Diabetes Medications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Treatment Patterns, Persistence and Adherence Rates in Patients with Type 2 Diabetes Mellitus in Japan: a Claims- Based Cohort Study
Open access Research BMJ Open: first published as 10.1136/bmjopen-2018-025806 on 1 March 2019. Downloaded from Treatment patterns, persistence and adherence rates in patients with type 2 diabetes mellitus in Japan: a claims- based cohort study Rimei Nishimura,1 Haruka Kato,2 Koichi Kisanuki,2 Akinori Oh,2 Shinzo Hiroi,2 Yoshie Onishi,3 Florent Guelfucci,4 Yukio Shimasaki2 To cite: Nishimura R, Kato H, ABSTRACT Strengths and limitations of this study Kisanuki K, et al. Treatment Objective To determine real-world trends in antidiabetic patterns, persistence and drug use, and persistence and adherence, in Japanese ► This retrospective evaluation of administrative adherence rates in patients patients with type 2 diabetes mellitus (T2DM). with type 2 diabetes mellitus claims data (2011–2015) using the Japan Medical Design Retrospective evaluation of administrative claims in Japan: a claims-based Data Center (JMDC) and Medical Data Vision (MDV) data (2011–2015) using the Japan Medical Data Center cohort study. BMJ Open databases was conducted to determine real-world (JMDC) and Medical Data Vision (MDV) databases. 2019;9:e025806. doi:10.1136/ trends in antidiabetic drug use, and persistence and Setting Analysis of two administrative claims databases bmjopen-2018-025806 adherence, in Japanese patients with type 2 dia- for Japanese patients with T2DM. betes mellitus (T2DM); 40 908 and 90 421 patients ► Prepublication history and Participants Adults (aged ≥18 years) with an International additional material for this were included from the JMDC and MDV databases, Classification of Diseases, 10th Revision code of T2DM and paper are available online. To respectively. at least one antidiabetic drug prescription. -

Management of Hyperglycaemia and Steroid (Glucocorticoid) Therapy
Management of Hyperglycaemia and Steroid (Glucocorticoid) Therapy October 2014 This document is coded JBDS 08 in the series of JBDS documents Other JBDS documents: Admissions avoidance and diabetes: guidance for clinical commissioning groups and clinical team; December 2013, JBDS 07 The management of the hyperosmolar hyperglycaemic state (HHS) in adults with diabetes; August 2012, JBDS 06 Glycaemic management during the inpatient enteral feeding of stroke patients with diabetes; June 2012, JBDS 05 Self-management of diabetes in hospital; March 2012, JBDS 04 Management of adults with diabetes undergoing surgery and elective procedures: improving standards; April 2011, JBDS 03 The Management of Diabetic Ketoacidosis in Adults; revised September 2013, JBDS 02 The hospital management of hypoglycaemia in adults with diabetes mellitus; revised September 2013, JBDS 01 These documents are available to download from: ABCD website: www.diabetologists-abcd.org.uk/JBDS/JBDS.htm Diabetes UK website: www.diabetes.org.uk Contents Page Foreword 4 Authorship and acknowledgments 5-6 Introduction 7 Steroids - mechanism of action 8 Steroid therapy – impact on blood glucose 9 Glucose targets 10 Glucose monitoring 11 Diabetes treatment options 12-13 Treatment of steroid induced hyperglycaemia 14-15 Hospital discharge 16-17 Steroid treatment in pregnancy 18 Steroid treatment in end of life 19 Audit standards 20 Controversial areas 21 References 22 Appendix 1 – Algorithm to show treatment of steroid 23 induced diabetes Appendix 2 – Algorithm to show management of patients 24 with diabetes on once daily steroids Appendix 3 – End of life steroid management 25 Appendix 4 – Patient letter – Glucose monitoring and 26 steroid use 3 Foreword This is the latest in the series of Joint British Diabetes Societies for Inpatient Care (JBDS-IP) guidelines, and focuses on steroid induced hyperglycaemia and steroid induced diabetes. -

