A Review on Evolution in Triglyceride Determination
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Valstybinės Vaistų Kontrolės Tarnybos Prie Lietuvos Respublikos Sveikatos Apsaugos Ministerijos Viršininko Įsakymas
VALSTYBINĖS VAISTŲ KONTROLĖS TARNYBOS PRIE LIETUVOS RESPUBLIKOS SVEIKATOS APSAUGOS MINISTERIJOS VIRŠININKO ĮSAKYMAS DĖL VALSTYBINĖS VAISTŲ KONTROLĖS TARNYBOS PRIE LIETUVOS RESPUBLIKOS SVEIKATOS APSAUGOS MINISTERIJOS VIRŠININKO 2006 M. LAPKRIČIO 2 D. ĮSAKYMO NR. 1A-658 „DĖL TARPTAUTINIŲ PREKĖS ŽENKLU NEREGISTRUOTŲ VAISTINIŲ MEDŽIAGŲ PAVADINIMŲ ATITIKMENŲ LIETUVIŲ KALBA SĄRAŠO PATVIRTINIMO“ PAKEITIMO 2011 m. gegužės 5 d. Nr. 1A-416 Vilnius Atsižvelgdamas į Pasaulinės sveikatos organizacijos 2011 m. paskelbtą 65-ąjį Rekomenduojamų tarptautinių prekės ženklu neregistruotų vaistinių medžiagų pavadinimų (INN) sąrašą, p a k e i č i u Tarptautinių prekės ženklu neregistruotų vaistinių medžiagų pavadinimų atitikmenų lietuvių kalba sąrašą, patvirtintą Valstybinės vaistų kontrolės tarnybos prie Lietuvos Respublikos sveikatos apsaugos ministerijos viršininko 2006 m. lapkričio 2 d. įsakymu Nr. 1A-658 „Dėl Tarptautinių prekės ženklu neregistruotų vaistinių medžiagų pavadinimų atitikmenų lietuvių kalba sąrašo patvirtinimo“ (Žin., 2006, Nr. 119-4557; 2007, Nr. 13-519, Nr. 43-1672; 2008, Nr. 9- 330, Nr. 24-896; 2010, Nr. 152-7773): 1. Papildau nauja eilute, kurią po eilutės „Amtolmetin guacil Amtolmetinas guacilas Amtolmetinum guacilum“ išdėstau taip: „Amuvatinib Amuvatinibas Amuvatinibum“ 2. Papildau nauja eilute, kurią po eilutės „Anagestone Anagestonas Anagestonum“ išdėstau taip: „Anagliptin Anagliptinas Anagliptinum“ 3. Papildau nauja eilute, kurią po eilutės „Atazanavir Atazanaviras Atazanavirum“ išdėstau taip: „Atecegatran Atecegatranas Atecegatranum“ -
Treatment Patterns, Persistence and Adherence Rates in Patients with Type 2 Diabetes Mellitus in Japan: a Claims- Based Cohort Study
Open access Research BMJ Open: first published as 10.1136/bmjopen-2018-025806 on 1 March 2019. Downloaded from Treatment patterns, persistence and adherence rates in patients with type 2 diabetes mellitus in Japan: a claims- based cohort study Rimei Nishimura,1 Haruka Kato,2 Koichi Kisanuki,2 Akinori Oh,2 Shinzo Hiroi,2 Yoshie Onishi,3 Florent Guelfucci,4 Yukio Shimasaki2 To cite: Nishimura R, Kato H, ABSTRACT Strengths and limitations of this study Kisanuki K, et al. Treatment Objective To determine real-world trends in antidiabetic patterns, persistence and drug use, and persistence and adherence, in Japanese ► This retrospective evaluation of administrative adherence rates in patients patients with type 2 diabetes mellitus (T2DM). with type 2 diabetes mellitus claims data (2011–2015) using the Japan Medical Design Retrospective evaluation of administrative claims in Japan: a claims-based Data Center (JMDC) and Medical Data Vision (MDV) data (2011–2015) using the Japan Medical Data Center cohort study. BMJ Open databases was conducted to determine real-world (JMDC) and Medical Data Vision (MDV) databases. 2019;9:e025806. doi:10.1136/ trends in antidiabetic drug use, and persistence and Setting Analysis of two administrative claims databases bmjopen-2018-025806 adherence, in Japanese patients with type 2 dia- for Japanese patients with T2DM. betes mellitus (T2DM); 40 908 and 90 421 patients ► Prepublication history and Participants Adults (aged ≥18 years) with an International additional material for this were included from the JMDC and MDV databases, Classification of Diseases, 10th Revision code of T2DM and paper are available online. To respectively. at least one antidiabetic drug prescription. -

