Pharmaceutical Compounding and Dispensing Sample Chapter
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Camphor Revisited: Focus on Toxicity
Camphor Revisited: Focus on Toxicity Committee on Drugs This commentary updates a previous AAP state- TABLE. List of Camphor-Containing Products ment developed by the Committee on Drugs con- Product % of Camphor cerning camphor.1 The original commentary re- Absorbine Arthritic Pain Lotion 10 flected the level of concern among pediatric Act-On Rub Lotion 1.5 practitioners and poison centers about the toxicity of Anabaim Lotion 3 camphor. Since the original statement, the Food and Aveeno Anti-Itch Conc. Lotion 0.3 t Drug Administration (FDA) has recognized camphor Avalgesic Banaig Muscle Pain Reliever 2 as a safe and effective topical antitussive, analgesic, Bangesic t anesthetic, and antipruritic agent.2 Following the ap- Ben Gay Children’s Vaporizing Rub 5 proval process in 1983, the FDA required that the Betuline Lotion t concentration of camphor in products not exceed Campho-phemque First Aid Gel 10.8 Campho-phenique Uquid 10.85 11%.2 Fligher concentrations were not more effective Campho-phemque Powder 4.375 and could cause more serious adverse reactions if Counterpain Rub t accidentally ingested. Most reported camphor-re- Deep Down Rub 0.5 lated fatalities involved agents containing a concen- Dencorub Cream Dermal Rub t tration greater than 11%. Dermolin Liniment t Ingestion of potentially toxic substances by chil- Emul-O-Balm 1.1 dren is related to the availabffity of a product in their Heet Lotion 3 3.6 environment. Camphor remains widely available Heat Spray Minit-Rub 3.5 (Table). The toxicity of camphor when inappropri- Mollifene Ear Drops t ately used is well documented.6 Ingestion is the Musterole Regular 4 most common route of potentially toxic exposure, Panalgesic 3 with rapid onset of toxic effects. -

Absorbine Veterinary Liniment for Horses
Doc# 03.287 Ver. 11 SAFETY DATA SHEET ABSORBINE® VETERINARY LINIMENT SECTION 1 - PRODUCT AND COMPANY IDENTIFICATION 1.1 Trade Name (as labeled): Absorbine® Veterinary Liniment Synonyms: N/A CAS No: Mixture 1.2 Product Use: Soothes sore muscles and stiff joints 1.3 Company Name: W.F. Young Company Address: 302 Benton Dr Company Address Cont: East Longmeadow, MA 01028 Business Phone: ( 413) 526-9999 Website: www.wfyoung.com 1.4 Emergency Telephone Number: (413) 526-9999 Date of Current Revision: January 17, 2017 Date of Last Revision: August 7, 2015 SECTION 2 - HAZARD IDENTIFICATION EMERGENCY OVERVIEW: This product is a green thin liquid with an acetone odor. Health Hazards: May cause skin, eye, and respiratory system irritation. Flammabilit Hazards: This product is a flammable liquid with a flash point over 20°F (-6. 7°C). Reactivit Hazards: None. Environmental Hazards: The environmental effectsof this product have not been investigated, however release may cause long term adverse environmental effects. US DOT Symbols: EU and GHS Symbols: Signal Word: Danger! 2.1 CLASSIFICATION OF SUBSTANCE OR MIXTURE IN ACCORDANCE WITH 29 CFR 1200 (OSHA HCSl AND THE EUROPEAN UNION DIRECTIVES: This product does meet the definition of a hazardous substance or preparation as defined by 29 CFR 1910. 1200 or the European Union Council Directives 67 /548/EEC, 1999/45/EC, 1272/2008/EC and subsequent Directives. EU HAZARD CLASSIFICATIONOF INGREDIENTS PER DIRECTIVE 1272/2008/EC: IndexNumber: EC# 201-939-0 This substance is not classified in the AnnexVI of Directive 67/548/EEC EC# 200-662-2 This substance is classified in the AnnexVI of Directive 67/548/EEC Index# 606-001-00-8 Substances not listed either individually or in group entries must be self classified. -