Diabetes Medication Reference for Clinicians This Table Provides Clinicians a Brief Overview of Examples of Medications Used to Treat Diabetes
Diabetes Medication Reference for Clinicians This table provides clinicians a brief overview of examples of medications used to treat diabetes. This is not a complete list and is not intended to be used as a sole reference. Nursing responsibilities with ALL diabetes medications: Emphasize importance of self-monitoring of blood glucose (SMBG); teach to be aware of signs/symptoms of allergic reactions; teach to be aware of possible side effects and contraindications; and monitor A1C levels. Oral Medication Action Possible Side-effects Contraindications Nursing Responsibilities Biguanide • Lowers glucose levels • Anorexia, nausea, • Renal disease Patient education: • metformin by decreasing the vomiting, diarrhea - • Liver failure or • Take with food (Glucophage, amount of glucose usually occurs during alcohol abuse (can • Keep appointments Glucophage XR, produced by the liver initiation of the drug result in lactic for regular kidney Glumetza, Fortamet, • Increases glucose • Vitamin B-12 acidosis) function lab tests Riomet) uptake in muscle deficiency • Temporarily held on • Avoid alcohol • Multiple combinations cells • Lactic acidosis day of procedures • Report abnormal with other classes • Improves (severe but rare) with dye and glucose levels • First line therapy for hyperglycemia & • Should not cause withheld 48 hours • Report s/s lactic type 2 diabetes; hypertriglyceridemia hypoglycemia as after the procedure; acidosis (weakness, current in obese patients monotherapy restart after drowsiness, malaise) recommendation is to with diabetes; may confirmation of renal start upon diagnosis promote weight loss function This material was prepared by Quality Insights, the Medicare Quality Innovation Network-Quality Improvement Organization supporting the Home Health Quality Improvement National 1 Campaign, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. -

Effect of Oral Hypoglycaemic Agents on Glucose Tolerance in Pancreatic Diabetes
Gut: first published as 10.1136/gut.13.4.285 on 1 April 1972. Downloaded from Gut, 1972, 13, 285-288 Effect of oral hypoglycaemic agents on glucose tolerance in pancreatic diabetes B. I. JOFFE, W. P. U. JACKSON, S. BANK, AND A. I. VINIK From the Department of Medicine, Witwatersrand University Medical School, Johannesburg, the Gastro- intestinal and Endocrine Research Units of Cape Town University Medical School, and the Chemical Pathology Department of Natal University, South Africa SUMMARY The short-term therapeutic effect of oral hypoglycaemic agents has been assessed in 12 patients with symptomatic diabetes secondary to chronic pancreatitis (pancreatic diabetes). In six patients who had moderate to severe carbohydrate intolerance, associated with severe insulino- paenia during arginine infusion, the potent sulphonylurea chlorpropamide produced no change in the fasting blood glucose level after two weeks of treatment. This contrasted with the significant reduction produced in a matched group of maturity-onset primary diabetics. The six patients with milder diabetes, and a greater (although still subnormal) insulin secretory capacity, showed an improvement in oral glucose tolerance during the first hour following glucose administration while on chlorpropamide. When the biguanide phenformin was substituted for chlorpropamide in five of these patients, a statistically insignificant improvement in glucose tolerance was observed during treatment. Applications of these findings to the practical management of pancreatic diabetes are briefly http://gut.bmj.com/ considered. Chronic pancreatitis is frequently complicated by and two women, ranging from 30 to 67 years of age. diabetes (pancreatic diabetes). Recent studies The diagnosis of pancreatitis was confirmed on the utilizing immunoassay procedures (Joffe, Bank, basis of a gross abnormality in at least two aspects of Jackson, Keller, O'Reilly, and Vinik, 1968; Anderson the pancreatic function test, namely, a low volume of on September 24, 2021 by guest. -