Natural Products As Lead Compounds for Sodium Glucose Cotransporter (SGLT) Inhibitors
Reviews Natural Products as Lead Compounds for Sodium Glucose Cotransporter (SGLT) Inhibitors Author ABSTRACT Wolfgang Blaschek Glucose homeostasis is maintained by antagonistic hormones such as insulin and glucagon as well as by regulation of glu- Affiliation cose absorption, gluconeogenesis, biosynthesis and mobiliza- Formerly: Institute of Pharmacy, Department of Pharmaceu- tion of glycogen, glucose consumption in all tissues and glo- tical Biology, Christian-Albrechts-University of Kiel, Kiel, merular filtration, and reabsorption of glucose in the kidneys. Germany Glucose enters or leaves cells mainly with the help of two membrane integrated transporters belonging either to the Key words family of facilitative glucose transporters (GLUTs) or to the Malus domestica, Rosaceae, Phlorizin, flavonoids, family of sodium glucose cotransporters (SGLTs). The intesti- ‑ SGLT inhibitors, gliflozins, diabetes nal glucose absorption by endothelial cells is managed by SGLT1, the transfer from them to the blood by GLUT2. In the received February 9, 2017 kidney SGLT2 and SGLT1 are responsible for reabsorption of revised March 3, 2017 filtered glucose from the primary urine, and GLUT2 and accepted March 6, 2017 GLUT1 enable the transport of glucose from epithelial cells Bibliography back into the blood stream. DOI http://dx.doi.org/10.1055/s-0043-106050 The flavonoid phlorizin was isolated from the bark of apple Published online April 10, 2017 | Planta Med 2017; 83: 985– trees and shown to cause glucosuria. Phlorizin is an inhibitor 993 © Georg Thieme Verlag KG Stuttgart · New York | of SGLT1 and SGLT2. With phlorizin as lead compound, specif- ISSN 0032‑0943 ic inhibitors of SGLT2 were developed in the last decade and some of them have been approved for treatment mainly of Correspondence type 2 diabetes. -

Effect of Oral Hypoglycaemic Agents on Glucose Tolerance in Pancreatic Diabetes
Gut: first published as 10.1136/gut.13.4.285 on 1 April 1972. Downloaded from Gut, 1972, 13, 285-288 Effect of oral hypoglycaemic agents on glucose tolerance in pancreatic diabetes B. I. JOFFE, W. P. U. JACKSON, S. BANK, AND A. I. VINIK From the Department of Medicine, Witwatersrand University Medical School, Johannesburg, the Gastro- intestinal and Endocrine Research Units of Cape Town University Medical School, and the Chemical Pathology Department of Natal University, South Africa SUMMARY The short-term therapeutic effect of oral hypoglycaemic agents has been assessed in 12 patients with symptomatic diabetes secondary to chronic pancreatitis (pancreatic diabetes). In six patients who had moderate to severe carbohydrate intolerance, associated with severe insulino- paenia during arginine infusion, the potent sulphonylurea chlorpropamide produced no change in the fasting blood glucose level after two weeks of treatment. This contrasted with the significant reduction produced in a matched group of maturity-onset primary diabetics. The six patients with milder diabetes, and a greater (although still subnormal) insulin secretory capacity, showed an improvement in oral glucose tolerance during the first hour following glucose administration while on chlorpropamide. When the biguanide phenformin was substituted for chlorpropamide in five of these patients, a statistically insignificant improvement in glucose tolerance was observed during treatment. Applications of these findings to the practical management of pancreatic diabetes are briefly http://gut.bmj.com/ considered. Chronic pancreatitis is frequently complicated by and two women, ranging from 30 to 67 years of age. diabetes (pancreatic diabetes). Recent studies The diagnosis of pancreatitis was confirmed on the utilizing immunoassay procedures (Joffe, Bank, basis of a gross abnormality in at least two aspects of Jackson, Keller, O'Reilly, and Vinik, 1968; Anderson the pancreatic function test, namely, a low volume of on September 24, 2021 by guest. -

