Murder by Poison in Scotland During the Nineteenth and Early Twentieth Centuries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Poison Prevention Packaging: a Guide for Healthcare Professionals
PPooiissoonn PPrreevveennttiioonn PPaacckkaaggiinngg:: AA GGuuiiddee FFoorr HHeeaalltthhccaarree PPrrooffeessssiioonnaallss REVISED 2005 CPSC 384 US. CONSUMER PRODUCT SAFETY COMMISSION, WASHINGTON, D.C. 20207 THIS BROCHURE BROUGHT TO YOU BY: U.S. CONSUMER PRODUCT SAFETY COMMISSION Washington, DC 20207 Web site: www.cpsc.gov Toll-free hotline: 1-800-638-2772 The U.S. Consumer Product Safety Commission (CPSC) is a federal agency that helps keep families and children safe in and around their homes. For more information, call the CPSC’s toll-free hotline at 1-800-638-2772 or visit its website at http://www.cpsc.gov. Poison Prevention Packaging: A Guide For Healthcare Professionals (revised 2005) Preface The U.S. Consumer Product Safety Commission (CPSC) administers the Poison Prevention Packaging Act of 1970 (PPPA), 15 U.S.C. §§ 1471-1476. The PPPA requires special (child-resistant and adult-friendly) packaging of a wide range of hazardous household products including most oral prescription drugs. Healthcare professionals are more directly involved with the regulations dealing with drug products than household chemical products. Over the years that the regulations have been in effect, there have been remarkable declines in reported deaths from ingestions by children of toxic household substances including medications. Despite this reduction in deaths, many children are poisoned or have "near-misses" with medicines and household chemicals each year. Annually, there are about 30 deaths of children under 5 years of age who are unintentionally poisoned. Data from the National Electronic Injury Surveillance System (a CPSC database of emergency room visits) indicate that in 2003, an estimated 78,000 children under 5 years of age were treated for poisonings in hospital emergency rooms in the United States. -
Approach to the Poisoned Patient
PED-1407 Chocolate to Crystal Methamphetamine to the Cinnamon Challenge - Emergency Approach to the Intoxicated Child BLS 08 / ALS 75 / 1.5 CEU Target Audience: All Pediatric and adolescent ingestions are common reasons for 911 dispatches and emergency department visits. With greater availability of medications and drugs, healthcare professionals need to stay sharp on current trends in medical toxicology. This lecture examines mind altering substances, initial prehospital approach to toxicology and stabilization for transport, poison control center resources, and ultimate emergency department and intensive care management. Pediatric Toxicology Dr. James Burhop Pediatric Emergency Medicine Children’s Hospital of the Kings Daughters Objectives • Epidemiology • History of Poisoning • Review initial assessment of the child with a possible ingestion • General management principles for toxic exposures • Case Based (12 common pediatric cases) • Emerging drugs of abuse • Cathinones, Synthetics, Salvia, Maxy/MCAT, 25I, Kratom Epidemiology • 55 Poison Centers serving 295 million people • 2.3 million exposures in 2011 – 39% are children younger than 3 years – 52% in children younger than 6 years • 1-800-222-1222 2011 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System Introduction • 95% decline in the number of pediatric poisoning deaths since 1960 – child resistant packaging – heightened parental awareness – more sophisticated interventions – poison control centers Epidemiology • Unintentional (1-2 -

Signs and Symptoms of Pesticide Poisoning
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Historical Materials from University of Nebraska-Lincoln Extension Extension 1997 EC97-2505 Signs and Symptoms of Pesticide Poisoning Larry D. Schulze University of Nebraska - Lincoln, [email protected] Clyde Ogg University of Nebraska - Lincoln, [email protected] Edward F. Vitzthum University of Nebraska - Lincoln, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/extensionhist Part of the Agriculture Commons, and the Curriculum and Instruction Commons Schulze, Larry D.; Ogg, Clyde; and Vitzthum, Edward F., "EC97-2505 Signs and Symptoms of Pesticide Poisoning" (1997). Historical Materials from University of Nebraska-Lincoln Extension. 