Therapeutic Class Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Treatment Patterns, Persistence and Adherence Rates in Patients with Type 2 Diabetes Mellitus in Japan: a Claims- Based Cohort Study
Open access Research BMJ Open: first published as 10.1136/bmjopen-2018-025806 on 1 March 2019. Downloaded from Treatment patterns, persistence and adherence rates in patients with type 2 diabetes mellitus in Japan: a claims- based cohort study Rimei Nishimura,1 Haruka Kato,2 Koichi Kisanuki,2 Akinori Oh,2 Shinzo Hiroi,2 Yoshie Onishi,3 Florent Guelfucci,4 Yukio Shimasaki2 To cite: Nishimura R, Kato H, ABSTRACT Strengths and limitations of this study Kisanuki K, et al. Treatment Objective To determine real-world trends in antidiabetic patterns, persistence and drug use, and persistence and adherence, in Japanese ► This retrospective evaluation of administrative adherence rates in patients patients with type 2 diabetes mellitus (T2DM). with type 2 diabetes mellitus claims data (2011–2015) using the Japan Medical Design Retrospective evaluation of administrative claims in Japan: a claims-based Data Center (JMDC) and Medical Data Vision (MDV) data (2011–2015) using the Japan Medical Data Center cohort study. BMJ Open databases was conducted to determine real-world (JMDC) and Medical Data Vision (MDV) databases. 2019;9:e025806. doi:10.1136/ trends in antidiabetic drug use, and persistence and Setting Analysis of two administrative claims databases bmjopen-2018-025806 adherence, in Japanese patients with type 2 dia- for Japanese patients with T2DM. betes mellitus (T2DM); 40 908 and 90 421 patients ► Prepublication history and Participants Adults (aged ≥18 years) with an International additional material for this were included from the JMDC and MDV databases, Classification of Diseases, 10th Revision code of T2DM and paper are available online. To respectively. at least one antidiabetic drug prescription. -

Effect of Oral Hypoglycaemic Agents on Glucose Tolerance in Pancreatic Diabetes
Gut: first published as 10.1136/gut.13.4.285 on 1 April 1972. Downloaded from Gut, 1972, 13, 285-288 Effect of oral hypoglycaemic agents on glucose tolerance in pancreatic diabetes B. I. JOFFE, W. P. U. JACKSON, S. BANK, AND A. I. VINIK From the Department of Medicine, Witwatersrand University Medical School, Johannesburg, the Gastro- intestinal and Endocrine Research Units of Cape Town University Medical School, and the Chemical Pathology Department of Natal University, South Africa SUMMARY The short-term therapeutic effect of oral hypoglycaemic agents has been assessed in 12 patients with symptomatic diabetes secondary to chronic pancreatitis (pancreatic diabetes). In six patients who had moderate to severe carbohydrate intolerance, associated with severe insulino- paenia during arginine infusion, the potent sulphonylurea chlorpropamide produced no change in the fasting blood glucose level after two weeks of treatment. This contrasted with the significant reduction produced in a matched group of maturity-onset primary diabetics. The six patients with milder diabetes, and a greater (although still subnormal) insulin secretory capacity, showed an improvement in oral glucose tolerance during the first hour following glucose administration while on chlorpropamide. When the biguanide phenformin was substituted for chlorpropamide in five of these patients, a statistically insignificant improvement in glucose tolerance was observed during treatment. Applications of these findings to the practical management of pancreatic diabetes are briefly http://gut.bmj.com/ considered. Chronic pancreatitis is frequently complicated by and two women, ranging from 30 to 67 years of age. diabetes (pancreatic diabetes). Recent studies The diagnosis of pancreatitis was confirmed on the utilizing immunoassay procedures (Joffe, Bank, basis of a gross abnormality in at least two aspects of Jackson, Keller, O'Reilly, and Vinik, 1968; Anderson the pancreatic function test, namely, a low volume of on September 24, 2021 by guest. -
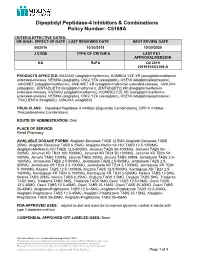
Dipeptidyl Peptidase-4 Inhibitors and Combinations
Dipeptidyl Peptidase-4 Inhibitors & Combinations Policy Number: C5169A CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DATE 06/2016 10/30/2019 10/30/2020 J CODE TYPE OF CRITERIA LAST P&T APPROVAL/VERSION NA RxPA Q4 2019 20191030C5169-A PRODUCTS AFFECTED: KAZANO (alogliptin/metformin), KOMBIGLYZE XR (saxagliptin/metformin extended-release), NESINA (alogliptin), ONGLYZA (saxagliptin), OSENI (alogliptin/pioglitazone), JANUMET (sitagliptin/metformin), JANUMET XR (sitagliptin/metformin extended-release), JANUVIA (sitagliptin), JENTADUETO (linagliptin/metformin), JENTADUETO XR (linagliptin/metformin extended-release), KAZANO (alogliptin/metformin), KOMBIGLYZE XR (saxagliptin/metformin extended-release), NESINA (alogliptin), ONGLYZA (saxagliptin), OSENI (alogliptin/pioglitazone) TRADJENTA (linagliptin), JANUVIA (sitagliptin) DRUG CLASS: Dipeptidyl Peptidase-4 Inhibitor-(Biguanide Combinations), DPP-4 Inhibitor- Thiazolidinedione Combinations ROUTE OF ADMINISTRATION: Oral PLACE OF SERVICE: Retail Pharmacy AVAILABLE DOSAGE FORMS: Alogliptin Benzoate TABS 12.5MG,Alogliptin Benzoate TABS 25MG, Alogliptin Benzoate TABS 6.25MG, Alogliptin-Metformin HCl TABS 12.5-1000MG Alogliptin-Metformin HCl TABS 12.5-500MG, Janumet TABS 50-1000MG, Janumet TABS 50- 500MG, Janumet XR TB24 100-1000MG, Janumet XR TB24 50-1000MG, Janumet XR TB24 50- 500MG, Januvia TABS 100MG, Januvia TABS 25MG, Januvia TABS 50MG, Jentadueto TABS 2.5- 1000MG, Jentadueto TABS 2.5-500MG, Jentadueto TABS 2.5-500MG, Jentadueto TABS 2.5- 850MG, Jentadueto -