Veterinary Dairy Spray Liniment by Dan Leiterman
1-888-376-6777 www.crystalcreeknatural.com December 2011 Introducing - Veterinary Dairy Spray Liniment By Dan Leiterman Crystal Creek is pleased to announce the addition of the new Veterinary Dairy Spray Liniment Features: Veterinary Dairy Spray Liniment • Available In A 24 oz. Spray Bottle Or A One Gallon (128 oz.) Refill Jug (VDSL) to our family of liniments (Veterinary Dairy Liniment and • A High Performance – Strong Relief Formula: Lini-Rub). Veterinary Dairy Spray Liniment provides the same ‘Contrast Therapy’ Warming and Cooling excellent performance as the original Analgesic Pain Relief rub-on Veterinary Dairy Liniment, only now with the convenience of a Anti-Inflammatory spray-on application. Anti-Microbial Skin Support – an aloe vera based formula Veterinary Dairy Spray Liniment is a powerful analgesic that combines • New Color For Lingering Identification Of Sprayed Animals the proven benefits of both warming and cooling ‘contrast therapy’ for • Meets National Organic Program Standards – challenged muscle tissue and edema Consider For Organic Use relief. The deep penetrating warmth soothes and supports proper • Economical To Use: circulation, while the lingering Retail Price coolness helps to reduce edema and inflammation of muscle tissue. 24 oz. Spray Bottle $29.95 / bottle If you prefer a spray-on liniment, Case Price (6 bottles/case) try Veterinary Dairy Spray Liniment and see the difference – it is stronger $28.95 / bottle and is better priced than the One Gallon Jug competition. If you prefer rub-on $134.00 / gallon liniments, try the Veterinary Dairy Case Price (4 gallons/case) Liniment (a white cream based $128.00 / gallon liniment) or the Crystal Creek Lini- Rub (an oil based liniment) and experience their excellent performance. -

The Effect of Calcium Carbonate and Sodium Bicarbonate on the Toxicity of Gossypol»
THE EFFECT OF CALCIUM CARBONATE AND SODIUM BICARBONATE ON THE TOXICITY OF GOSSYPOL» By WILLIS D. GALLUP, assistant chemist, and RUTH REDER, associate chemist, Department of Agricultural Chemistry Research, Oklahoma Agricultural Experi- ment Station INTRODUCTION In a previous study of the influence of certain dietary constituents on the response of rats to gossypol ingestion {2) ^ the authors showed that the toxicity of diets containing known amounts of gossypol was materially reduced when the diets were made basic by the addition of calcium carbonate and sodium bicarbonate. When the diets were made acidic by the addition of calcium chloride, only indirect evidence of a slight decrease in toxicity was obtained. Decreased toxicity was observed also when the protein content of the diet was increased from 13 percent to 35 percent. The conclusion was drawn that diets of high protein content and basic diets of high calcium content are favorable to the detoxication of gossypol. Considerable importance is attached to the results since calcium and protein are variable ingredients in diets used for the bio-assay of gossypol. The importance of these constituents in feeding cottonseed products to livestock has not been fully determined, although the value of supplementary protein in cottonseed-meal rations for pigs has recently been pointed out by Robison (5). In view of the favorable results obtained with sodium bicarbonate and calcium carbonate, it was deemed desirable to determine the pro- portion of these salts which would offer the greatest degree of pro- tection against gossypol injury and to determine the value of each salt in the presence of moderate amounts of thç other, as the principal elements of both are requisite for a normal nutritive condition. -
Experimental Study on Capture of Carbon Dioxide and Production of Sodium Bicarbonate from Sodium Hydroxide
Environ. Eng. Res. 2016; 21(3): 297-303 pISSN 1226-1025 http://dx.doi.org/10.4491/eer.2016.042 eISSN 2005-968X Experimental study on capture of carbon dioxide and production of sodium bicarbonate from sodium hydroxide Jae-Goo Shim†, Dong Woog Lee, Ji Hyun Lee, No-Sang Kwak KEPCO Research Institute, 105 Munji-ro, Yuseong-gu, Daejeon, 54056, Korea ABSTRACT Global warming due to greenhouse gases is an issue of great concern today. Fossil fuel power plants, especially coal-fired thermal power plants, are a major source of carbon dioxide emission. In this work, carbon capture and utilization using sodium hydroxide was studied experimentally. Application for flue gas of a coal-fired power plant is considered. Carbon dioxide, reacting with an aqueous solution of sodium hydroxide, could be converted to sodium bicarbonate (NaHCO3). A bench-scale unit of a reactor system was designed for this experiment. The capture scale of the reactor system was 2 kg of carbon dioxide per day. The detailed operational condition could be determined. The purity of produced sodium bicarbonate was above 97% and the absorption rate of CO2 was above 95% through the experiment using this reactor system. The results obtained in this experiment contain useful information for the construction and operation of a commercial-scale plant. Through this experiment, the possibility of carbon capture for coal power plants using sodium hydroxide could be confirmed. Keywords: Carbon Capture, Carbon Utilization, Sodium Bicarbonate 1. Introduction the post-combustion amine process [8-11]. The amine process is has been a proven method for a relatively long time, and it is close to commercialization. -