1225. https://digitalcommons.unl.edu/extensionhist/1225 This Article is brought to you for free and open access by the Extension at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Historical Materials from University of Nebraska-Lincoln Extension by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. University of Nebraska Cooperative Extension EC97-2505-A Signs and Symptoms of Pesticide Poisoning Larry D. Schulze, Extension Pesticide Coordinator Clyde L. Ogg, Extension Assistant, Pesticide Training Edward F. Vitzthum, Coordinator, Environmental Programs z Manage Your Risk z Signal Words z Read the pesticide Label z Routes of Exposure z Pesticide Toxicity z Recognizing Signs and Symptoms of Poisoning z Recognizing Common pesticide Poisonings { Organophosphate and Carbamate Insecticides { Organochlorine Insecticides { Synthetic Pyrethroid Insecticides { Plant-derived Insecticides { Inorganic Insecticides { Microbial Insecticides { DEET Repellent { Bipyridyl Herbicides { Chlorophenoxy Herbicides { Arsenical Herbicides { Wood Preservatives { Fumigants { Rodenticides { Fungicides z What To Do When Pesticide Poisoning Occurs z References z Pesticide Safety Telephone Numbers Accidental exposure or overexposure to pesticides can have serious implications. -

Strychnine Poisoning
0++- Poison HOTLINE Partnership between UnityPoint Health and University of Iowa Hospitals and Clinics November 2013 Strychnine Poisoning Strychnine is a chemical naturally found in the seeds of the tree Strychnos nux- vomica. It is mainly used as a pesticide to control rats, moles, gophers, and coyotes. Commercial baits are pelleted and often dyed red or green. Strychnine has on rare occasions been found to be mixed with street drugs such as LSD, heroin, and cocaine. Strychnine is a white, odorless, bitter tasting crystalline powder that can be taken by mouth, inhaled or given intravenously. Strychnine is highly toxic and Did you know …… only a small amount is needed to produce severe health effects in people. As little as 30 mg may cause death in an adult. Vaporizing alcohol and “smoking” the vapors (inhaling Strychnine blocks the action of the neurotransmitter glycine which controls how is a more accurate term) is a nerve signals are sent to muscles. Glycine is an inhibitory neurotransmitter and new method for alcohol works like an “off switch” for muscles. When this “off switch” is not working consumption. The alcohol is because it is being blocked by strychnine, muscles throughout the body have poured into a vaporizing severe, painful spasms. While these spasms may look like the patient is having machine or over dry ice and a seizure, it is not a true seizure and there is no post-ictal phase. Repetitive inhaled. The alcohol enters muscle spasms caused by strychnine will lead to fever, muscle break down the lungs where it is rapidly (rhabdomyolysis), severe metabolic acidosis and respiratory failure. -

Toxicology in Antiquity
TOXICOLOGY IN ANTIQUITY Other published books in the History of Toxicology and Environmental Health series Wexler, History of Toxicology and Environmental Health: Toxicology in Antiquity, Volume I, May 2014, 978-0-12-800045-8 Wexler, History of Toxicology and Environmental Health: Toxicology in Antiquity, Volume II, September 2014, 978-0-12-801506-3 Wexler, Toxicology in the Middle Ages and Renaissance, March 2017, 978-0-12-809554-6 Bobst, History of Risk Assessment in Toxicology, October 2017, 978-0-12-809532-4 Balls, et al., The History of Alternative Test Methods in Toxicology, October 2018, 978-0-12-813697-3 TOXICOLOGY IN ANTIQUITY SECOND EDITION Edited by PHILIP WEXLER Retired, National Library of Medicine’s (NLM) Toxicology and Environmental Health Information Program, Bethesda, MD, USA Academic Press is an imprint of Elsevier 125 London Wall, London EC2Y 5AS, United Kingdom 525 B Street, Suite 1650, San Diego, CA 92101, United States 50 Hampshire Street, 5th Floor, Cambridge, MA 02139, United States The Boulevard, Langford Lane, Kidlington, Oxford OX5 1GB, United Kingdom Copyright r 2019 Elsevier Inc. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Details on how to seek permission, further information about the Publisher’s permissions policies and our arrangements with organizations such as the Copyright Clearance Center and the Copyright Licensing Agency, can be found at our website: www.elsevier.com/permissions. This book and the individual contributions contained in it are protected under copyright by the Publisher (other than as may be noted herein). -