Polyhexamethylene Biguanide Hydrochloride) As Used in Cosmetics
Safety Assessment of Polyaminopropyl Biguanide (polyhexamethylene biguanide hydrochloride) as Used in Cosmetics Status: Tentative Report for Public Comment Release Date: September 26, 2017 Panel Date: December 4-5, 2017 All interested persons are provided 60 days from the above date to comment on this safety assessment and to identify additional published data that should be included or provide unpublished data which can be made public and included. Information may be submitted without identifying the source or the trade name of the cosmetic product containing the ingredient. All unpublished data submitted to CIR will be discussed in open meetings, will be available at the CIR office for review by any interested party and may be cited in a peer-reviewed scientific journal. Please submit data, comments, or requests to the CIR Executive Director, Dr. Bart Heldreth. The 2017 Cosmetic Ingredient Review Expert Panel members are: Chair, Wilma F. Bergfeld, M.D., F.A.C.P.; Donald V. Belsito, M.D.; Ronald A. Hill, Ph.D.; Curtis D. Klaassen, Ph.D.; Daniel C. Liebler, Ph.D.; James G. Marks, Jr., M.D.; Ronald C. Shank, Ph.D.; Thomas J. Slaga, Ph.D.; and Paul W. Snyder, D.V.M., Ph.D. The CIR Executive Director is Bart Heldreth, Ph.D. This report was prepared by Wilbur Johnson, Jr., M.S., Senior Scientific Analyst and Ivan Boyer, Ph.D., former Senior Toxicologist. © Cosmetic Ingredient Review 1620 L STREET, NW, SUITE 1200 ◊ WASHINGTON, DC 20036-4702 ◊ PH 202.331.0651 ◊ FAX 202.331.0088 ◊ [email protected] ABSTRACT: The Cosmetic Ingredient Review (CIR) Expert Panel (Panel) reviewed the safety of Polyaminopropyl Biguanide (polyhexamethylene biguanide hydrochloride), which functions as a preservative in cosmetic products. -