Remogliflozin Etabonate, a Selective Inhibitor of the Sodium-Glucose
Clinical Care/Education/Nutrition/Psychosocial Research BRIEF REPORT Remogliflozin Etabonate, a Selective Inhibitor of the Sodium-Glucose Transporter 2, Improves Serum Glucose Profiles in Type 1 Diabetes 1,2 3 SUNDER MUDALIAR, MD JUNE YE, PHD placebo (placebo), 2) mealtime insulin 1 3 DEBRA A. ARMSTRONG, BA, RN, CCRC ELIZABETH K. HUSSEY, PHARMD 2 3 injection + RE placebo (prandial insulin), ANNIE A. MAVIAN, MD DEREK J. NUNEZ, MD 3 3 1,2 ) placebo insulin injection + 50 mg RE (RE ROBIN O’CONNOR-SEMMES, PHD ROBERT R. HENRY, MD 3 3 50 mg), 4) placebo insulin injection + 150 PATRICIA K. MYDLOW, BS ROBERT L. DOBBINS, MD, PHD mg RE (RE 150 mg), and 5) placebo insulin injection + 500 mg RE (RE 500 mg). d fl Each individual received 75-g oral OBJECTIVES Remogli ozin etabonate (RE), an inhibitor of the sodium-glucose transporter glucose and identical meals during all 2, improves glucose profiles in type 2 diabetes. This study assessed safety, tolerability, pharma- cokinetics, and pharmacodynamics of RE in subjects with type 1 diabetes. treatment periods. Frequent samples were obtained for measurement of plasma RESEARCH DESIGN AND METHODSdTen subjects managed with continuous sub- glucose and insulin concentrations. Urine cutaneous insulin infusion were enrolled. In addition to basal insulin, subjects received five samples were collected for 24 h to assess randomized treatments: placebo, prandial insulin, 50 mg RE, 150 mg RE, and mg RE 500. creatinine clearance and glucose excre- d tion. Plasma samples were collected for RESULTS Adverse events and incidence of hypoglycemia with RE did not differ from placebo fl and prandial insulin groups. -
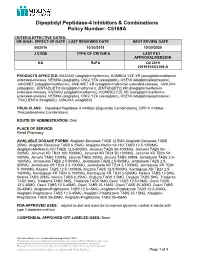
Dipeptidyl Peptidase-4 Inhibitors and Combinations
Dipeptidyl Peptidase-4 Inhibitors & Combinations Policy Number: C5169A CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DATE 06/2016 10/30/2019 10/30/2020 J CODE TYPE OF CRITERIA LAST P&T APPROVAL/VERSION NA RxPA Q4 2019 20191030C5169-A PRODUCTS AFFECTED: KAZANO (alogliptin/metformin), KOMBIGLYZE XR (saxagliptin/metformin extended-release), NESINA (alogliptin), ONGLYZA (saxagliptin), OSENI (alogliptin/pioglitazone), JANUMET (sitagliptin/metformin), JANUMET XR (sitagliptin/metformin extended-release), JANUVIA (sitagliptin), JENTADUETO (linagliptin/metformin), JENTADUETO XR (linagliptin/metformin extended-release), KAZANO (alogliptin/metformin), KOMBIGLYZE XR (saxagliptin/metformin extended-release), NESINA (alogliptin), ONGLYZA (saxagliptin), OSENI (alogliptin/pioglitazone) TRADJENTA (linagliptin), JANUVIA (sitagliptin) DRUG CLASS: Dipeptidyl Peptidase-4 Inhibitor-(Biguanide Combinations), DPP-4 Inhibitor- Thiazolidinedione Combinations ROUTE OF ADMINISTRATION: Oral PLACE OF SERVICE: Retail Pharmacy AVAILABLE DOSAGE FORMS: Alogliptin Benzoate TABS 12.5MG,Alogliptin Benzoate TABS 25MG, Alogliptin Benzoate TABS 6.25MG, Alogliptin-Metformin HCl TABS 12.5-1000MG Alogliptin-Metformin HCl TABS 12.5-500MG, Janumet TABS 50-1000MG, Janumet TABS 50- 500MG, Janumet XR TB24 100-1000MG, Janumet XR TB24 50-1000MG, Janumet XR TB24 50- 500MG, Januvia TABS 100MG, Januvia TABS 25MG, Januvia TABS 50MG, Jentadueto TABS 2.5- 1000MG, Jentadueto TABS 2.5-500MG, Jentadueto TABS 2.5-500MG, Jentadueto TABS 2.5- 850MG, Jentadueto -