Dermal Exposure to Strychnine
Journal of Analytical Toxicology, Vol. 25, July/August 2001 [CaseReport Dermal Exposureto Strychnine Richard Greene 1 and Robert MeatheralP,* 1Emergency Department, Grace General Hospital and 2Laboratory Medicine, St. Boniface General Hospital, Winnipeg, Manitoba, Canada Downloaded from https://academic.oup.com/jat/article/25/5/344/778260 by guest on 24 September 2021 t Abstract ] tents into the toilet. She accidently spilled about 1 cupful on the floor, which she wiped up with a cloth soaked in a diluted Javex A non-fatal case of strychnine poisoning through dermal exposure is solution (sodium hypochlorite). Her dermal exposure was limited described. About 24 b after cleaning up a strychnine spill, a 50-year- to her left palm; she washed her hands about 30 rain after old woman presented to the emergency department with classical cleaning up the spill. During the prodromal time period, she signs of strychnine poisoning, consisting of marked pain in the experienced no irritation or dermatitis to the left hand. Except for muscles of her lower limbs, dermal sensitivity, and stiffness in her a tingling sensation in her left hand, she was asymptomatic until jaw. Her treatment was intravenous fluid replacement and about 22:00 h when her arms and legs began to shake, pro- alkalinization in anticipation of potential renal failure due to gressing to spasms. Over the course of the night, the frequency rhabdomyolysis. Her plasma creatine kinase was elevated to 677 and duration of these muscle contractions increased. By U/L with no rise in the heart specific MB fraction. Serum myoglobin morning, the pain was more severe in the muscles of her lower level obtained retrospectively was 195 pg/L. -

Question of the Day Archives: Monday, December 5, 2016 Question: Calcium Oxalate Is a Widespread Toxin Found in Many Species of Plants
Question Of the Day Archives: Monday, December 5, 2016 Question: Calcium oxalate is a widespread toxin found in many species of plants. What is the needle shaped crystal containing calcium oxalate called and what is the compilation of these structures known as? Answer: The needle shaped plant-based crystals containing calcium oxalate are known as raphides. A compilation of raphides forms the structure known as an idioblast. (Lim CS et al. Atlas of select poisonous plants and mushrooms. 2016 Disease-a-Month 62(3):37-66) Friday, December 2, 2016 Question: Which oral chelating agent has been reported to cause transient increases in plasma ALT activity in some patients as well as rare instances of mucocutaneous skin reactions? Answer: Orally administered dimercaptosuccinic acid (DMSA) has been reported to cause transient increases in ALT activity as well as rare instances of mucocutaneous skin reactions. (Bradberry S et al. Use of oral dimercaptosuccinic acid (succimer) in adult patients with inorganic lead poisoning. 2009 Q J Med 102:721-732) Thursday, December 1, 2016 Question: What is Clioquinol and why was it withdrawn from the market during the 1970s? Answer: According to the cited reference, “Between the 1950s and 1970s Clioquinol was used to treat and prevent intestinal parasitic disease [intestinal amebiasis].” “In the early 1970s Clioquinol was withdrawn from the market as an oral agent due to an association with sub-acute myelo-optic neuropathy (SMON) in Japanese patients. SMON is a syndrome that involves sensory and motor disturbances in the lower limbs as well as visual changes that are due to symmetrical demyelination of the lateral and posterior funiculi of the spinal cord, optic nerve, and peripheral nerves. -

Survival After Deliberate Strychnine Self-Poisoning, with Toxicokinetic Data
