 2 PLACES 426.27 142 0014200 INSTRUMENT JAR, Ø 60 mm 162.40 143 0014300 INSTRUMENT JAR, Ø 90 mm 224.88 145 0014500 ANALYTICAL FUNNELS, Ø 25 mm 17.35 146 0014600 ANALYTICAL FUNNELS, Ø 35 mm 20.42 147 0014700 ANALYTICAL FUNNELS, Ø 50 mm 24.81 148 0014800 ANALYTICAL FUNNELS, Ø 65 mm 40.73 150 0015000 ANALYTICAL FUNNELS, Ø 80 mm 50.57 152 0015200 ANALYTICAL FUNNELS, Ø 100 mm 62.00 153 0015300 ANALYTICAL FUNNELS, Ø 120 mm 66.55 155 0015500 ANALYTICAL FUNNELS, Ø 150 mm 115.11 156 0015600 ANALYTICAL FUNNELS, Ø 180 mm 154.52 162 0016200 LONG FUNNELS DIAM. 60 mm 118.76 164 0016400 LONG FUNNELS, Ø 80 mm 134.90 165 0016500 LONG FUNNELS, Ø 100 mm 150.18 166 0016600 POWDER FUNNELS, Ø 180 mm 102.57 167 0016700 POWDER FUNNELS, Ø 80 mm 50.94 168 0016800 POWDER FUNNELS, Ø 100 mm 56.76 169 0016900 POWDER FUNNELS, Ø 120 mm 66.18 170 0017000 POWDER FUNNELS, Ø 150 mm 82.89 171 0017100 POWDER FUNNEL, Ø 60 mm 23.59 172 0017200 FUNNELS, Ø 100 mm 28.04 173 0017300 FUNNELS, Ø 120 mm 33.38 174 0017400 FUNNELS, Ø 140 mm 53.11 175 0017500 FUNNELS, Ø 180 mm 95.59 176 0017600 FUNNELS, Ø 210 mm 119.34 177 0017700 FUNNELS, Ø 250 mm 171.66 178 0017800 FUNNELS, Ø 300 mm 225.67 179 0017900 WASH BOTTLES, 50 ml 38.46 180 0018000 WASH BOTTLES, 100 ml 41.79 182 0018200 WASH BOTTLES, 250 ml 53.43 183 0018300 WASH BOTTLES, 500 ml 60.73 PROVEEDOR DE LABORATORIOS, S.A. -

Weights and Measures Laws Or Cap
LAWS OF KENYA WEIGHTS AND MEASURES ACT CHAPTER 513 Revised Edition 2012 [1993] Published by the National Council for Law Reporting with the Authority of the Attorney-General www.kenyalaw.org [Rev. 2012] CAP. 513 Weights and Measures CHAPTER 513 WEIGHTS AND MEASURES ACT ARRANGEMENT OF SECTIONS PART I – PRELIMINARY Section 1. Short title. 2. Interpretation. PART II – UNITS OF MEASUREMENT 3. Units of measurement. 4. Measurement of weight. 5. Measurement of length. 6. Measurement of time. 7. Measurement of electric current. 8. Measurement of thermodynamic temperature. 9. Measurement of luminous intensity. 10. Measurement of amount of substance. 11. Offence to use unauthorized units of measurement. PART III – STANDARDS OF MEASUREMENT 12. Kenya primary standards. 13. Kenya primary reference standards. 14. Secondary standards to be procured. 15. Secondary reference standards. 16. Working standards and testing equipment. 17. Testing of standards and equipment of other institutions. PART IV – WEIGHING AND MEASURING FOR TRADE 18. Meaning of “use for trade”. 19. Units of measurement, weights and measures lawful for use for trade. 20. Offences for use or possession of certain weighing or measuring instruments. 21. Offences relating to false or unjust weights, measures or weighing or measuring instruments. 22. Mode of use of measure of capacity. 23. Offences relating to fraud in the use of weights, measures or weighing and measuring instruments. 24. What weight, measure, weighing or measuring instruments is unjust. 25. Offences for sale of incorrect weights, measures, weighing or measuring instruments. 26. Offences in connection with stamping of weights, measures, weighing or measuring instruments. 27. Verification of weights, measures, weighing of measuring instruments. -

Pharmaceutical Calculation Lab: 1 Instruments Used in Pharmaceutical Preparation
University of Anbar College of Pharmacy Pharmaceutical calculation Lab: 1 The pharmaceutical preparation, as the final forms used for medication must be effective and safe. It should be accurate quantitatively and qualitatively. Quantitatively: It means the amount (wt. or vol.) of the ingredient be accurate. Qualitatively: It means the identity of the ingredient be certain. Instruments used in pharmaceutical preparation 1. A watch glass is a circular, slightly convex-concave piece of glass used in chemistry as a surface to evaporate a liquid, to hold solids while being weighed, or as a cover for a beaker. 2. Test tubes are widely used by chemists to hold, mix, or heat small quantities of solid or liquid chemicals, especially for qualitative experiments and assays. Their round bottom and straight sides minimize mass loss when pouring, make them easier to clean, and allow convenient monitoring of the contents. The long, narrow neck slows down the spreading of vapors and gases to the environment. 3. Beaker: The traditional use of a beaker is to hold liquids. They are usually used in a scientific setting. Being glass, they can reach higher temperatures than plastic, so they are preferable in many science experiments. 4. Funnel: It is used to channel liquid or fine-grained substances into containers with a small opening. Without a funnel, spillage would occur. 5. Mortars and pestles were traditionally used in pharmacies to crush various ingredients prior to preparing a prescription. 6. A volumetric flask is a type of glassware utilized in laboratories for accurately measuring volumes of liquids. 1 7. Filter paper is a semi-permeable paper barrier placed perpendicular to a liquid or air flow.