OHAUS New Scout Balance Range
Catalogue OHAUS new Scout Balance Range Touchscreen Page 121 Memmert Ovens & Incubators New bollé German Made Page 140 Rush Plus Small Has Arrived Page 77 Schott-DURAN Youtility Bottles A New Age Page 6 SAVINGS Up to 70% off major brands Bacto Laboratories Feb 2018 BactoIssue Laboratories 7.5 Pty Ltd - Phone (02) 9823-9000Proudly - Email [email protected] Supplying - (prices Science excl GST) Since 1966 1 Contents A Centrifuge 145 Flask, Volumetric Glass 17 Alcohol Wipes 55 Centrifuge Tube, Glass 24 Flask, Volumetric Plastic 29 Analytical Balance 117 Centrifuge Tube, Plastic 44 Forceps 88 Aspirator Bottle, Plastic 42 Chemicals 67 Forceps, Artery 92 Autoclave Indicators 59 Clamps, Bosshead 96 Fridge Thermometers 102 Autoclave Tape 59 Clamps, Burettes 97 Funnel, Glass 15 Autoclave Waste Bags 61 Clamps, Retort 96 Funnel, Plastic 30 Clinical Centrifuge 145 G - H B Coats, Laboratory 74 Gloves, Examination 72 Bacticinerator 82 Cold Bricks 69 Gloves, Safety 71 Bags, Waste 61 Colony Counter 81 Gowns 75 Balance, Moisture 119 Conductivity Meter 109 Hand Wash, Alcohol 55 Balances 116 Conical Measure, Plastic 27 Hand Wash, Cleanser 56 Batteries 102 Contaminated Waste Bags 62 Hand Wash, Sanitiser 55 Beaker, Glass 11 Coplin Jar 53 Hockey Stick 50 Beaker, Plastic 27 Corrosive Cabinets 85 Hotplate 124 Bench Roll 58 Cover Slips, Glass 52 Hotplate Stirrer 124 Biju McCartney Bottle 25 Cryo Vial, Plastic 37 Hygrometers 102 Bins, Broken Glass 61 Culture Media 50 I Bins, Chemotherapy 65 Culture Tube, Glass 24 Incubator 138 Bins, Contaminated Waste 61 Cuvettes, -

TOXICOLOGY and EXPOSURE GUIDELINES ______(For Assistance, Please Contact EHS at (402) 472-4925, Or Visit Our Web Site At
(Revised 1/03) TOXICOLOGY AND EXPOSURE GUIDELINES ______________________________________________________________________ (For assistance, please contact EHS at (402) 472-4925, or visit our web site at http://ehs.unl.edu/) "All substances are poisons; there is none which is not a poison. The right dose differentiates a poison and a remedy." This early observation concerning the toxicity of chemicals was made by Paracelsus (1493- 1541). The classic connotation of toxicology was "the science of poisons." Since that time, the science has expanded to encompass several disciplines. Toxicology is the study of the interaction between chemical agents and biological systems. While the subject of toxicology is quite complex, it is necessary to understand the basic concepts in order to make logical decisions concerning the protection of personnel from toxic injuries. Toxicity can be defined as the relative ability of a substance to cause adverse effects in living organisms. This "relative ability is dependent upon several conditions. As Paracelsus suggests, the quantity or the dose of the substance determines whether the effects of the chemical are toxic, nontoxic or beneficial. In addition to dose, other factors may also influence the toxicity of the compound such as the route of entry, duration and frequency of exposure, variations between different species (interspecies) and variations among members of the same species (intraspecies). To apply these principles to hazardous materials response, the routes by which chemicals enter the human body will be considered first. Knowledge of these routes will support the selection of personal protective equipment and the development of safety plans. The second section deals with dose-response relationships. -