University of Wollongong Research Online Faculty of Science, Medicine and Health - Papers: part A Faculty of Science, Medicine and Health 2002 Case report: Survival after deliberate strychnine self-poisoning, with toxicokinetic data David Michael Wood Guy’s and St. Thomas’ Hospital Emma Webster Royal Oldham Hospital Daniel Martinez Guy’s and St. Thomas’ Hospital Paul Ivor Dargan Guy’s and St. Thomas’ Hospital Alison L. Jones University of Wollongong, [email protected] Follow this and additional works at: https://ro.uow.edu.au/smhpapers Part of the Medicine and Health Sciences Commons, and the Social and Behavioral Sciences Commons Recommended Citation Wood, David Michael; Webster, Emma; Martinez, Daniel; Dargan, Paul Ivor; and Jones, Alison L., "Case report: Survival after deliberate strychnine self-poisoning, with toxicokinetic data" (2002). Faculty of Science, Medicine and Health - Papers: part A. 1903. https://ro.uow.edu.au/smhpapers/1903 Research Online is the open access institutional repository for the University of Wollongong. For further information contact the UOW Library: [email protected] Case report: Survival after deliberate strychnine self-poisoning, with toxicokinetic data Abstract Introduction Strychnine poisoning is uncommon, and in most severe cases, the patient dies before reaching hospital. The management of strychnine poisoning is well documented, although there are few data on the kinetics of elimination of strychnine after overdose. Case report A 42-year-old man presented shortly after ingestion of an unknown quantity of strychnine powder. After a respiratory arrest, with intensive supportive management requiring admission to an intensive care unit, he survived. Eight serum samples were taken over the first 5 days and analysed subsequently for strychnine concentrations. -
Ingested Lethal Ageni's Strychnine
REVIEW OF CURRENT VERTEBRATE PESTICIDES D. Glen Crabtree Bureau of Sport Fisheries and Wildlife, Wildlife Research Center, B1dg. 45, Denver Federal Center, Denver 25, Colorado. For the purpose of this brief review, EmG>hasis will be placed on development, physical properties, physiological action, experience and limitations of vertebrate pesticides primarily of current opera- tional 1.m;portance in the control of field rodents and predatory animals. INGESTED LETHAL AGENI'S STRYCHNINE (C21H~202) 'Dlis al.kaloid was discovered by Pelletier and Cavento,}/in 1817 as a constituent in the seeds of Strychnos Nux-vomica or Strychnos !gnatii, which were used :for killing dogs, cats and birds in Europe at least as early as J.6ljo • Strychnine (probably the sulfate) appears to have been introduced as a pesticide in the United States about 1847 and became the g/ principal tool of the professional "wolfer" during the years 1800-1885. PHYSICAL PROPERTIES: ~e alkaJ.oid of commerce is a white or greyish white powder prepared from seeds grown in Southern Asia. It is quite stable, almost insoluble in water, but soluble in many organic solvents and to varying degrees in dilute acids With which it forms salts having limited solubility in water. Strychnine and its salts have an exceedingly bitter taste and are not absorbed through the normal intact skin. 327 Both the alkaloid and strychnine sul.fate are widely used today as vertebrate pesticides. In the case of the latter, allowance must be made in preparing l.ethal baits since it contains onl.y 78.04~ strychnine. PHYSIOLOGICAL ACTION: Ingested strychnine is proJJG>tly absorbed, mainly, from the intestinal tract. -

The Elements of Murder a History of Poison John Emsley Oxford University Press
Book review The elements of murder A history of poison John Emsley Oxford University Press. New York, New York, USA. 2005. 421 pp. $30.00. ISBN: 0-19280-599-1 (hardcover). Reviewed by Donna Mendrick Gene Logic Inc., Gaithersburg, Maryland, USA. E-mail: [email protected] John Emsley has written an entertain- Yet there are some weaknesses in the book. lar statements that should have been cor- ing book entitled The elements of murder: a The introductory chapter lists an extensive rected in the editing process. For example, history of poison. He is a chemist who spent history of alchemists, and although this he concludes in the last sentence relating many years as a researcher and lecturer lends credibility to the author’s research, it to the British Empire that “lead cannot be at London University before becoming is dry reading, and the selected elements are blamed” for its rapid decline yet states that a popular science writer. This enjoyable profiled more extensively later in the book. “some future historian will conclude . book is devoted to the poisonous elements Not to worry, though. The reader becomes that lead was the reason.” found in the periodic table. His descrip- engrossed by the second chapter as it delves Even with these lapses, the book is enjoy- tion of the chemicals is encompassing into details on mercury. Another concern able. Included is a letter written in 1786 by and will interest chemists, physicians, and is the limited reference list and citations, Benjamin Franklin stating that the dan- knowledgeable readers of murder myster- which require the reader to rely on Ems- gers of lead have been known for at least ies. -