A Review on Evolution in Triglyceride Determination
Available online at www.derpharmachemica.com ISSN 0975-413X Der Pharma Chemica, 2018, 10(5): 84-88 CODEN (USA): PCHHAX (http://www.derpharmachemica.com/archive.html) Sodium-glucose co-transporter 2 (SGLT2) Inhibitors: New Target for Type 2 Diabetes Mellitus (T2DM) Review Swapna Vadlamani* Asst. proffesor, NIPER, Hyderabad, Andhra Pradesh, India ABSTRACT Introduction: Knocking out type2 diabetes by new insulin independent renal glucose transporters as targets, reducing the side effects related to high rise in glucose levels is a more efficient way to manage diabetes. Sodium-glucose co-transporter 2 (SGLT2) inhibitors block reabsorption of glucose back into the blood and stimulate secretion in urine in a way controlling blood glucose levels. Areas discussed: We emphasize in this review an overview of type 2 diabetes. New insulin independent targets, SGLT family inhibitors and their mechanism of action are briefly discussed. Molecular modeling studies carried out for new analogues of SGLT2 were indicated and also about current marketed SGLT drugs their safety issues are briefly outlined. Conclusion: SGLT2 inhibitors are very promising drugs for near future, where insulin sensitization is a problem. A combination of drugs related to insulin dependent pathway and also independent pathway like SGLT2/SGLT1 drugs will be more effective in glycemic control with lesser side effects. Keywords: Type II Diabetes, SGLT2 inhibitors INTRODUCTION Present scenario of food habits and absolutely very less physical activity is becoming the major cause for obesity finally leading to diabetes. Diabetes is said to be a rich man disease and mostly occurs at the later age of 40, but now one in every 5 persons at early age diagnosed turned to be diabetic mainly because of lifestyle changes. -

Type 2 Diabetes Treatment Recommendations Update
abetes & Di M f e o t a l b a o Cornell, J Diabetes Metab 2014, 5:8 n l r i s u m o DOI: 10.4172/2155-6156.1000414 J Journal of Diabetes and Metabolism ISSN: 2155-6156 Review Article Open Access Type 2 Diabetes Treatment Recommendations Update: Appropriate Use of Dipeptidyl Peptidase-4 Inhibitors Susan Cornell* Midwestern University, Chicago College of Pharmacy, Downers Grove, IL, USA Abstract In this article, recommendations from the 2012 American Diabetes Association (ADA)/European Association for the Study of Diabetes (EASD) position statement are discussed with an emphasis on the appropriate use of Dipeptidyl Peptidase-4 (DPP-4) inhibitors in individuals with Type 2 Diabetes Mellitus (T2DM). The 2012 ADA/EASD position statement emphasizes individualization of treatment, with glycated hemoglobin (A1C) targets being determined for each patient based on life expectancy, complications, disease duration, comorbidities, such as cardiovascular disease or cognitive impairment, and the risk of hypoglycemia and other adverse events. Patients’ attitudes and support systems should also be considered. Recommendations for pharmacotherapy are less prescriptive and should be based on a patient’s needs, preferences, and tolerances. In general, metformin is recommended as first- line therapy for most patients, although combination of 2 noninsulin agents or insulin alone should be considered in patients with baseline A1C ≥ 9.0%. Add-on therapy to metformin will likely be needed to achieve and maintain glycemic control as the disease progresses. It is important to avoid therapies that increase the risk of weight gain or and, especially in older patients, hypoglycemia. As discussed in this review, DPP-4 inhibitors are well tolerated and effectively lower A1C and improve β-cell function without increasing the risk of hypoglycemia and weight gain. -

Glycemic Management of Type 2 Diabetes
Glycemic Management of Type 2 Diabetes Gail Nunlee-Bland, M.D. Professor Medicine & Pediatrics Director, Diabetes Treatment Center Howard University 1 Disclosures • None Learning Objectives • Understand the importance of lifestyle therapy in diabetes management • Know the classes of antihyperglycemic agents, mechanism of action, benefits and side effects of these agents • Recognize the importance of individualized treatment goals for diabetic patients AACE Comprehensive Care Plan Disease management from Antihyperglycemic a multidisciplinary team pharmacotherapy Comprehensive Care Plan Comprehensive diabetes Therapeutic lifestyle self-education for the change patient 4 Handelsman YH, et al. Endocr Pract. 2015;21(suppl 1):1-87. Glycemic Management of Type 2 Diabetes THERAPEUTIC LIFESTYLE CHANGE 5 Components of Therapeutic Lifestyle Change • Healthful eating • Sufficient physical activity • Sufficient sleep • Avoidance of tobacco products • Limited alcohol consumption • Stress reduction 6 Handelsman YH, et al. Endocr Pract. 2015;21(suppl 1):1-87. Glycemic Management of Type 2 Diabetes ANTIHYPERGLYCEMIC THERAPY 7 Cardiovascular Outcomes Trials: A Brief History • 2008 FDA guidance mandating assessment of CV safety of all antihyperglycemic agents in RCTs – Designed as noninferiority studies to demonstrate study drug was not associated with more MACE than placebo • Some study designs tested for superiority if noninferiority criteria were met – Primary endpoint: composite of cardiovascular death, nonfatal MI, and nonfatal stroke • Some primary -