Polyhexamethylene Biguanide Hydrochloride) As Used in Cosmetics
Safety Assessment of Polyaminopropyl Biguanide (polyhexamethylene biguanide hydrochloride) as Used in Cosmetics Status: Tentative Report for Public Comment Release Date: September 26, 2017 Panel Date: December 4-5, 2017 All interested persons are provided 60 days from the above date to comment on this safety assessment and to identify additional published data that should be included or provide unpublished data which can be made public and included. Information may be submitted without identifying the source or the trade name of the cosmetic product containing the ingredient. All unpublished data submitted to CIR will be discussed in open meetings, will be available at the CIR office for review by any interested party and may be cited in a peer-reviewed scientific journal. Please submit data, comments, or requests to the CIR Executive Director, Dr. Bart Heldreth. The 2017 Cosmetic Ingredient Review Expert Panel members are: Chair, Wilma F. Bergfeld, M.D., F.A.C.P.; Donald V. Belsito, M.D.; Ronald A. Hill, Ph.D.; Curtis D. Klaassen, Ph.D.; Daniel C. Liebler, Ph.D.; James G. Marks, Jr., M.D.; Ronald C. Shank, Ph.D.; Thomas J. Slaga, Ph.D.; and Paul W. Snyder, D.V.M., Ph.D. The CIR Executive Director is Bart Heldreth, Ph.D. This report was prepared by Wilbur Johnson, Jr., M.S., Senior Scientific Analyst and Ivan Boyer, Ph.D., former Senior Toxicologist. © Cosmetic Ingredient Review 1620 L STREET, NW, SUITE 1200 ◊ WASHINGTON, DC 20036-4702 ◊ PH 202.331.0651 ◊ FAX 202.331.0088 ◊ [email protected] ABSTRACT: The Cosmetic Ingredient Review (CIR) Expert Panel (Panel) reviewed the safety of Polyaminopropyl Biguanide (polyhexamethylene biguanide hydrochloride), which functions as a preservative in cosmetic products. -

An Emerging Protagonist: Sodium Glucose Co-Transporters (Sglts)
abetes & Di M f e o t a l b a o Ahmed et al., J Diabetes Metab 2014, 5:4 n l r i s u m o DOI: 10.4172/2155-6156.1000358 J Journal of Diabetes and Metabolism ISSN: 2155-6156 Review Article Open Access An Emerging Protagonist: Sodium Glucose Co-transporters (SGLTs) as a Burgeoning Target for the Treatment of Diabetes Mellitus Danish Ahmed1*, Manju Sharma2, Vikas Kumar1 and Yadav Pankajkumar Subhashchandra1 1Department of Pharmaceutical Sciences, Sam Higginbottom Institute of Agriculture, Technology and Sciences (SHIATS)-Deemed University, India 2Department of Pharmacology, JamiaHamdard University, Hamdard Nagar, New Delhi, India Abstract Contemporary therapies to rationalize the hyperglycaemia in type 2 diabetes mellitus (T2DM) generally involve insulin-dependent mechanisms and lose their effectiveness as pancreatic b-cell function decreases to a greater extent. Kidney emerges out as a novel and potential target to trim down the complications of T2DM. The filtered glucose is reabsorbed principally through the sodium glucose co-transporter-2 (SGLT2), a low affinity transport system, which are present at the luminal surface cells that covers the first segment of proximal tubules. Competitive inhibition of SGLT2 therefore represents an innovative therapeutic strategy for the treatment of hyperglycaemia and/or obesity in patients with type 1 or type 2 diabetes by enhancing glucose and energy loss through the urine. Selective inhibitors of SGLT2 reduce glucose reabsorption, causing excess glucose to be eliminated in the urine; this decreases plasma glucose. SGLT2 inhibitors are coupled with osmotic dieresis and loss of weight which aid in reducing the blood pressure. The observation that individuals with familial renal glycosuria maintain normal long- term kidney function provides some encouragement that this mode of action will not adversely affect renal function. -