Poisoned Relations: Medicine, Sorcery, and Poison Trials in the Contested Atlantic, 1680-1850
POISONED RELATIONS: MEDICINE, SORCERY, AND POISON TRIALS IN THE CONTESTED ATLANTIC, 1680-1850 A Dissertation Submitted to the Faculty of the Graduate School of Arts and Sciences of Georgetown University in partial fulfillment of the requirements for the degree of Doctor of Philosophy in History By Chelsea L. Berry, B.A. Washington, DC March 25, 2019 Copyright 2019 by Chelsea L. Berry All Rights Reserved ii POISONED RELATIONS: MEDICINE, SORCERY, AND POISON TRIALS IN THE CONTESTED ATLANTIC, 1680-1850 Chelsea L. Berry, B.A. Thesis Advisor: Alison Games, Ph.D. ABSTRACT From 1680 to 1850, courts in the slave societies of the western Atlantic tried hundreds of free and enslaved people of African descent for poisoning others, often through sorcery. As events, poison accusations were active sites for the contestation of ideas about health, healing, and malevolent powers. Many of these cases centered on the activities of black medical practitioners. This thesis explores changes in ideas about poison through the wave of poison cases over this 170-year period and the many different people who made these changes and were bound up these cases. It analyzes over five hundred investigations and trials in Virginia, Bahia, Martinique, and the Dutch Guianas—each vastly different slave societies that varied widely in their conditions of enslaved labor, legal systems, and histories. It is these differences that make the shared patterns in the emergence, growth, and decline of poison cases, and of the relative importance of African medical practitioners within them, so intriguing. Across these four locations, there was a specific, temporally bounded, and widely shared relationship between poison, medicine, and sorcery in this period. -
Managing Pesticide Poisoning Risk and Understanding the Signs and Symptoms Clyde L
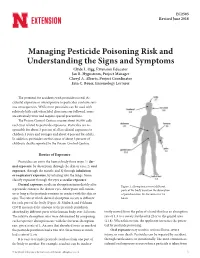
EC2505 Revised June 2018 Managing Pesticide Poisoning Risk and Understanding the Signs and Symptoms Clyde L. Ogg, Extension Educator Jan R. Hygnstrom, Project Manager Cheryl A. Alberts, Project Coordinator Erin C. Bauer, Entomology Lecturer The potential for accidents with pesticides is real. Ac- cidental exposure or overexposure to pesticides can have seri- ous consequences. While most pesticides can be used with relatively little risk when label directions are followed, some are extremely toxic and require special precautions. The Poison Control Centers receive about 90,000 calls each year related to pesticide exposures. Pesticides are re- sponsible for about 3 percent of all accidental exposures to children 5 years and younger and about 4 percent for adults. In addition, pesticides are the cause of about 3 percent of children’s deaths reported to the Poison Control Centers. Routes of Exposure Pesticides can enter the human body three ways: 1) der- mal exposure, by absorption through the skin or eyes; 2) oral exposure, through the mouth; and 3) through inhalation or respiratory exposure, by inhaling into the lungs. Some classify exposure through the eyes as ocular exposure. Dermal exposure results in absorption immediately after Figure 1. Absorption rates of different a pesticide contacts the skin or eyes. Absorption will contin- parts of the body based on the absorption ue as long as the pesticide remains in contact with the skin or of parathion into the forearm over 24 eyes. The rate at which dermal absorption occurs is different hours. for each part of the body (Figure 1). Maiback and Feldman (1974) measured the amount of the pesticide parathion absorbed by different parts of the human body over 24 hours.