Dipeptidyl Peptidase-IV Inhibitors: Pharmacological Profile and Clinical Use
F E A T U R E A R TICLE Dipeptidyl Peptidase-IV Inhibitors: Pharmacological Profile and Clinical Use John R. White, Jr., PA, PharmD decade and a half ago, the on insulin biosynthesis and its inhibition creation of molecules that circumvent or choice of an oral antihypergly- of glucagon release.2 reduce the rate degradation by DPP-IV Acemic agent for any particu- Because GLP-1 stimulates insulin while maintaining the agonist effects of lar patient was in some ways a debate secretion only under hyperglycemic GLP-1 has been pursued aggressively. of nuance. Sulfonylureas (SUs) were conditions, there is minimal risk of One GLP-1 analog (exenatide) is avail- the only class available, and provid- hypoglycemia, making this molecule and able in the United States, and another ers were left to sift though pharmacoki- its congeners likely candidates for use as (liraglutide) is in phase III trials. netic, small efficacy, and sometimes sig- antihyperglycemic agents. GLP-1 is also In addition to GLP-1 analogs, mol- nificant side effect differences among associated with increased satiety, possi- ecules that inhibit the activity of DPP-IV the various choices within this class. The bly because it reduces the rate of gastric and thereby prolong the activity of situation today demands a more robust emptying. People with type 2 diabetes endogenous GLP-1 are of great interest. evaluation of multiple categories of med- have reduced circulating levels of GLP-1 Because GLP-1 analogs are proteina- ications with different mechanisms of but retain their ability to respond to this cious in structure, they will most likely action. -

Therapeutic Class Overview Dipeptidyl Peptidase-4 (DPP-4) Inhibitors
Therapeutic Class Overview Dipeptidyl Peptidase-4 (DPP-4) Inhibitors Therapeutic Class Overview/Summary: The dipeptidyl peptidase-4 (DPP-4) inhibitors are one of two incretin-based therapies currently available for the management of type 2 diabetes. The DPP-4 inhibitors linagliptin, saxagliptin, and sitagliptin, are available as single-entity agents (linagliptin [Tradjenta®], saxagliptin [Onglyza®], and sitagliptin [Januvia®]) or in fixed-dose combination products with metformin (linagliptin/metformin [Jentadueto®], saxagliptin/metformin [Kombiglyze ER®], and sitagliptin/metformin [Janumet®, Janumet XR®]) or simvastatin (sitagliptin/simvastatin [Juvisync®]). Single-entity agents are available for use either as monotherapy or in combination with other antidiabetic agents. The fixed-dose combination products are available for use when treatment with both drug components is appropriate.1-8 The DPP-4 inhibitors reversibly block the enzyme DPP-4, which is responsible for the rapid degradation of endogenous incretin hormones. These hormones are involved in the regulation of insulin and have multiple antidiabetic actions, including the enhancement of meal stimulated insulin secretion, decreased glucagon secretion, improvements in β cell function, and slowing of gastric emptying. Through their effect on these hormones, the DPP-4 inhibitors primarily target post-prandial glucose and have also been shown to decrease fasting plasma glucose. In general, this medication class is associated with a favorable side effect profile and also have a weight neutral effect compared to other antidiabetic agents commonly used in the management of type 2 diabetes.9-11 Most of products within this medication class are available for once-daily dosing; however, the fixed-dose combination products containing metformin immediate- release require twice-daily dosing. -