Type 2 Diabetes Treatment Recommendations Update
abetes & Di M f e o t a l b a o Cornell, J Diabetes Metab 2014, 5:8 n l r i s u m o DOI: 10.4172/2155-6156.1000414 J Journal of Diabetes and Metabolism ISSN: 2155-6156 Review Article Open Access Type 2 Diabetes Treatment Recommendations Update: Appropriate Use of Dipeptidyl Peptidase-4 Inhibitors Susan Cornell* Midwestern University, Chicago College of Pharmacy, Downers Grove, IL, USA Abstract In this article, recommendations from the 2012 American Diabetes Association (ADA)/European Association for the Study of Diabetes (EASD) position statement are discussed with an emphasis on the appropriate use of Dipeptidyl Peptidase-4 (DPP-4) inhibitors in individuals with Type 2 Diabetes Mellitus (T2DM). The 2012 ADA/EASD position statement emphasizes individualization of treatment, with glycated hemoglobin (A1C) targets being determined for each patient based on life expectancy, complications, disease duration, comorbidities, such as cardiovascular disease or cognitive impairment, and the risk of hypoglycemia and other adverse events. Patients’ attitudes and support systems should also be considered. Recommendations for pharmacotherapy are less prescriptive and should be based on a patient’s needs, preferences, and tolerances. In general, metformin is recommended as first- line therapy for most patients, although combination of 2 noninsulin agents or insulin alone should be considered in patients with baseline A1C ≥ 9.0%. Add-on therapy to metformin will likely be needed to achieve and maintain glycemic control as the disease progresses. It is important to avoid therapies that increase the risk of weight gain or and, especially in older patients, hypoglycemia. As discussed in this review, DPP-4 inhibitors are well tolerated and effectively lower A1C and improve β-cell function without increasing the risk of hypoglycemia and weight gain. -

Exploring Glycosuria As a Mechanism for Weight and Fat Mass Reduction. a Pilot Study with Remogliflozin Etabonate and Sergliflozin Etabonate in Healthy Obese Subjects
Journal of Clinical & Translational Endocrinology 1 (2014) e3ee8 Contents lists available at ScienceDirect Journal of Clinical & Translational Endocrinology journal homepage: www.elsevier.com/locate/jcte Research Paper Exploring glycosuria as a mechanism for weight and fat mass reduction. A pilot study with remogliflozin etabonate and sergliflozin etabonate in healthy obese subjects Antonella Napolitano a,*, Sam Miller a, Peter R. Murgatroyd c, Elizabeth Hussey b, Robert L. Dobbins b, Edward T. Bullmore a, Derek J.R. Nunez b View metadata, citation and similar papers at core.ac.uk brought to you by CORE a Clinical Unit in Cambridge, GlaxoSmithKline, Addenbrookes Hospital, Cambridge, UK b Metabolic Pathways and Cardiovascular Unit, GlaxoSmithKline,provided by NC, Elsevier USA - Publisher Connector c Wellcome Trust Clinical Research Facility, Cambridge University Hospital NHS Trust, UK article info abstract Article history: Inhibitors of sodium-dependent glucose co-transporter 2 (SGLT2) increase glucose excretion in the urine Received 16 October 2013 and improve blood glucose in Type 2 diabetes mellitus. Glycosuria provides an energy and osmotic drain Received in revised form that could alter body composition. We therefore conducted a pilot study comparing the effects on body 26 November 2013 composition of two SGLT2 inhibitors, remogliflozin etabonate (RE) 250 mg TID (n ¼ 9) and sergliflozin Accepted 5 December 2013 etabonate (SE) (1000 mg TID) (n ¼ 9), with placebo (n ¼ 12) in obese non-diabetic subjects. Both drugs Available online 7 February 2014 were well tolerated during 8 weeks of dosing, and the most common adverse event was headache. No urinary tract infections were observed, but there was one case of vaginal candidiasis in the RE group. -