Safety Data Sheet
First issue: September 17, 2009 Revision date: October 27, 2014 SDS No. 007.636 Version: 5 SAFETY DATA SHEET In accordance with OSHA’s Hazard Communication Standard 29 CFR §1910.1200 SECTION 1: IDENTIFICATION OF THE SUBSTANCE/MIXTURE AND OF THE COMPANY/UNDERTAKING 1.1. Product identifier: Absorbine® Veterinary Liniment Gel 1.2. Relevant identified uses of the substance or mixture and uses advised against Topical Analgesic 1.3. Details of the supplier of the safety data sheet Manufacturer/Supplier: W. F. Young, Inc. 302 Benton Drive East Longmeadow, MA 01028 Telephone number for information: 413 526 9999 E-mail: [email protected] 1.4. Emergency telephone number 413 526 9999 SECTION 2: HAZARDS IDENTIFICATION 2.1. Classification of the mixture F, Xn, Xi R10, 22, 43 2.2. Label elements Flammable Keep out of the reach of children Harmful if swallowed May product an allergic reaction 2.3. Other hazards Inhalation of vapors can cause anesthetic effect. Page 1 of 8 First issue: September 17, 2009 Revision date: October 27, 2014 SDS No. 007.636 Version: 5 SECTION 3: COMPOSITION/INFORMATION ON INGREDIENTS 3.2. Mixtures Hazardous ingredients information Component CAS Nr. EINECS / Amount DSD DSD ELINCS (%) Hazard R-Phrases Symbol Ethanola,denatured 64-17-5 200-578-6 40 - 70 F R11 Menthol 89-78-1 201-939-0 4 Choroxylenol 88-04-0 201-793-8 0.5 Xi R43 Spearmint Oil 8008-79-5 Not classified 0.5-1.0 Xi R43 Propylene Glycola 57-55-6 200-338-0 1 - 5 Other Components: Remaining components of this alcoholic mixture are proprietary, non-hazardous and/or are present at concentrations below reportable limits. -

Laboratory Manual
International Program UAM-Boston University Laboratory Manual Organic Chemistry I 2013-2014 Departamento de Química Orgánica Ernesto Brunet Romero Ana María Martín Castro Ramón Gómez Arrayás Laboratory Manual Table of Contents ............................................................................... 1 Introduction ............................................................................... 2 Prelab preparation ............................................................................... 2 Notebook ............................................................................. 3 Safety .............................................................................. 3 Laboratory Practices and Safety Rules ............................................................. 4 Accidents and injuries ........................................................................... 5 Fires ............................................................................. 5 Chemical Wastes ............................................................................. 6 Cleaning Responsibilities ............................................................................. 6 Lab cleanliness ............................................................................. 6 Laboratory Equipment ............................................................................. 7 Proper use of glassware ............................................................................. 8 Some techniques in lab experiments Heating, cooling and stirring ............................................................................ -

Biopharmaceutical Properties of Patches Relevant for Transdermal Drug Absorption – Confounding Factors and In‐Vitro Testing
Biopharmaceutical Properties of Patches 16.06.2015 Relevant for Transdermal Drug Absorption Biopharmaceutical Properties of Patches Relevant for Transdermal Drug Absorption – Confounding Factors and In‐Vitro Testing Johannes Bartholomäus Pharmakreativ Consulting, Aachen Skin as Barrier to Transdermal Absorption And that’s from what Mother Nature did not design all the difficulties in transdermal drug skin as an absorption site. delivery arise. It‘s much more the opposite! Stratum corneum as lipophilic barrier June 16, 2015 J. Bartholomäus: Biopharmaceutical Properties of Patches 2 © Johannes Bartholomäus 1 Biopharmaceutical Properties of Patches 16.06.2015 Relevant for Transdermal Drug Absorption Definition TDDS by Guidelines . Transdermal drug delivery systems . Transdermal patch:** Flexible single‐ (TDDS):* A TDDS or transdermal dose preparation intended to be patch is a flexible pharmaceutical applied to the unbroken skin to preparation of varying size containing obtain a systemic delivery over an one or more active substance(s) to be extended period of time. applied on the intact skin for systemic . Transdermal patches consist of a availability. backing sheet supporting a reservoir . There are two main types of or a matrix containing the active transdermal patch systems substance(s) and on the top a depending on how the drug pressure‐sensitive adhesive, which substance is dispersed in other patch assures the adhesion of the components: preparation to the skin. – Matrix systems with drug release based on . The backing sheet is impermeable to the diffusion of drug substance. the active substance(s) and normally – Reservoir systems containing a specific liquid drug compartment and release is impermeable to water. controlled by a membrane. -