Oral Anti-Diabetic Agents-Review and Updates
British Journal of Medicine & Medical Research 5(2): 134-159, 2015, Article no.BJMMR.2015.016 ISSN: 2231-0614 SCIENCEDOMAIN international www.sciencedomain.org Oral Anti-Diabetic Agents-Review and Updates Patience O. Osadebe1, Estella U. Odoh2 and Philip F. Uzor1* 1Department of Pharmaceutical and Medicinal Chemistry, Faculty of Pharmaceutical Sciences, University of Nigeria, Nsukka, Enugu State, 410001, Nigeria. 2Department of Pharmacognosy and Environmental Medicine, Faculty of Pharmaceutical Sciences, University of Nigeria, Nsukka, Enugu State, 410001, Nigeria. Authors’ contributions Author POO designed the study, participated in the literature search. Author EUO participated in designing the work and in searching the literature. Author PFU participated in designing the work, searched the literature and wrote the first draft of the manuscript. All authors read and approved the final manuscript. Article Information DOI:10.9734/BJMMR/2015/8764 Editor(s): (1) Mohamed Essa, Department of Food Science and Nutrition, Sultan Qaboos University, Oman. (2) Franciszek Burdan, Experimental Teratology Unit, Human Anatomy Department, Medical University of Lublin, Poland and Radiology Department, St. John’s Cancer Center, Poland. Reviewers: (1) Anonymous, Bushehr University of Medical, Iran. (2) Anonymous, Tehran University of Medical Sciences, Iran. (3) Anonymous, King Fahad Armed Forces Hospital, Saudi Arabia. (4) Awadhesh Kumar Sharma, Mlb Medical College, Jhansi, UP, India. Peer review History: http://www.sciencedomain.org/review-history.php?iid=661&id=12&aid=5985 Received 30th December 2013 Review Article Accepted 13th March 2014 Published 8th September 2014 ABSTRACT Diabetes is a chronic metabolic disorder with high mortality rate and with defects in multiple biological systems. Two major types of diabetes are recognized, type 1 and 2 with type 2 diabetes (T2D) being by far the more prevalent type. -

Diabetes Medications
DIABETES MEDICATIONS Type of Drug and How it Generic Brand Name How Is it Taken? A1C Weight Risk for Works Name Change Change Hypoglycemia Consider Before Choosing This Medication Biguanide Lowers the amount of glucose metformin Glucophage 1 to 2 times a day, with or 1-2% None No Side effects: Indigestion, diarrhea, nausea. These are more likely to occur with released from the liver. Glucophage XR, without food higher doses. Helps your body absorb and use Glumetza, Possible risks: Avoid drinking more alcohol than normal. Take with caution if you more glucose. Fortamet, have kidney or liver problems. Riomet (liquid) Talk with your health care provider if you need an X-ray or CT scan with dye. Your metformin may be stopped for the test. Addition considerations: Recommended as first-line therapy by ADA and AACE. May reduce risk of cardiovascular events and death. Low-cost option. Sulfonylureas Helps the pancreas release more glimepiride Amaryl 1 to 2 times a day 1-2% Gain Yes Side effects: Hypoglycemia (low blood glucose), weight gain, nausea. insulin. glipizide Glucotrol and (average Possible risks: Take with caution if you have liver or kidney problems or are 65 Glucotrol XL 2 to 3 years of age or older. glyburide Diabeta pounds) Additional considerations: If cost is a major factor. glyburide- micronized Glynase DPP-4 Inhibitors “Gliptins” Helps your body use incretins. sitagliptin Januvia Once a day 0.6-1% None No Side effects: Headaches, nose and sinus congestion. These are hormones that make saxagliptin Onglyza Possible risks: May cause pancreatitis (inflammation of the pancreas). -

Metformin: Myths, Misunderstandings and Lessons from History
VOLUME 36 : NUMBER 2 : APRIL 2013 EDITORIal Metformin: myths, misunderstandings and lessons from history Gillian Shenfield Clinical trials of new drugs may overstate efficacy and could be minimised by a ‘start low, go slow’ approach Consultant clinical not identify adverse effects. It is therefore unusual to dosing. pharmacologist for the passage of time to reveal that a drug is less Sydney Also in 1957 an American group published similar toxic, has greater efficacy and a wider range of results for phenformin (phenylethyl biguanide). uses than first claimed. For decades metformin was Phenformin was energetically marketed worldwide Key words misunderstood, vilified and banned in many countries, biguanides, lactic acidosis, by Ciba-Geigy, but by 1959 an association with lactic but it is now one of the most prescribed drugs in type 2 diabetes acidosis was reported. Unfortunately, this report the world. In 2010 there were more than 100 million generated little interest. In contrast, metformin was prescriptions worldwide for metformin, alone and in manufactured by a small French company and, Aust Prescr 2013;36:38–9 combination tablets. among developed countries, was only the preferred Metformin was developed from a herb, Galega biguanide in France and Scotland. officinalis*, which was used for centuries to treat In the 1970s the number of reports of phenformin- many ailments including polyuria. It is a rich source related lactic acidosis and deaths increased. In 1977 of the toxic substance guanidine. A less toxic it was removed from the market in the USA and also alkaloid, galegine, was identified in France just before withdrawn from many other countries.