Glycemic Management of Type 2 Diabetes
Glycemic Management of Type 2 Diabetes Gail Nunlee-Bland, M.D. Professor Medicine & Pediatrics Director, Diabetes Treatment Center Howard University 1 Disclosures • None Learning Objectives • Understand the importance of lifestyle therapy in diabetes management • Know the classes of antihyperglycemic agents, mechanism of action, benefits and side effects of these agents • Recognize the importance of individualized treatment goals for diabetic patients AACE Comprehensive Care Plan Disease management from Antihyperglycemic a multidisciplinary team pharmacotherapy Comprehensive Care Plan Comprehensive diabetes Therapeutic lifestyle self-education for the change patient 4 Handelsman YH, et al. Endocr Pract. 2015;21(suppl 1):1-87. Glycemic Management of Type 2 Diabetes THERAPEUTIC LIFESTYLE CHANGE 5 Components of Therapeutic Lifestyle Change • Healthful eating • Sufficient physical activity • Sufficient sleep • Avoidance of tobacco products • Limited alcohol consumption • Stress reduction 6 Handelsman YH, et al. Endocr Pract. 2015;21(suppl 1):1-87. Glycemic Management of Type 2 Diabetes ANTIHYPERGLYCEMIC THERAPY 7 Cardiovascular Outcomes Trials: A Brief History • 2008 FDA guidance mandating assessment of CV safety of all antihyperglycemic agents in RCTs – Designed as noninferiority studies to demonstrate study drug was not associated with more MACE than placebo • Some study designs tested for superiority if noninferiority criteria were met – Primary endpoint: composite of cardiovascular death, nonfatal MI, and nonfatal stroke • Some primary -

Dipeptidyl Peptidase-IV Inhibitors: Pharmacological Profile and Clinical Use
F E A T U R E A R TICLE Dipeptidyl Peptidase-IV Inhibitors: Pharmacological Profile and Clinical Use John R. White, Jr., PA, PharmD decade and a half ago, the on insulin biosynthesis and its inhibition creation of molecules that circumvent or choice of an oral antihypergly- of glucagon release.2 reduce the rate degradation by DPP-IV Acemic agent for any particu- Because GLP-1 stimulates insulin while maintaining the agonist effects of lar patient was in some ways a debate secretion only under hyperglycemic GLP-1 has been pursued aggressively. of nuance. Sulfonylureas (SUs) were conditions, there is minimal risk of One GLP-1 analog (exenatide) is avail- the only class available, and provid- hypoglycemia, making this molecule and able in the United States, and another ers were left to sift though pharmacoki- its congeners likely candidates for use as (liraglutide) is in phase III trials. netic, small efficacy, and sometimes sig- antihyperglycemic agents. GLP-1 is also In addition to GLP-1 analogs, mol- nificant side effect differences among associated with increased satiety, possi- ecules that inhibit the activity of DPP-IV the various choices within this class. The bly because it reduces the rate of gastric and thereby prolong the activity of situation today demands a more robust emptying. People with type 2 diabetes endogenous GLP-1 are of great interest. evaluation of multiple categories of med- have reduced circulating levels of GLP-1 Because GLP-1 analogs are proteina- ications with different mechanisms of but retain their ability to respond to this cious in structure, they will most likely action.