Pulmonary Delivery of Biological Drugs
pharmaceutics Review Pulmonary Delivery of Biological Drugs Wanling Liang 1,*, Harry W. Pan 1 , Driton Vllasaliu 2 and Jenny K. W. Lam 1 1 Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, 21 Sassoon Road, Pokfulam, Hong Kong, China; [email protected] (H.W.P.); [email protected] (J.K.W.L.) 2 School of Cancer and Pharmaceutical Sciences, King’s College London, 150 Stamford Street, London SE1 9NH, UK; [email protected] * Correspondence: [email protected]; Tel.: +852-3917-9024 Received: 15 September 2020; Accepted: 20 October 2020; Published: 26 October 2020 Abstract: In the last decade, biological drugs have rapidly proliferated and have now become an important therapeutic modality. This is because of their high potency, high specificity and desirable safety profile. The majority of biological drugs are peptide- and protein-based therapeutics with poor oral bioavailability. They are normally administered by parenteral injection (with a very few exceptions). Pulmonary delivery is an attractive non-invasive alternative route of administration for local and systemic delivery of biologics with immense potential to treat various diseases, including diabetes, cystic fibrosis, respiratory viral infection and asthma, etc. The massive surface area and extensive vascularisation in the lungs enable rapid absorption and fast onset of action. Despite the benefits of pulmonary delivery, development of inhalable biological drug is a challenging task. There are various anatomical, physiological and immunological barriers that affect the therapeutic efficacy of inhaled formulations. This review assesses the characteristics of biological drugs and the barriers to pulmonary drug delivery. -
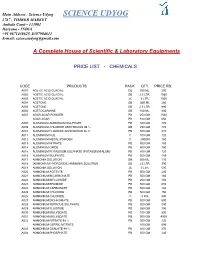
Science Udyog SCIENCE UDYOG 2767 , TIMBER MARKET Ambala Cantt - 133001 Haryana - INDIA +91 9671438625 ,8397904611 E-Mail: [email protected]
Main Address : Science Udyog SCIENCE UDYOG 2767 , TIMBER MARKET Ambala Cantt - 133001 Haryana - INDIA +91 9671438625 ,8397904611 E-mail: [email protected] A Complete House of Scientific & Laboratory Equipments PRICE LIST - CHEMICALS CODE PRODUCTS PACK QTY. PRICE RS. A001 ACETIC ACID GLACIAL GB 500 ML. 200 A002 ACETIC ACID GLACIAL GB 2.5 LTR. 1080 A003 ACETIC ACID GLACIAL JC 5 LTR. 1500 A004 ACETONE GB 500 ML 260 A005 ACETONE GB 2.5 LTR. 990 A006 ACETOCARMINE GB 100 ML. 800 A007 AGAR AGAR POWDER PB 250 GM 1500 AGAR AGAR PB 100 GM 650 A008 ALUMINIUM AMMONIUM SULPHATE PB 500 GM 170 A009 ALUMINIUM CHLORIDE ANHYDROUS 98 % GB 250 GM 170 A010 ALUMINIUM FLUORIDE ANHYDROUS 96 % PB 500 GM 410 A011 ALUMINIUM FOIL C 100 GM 120 A012 ALUMINIUM METAL POWDER C 250GM 180 A013 ALUMINIUM NITRATE PB 500 GM 180 A014 ALUMINIUM OXIDE PB 500 GM 150 A015 ALUMINIUM POTASSIUM SULPHATE (POTASSIUM ALUM) PB 500 GM 120 A016 ALUMINIUM SULPHATE PB 500 GM 148 A017 AMMONIA SOLUTION GB 500 ML. 110 A018 (AMMONIUM HYDROXIDE) AMMONIA SOLUTION GB 2.5 LTR. 390 A019 AMMONIA SOLUTION JC 5 LTR. 590 A020 AMMONIUM ACETATE PB 500 GM 240 A021 AMMONIUM BICARBONATE PB 500 GM 180 A022 AMMONIUM BIFLUORIDE PB 250 GM 156 A023 AMMONIUM BROMIDE PB 500 GM 680 A024 AMMONIUM CARBONATE PB 500 GM 194 A025 AMMONIUM CHLORIDE PB 500 GM 150 A026 AMMONIUM CHLORIDE C 5 KG. 990 A027 AMMONIUM DICHROMATE PB 500 GM 690 A028 AMMONIUM FERROUS SULPHATE PB 500 GM 240 A029 AMMONIUM FLUORIDE PB 250 GM 196 A030 AMMONIUM MOLYBDATE PB 100 GM 890 A031 AMMONIUM MOLYBDATE PB 500 GM 4500 A032 AMMONIUM NITRATE 98 % PB 500 GM 136 AMMONIUM CERRIC NITRATE 100 GM 595 A033 AMMONIUM OXALATE 99 % PB 500 GM 270 A034 AMMONIUM PHOSPHATE PB 500 GM 240 A035 AMMONIUM SULPHATE PB 500GM 142 A036 AMYL ACETATE ISO GB 500 ML.