What You Need to Know: Centers for Medicare & Medicaid Services Part D Measure — Statin Use in Persons with Diabetes
T:8.5” What You Need to Know: Centers for Medicare & Medicaid Services Part D Measure — Statin Use in Persons With Diabetes UnitedHealthcare recognizes the time and effort you put into managing the health of your patients with diabetes. To help you be as efficient as possible, we’re offering this guide with detailed information about the Statin Use in Persons With Diabetes (SUPD) Part D measure from the Centers for Medicare & Medicaid Services (CMS). Defining the SUPD measure CMS defines this measure as the percentage of Medicare members with diabetes ages 40–75 who receive at least one fill of a statin medication in the measurement year. Members with diabetes are defined as those who have at least two fills of diabetes medications during the measurement year. Only pharmacy claims are used to identify and close care opportunities for this measure. Members who have end-stage renal disease (ESRD) and/or are in hospice care are excluded from the SUPD measure. Understanding measure rationale The SUPD measure is based on cholesterol guidelines from the American College of Cardiology/American Heart T:11” Association (ACC/AHA). The guidelines recommend moderate- to high-intensity statin therapy for patients ages 40–75 with diabetes to help prevent atherosclerotic cardiovascular disease (ASCVD).1,2 The guidelines: • Recognize patients ages 40–75 with diabetes are at a substantially higher lifetime risk for ASCVD events and experience greater morbidity and worse survival rates following the start of clinical ASCVD. • Indicate statins have been shown to be effective in reducing the risk for cardiovascular events. • Align with the American Diabetes Association in recommending statin therapy for patients ages 40–75 with diabetes to help prevent ASCVD.3 Reaching the SUPD target goal To successfully meet CMS requirements, men and women who fit the measure definition must be on a statin medication for the prevention of ASCVD, if clinically appropriate. -
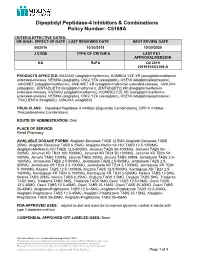
Dipeptidyl Peptidase-4 Inhibitors and Combinations
Dipeptidyl Peptidase-4 Inhibitors & Combinations Policy Number: C5169A CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DATE 06/2016 10/30/2019 10/30/2020 J CODE TYPE OF CRITERIA LAST P&T APPROVAL/VERSION NA RxPA Q4 2019 20191030C5169-A PRODUCTS AFFECTED: KAZANO (alogliptin/metformin), KOMBIGLYZE XR (saxagliptin/metformin extended-release), NESINA (alogliptin), ONGLYZA (saxagliptin), OSENI (alogliptin/pioglitazone), JANUMET (sitagliptin/metformin), JANUMET XR (sitagliptin/metformin extended-release), JANUVIA (sitagliptin), JENTADUETO (linagliptin/metformin), JENTADUETO XR (linagliptin/metformin extended-release), KAZANO (alogliptin/metformin), KOMBIGLYZE XR (saxagliptin/metformin extended-release), NESINA (alogliptin), ONGLYZA (saxagliptin), OSENI (alogliptin/pioglitazone) TRADJENTA (linagliptin), JANUVIA (sitagliptin) DRUG CLASS: Dipeptidyl Peptidase-4 Inhibitor-(Biguanide Combinations), DPP-4 Inhibitor- Thiazolidinedione Combinations ROUTE OF ADMINISTRATION: Oral PLACE OF SERVICE: Retail Pharmacy AVAILABLE DOSAGE FORMS: Alogliptin Benzoate TABS 12.5MG,Alogliptin Benzoate TABS 25MG, Alogliptin Benzoate TABS 6.25MG, Alogliptin-Metformin HCl TABS 12.5-1000MG Alogliptin-Metformin HCl TABS 12.5-500MG, Janumet TABS 50-1000MG, Janumet TABS 50- 500MG, Janumet XR TB24 100-1000MG, Janumet XR TB24 50-1000MG, Janumet XR TB24 50- 500MG, Januvia TABS 100MG, Januvia TABS 25MG, Januvia TABS 50MG, Jentadueto TABS 2.5- 1000MG, Jentadueto TABS 2.5-500MG, Jentadueto TABS 2.5-500MG, Jentadueto TABS 2.5- 850MG, Jentadueto -

Polyhexamethylene Biguanide Hydrochloride) As Used in Cosmetics
Safety Assessment of Polyaminopropyl Biguanide (polyhexamethylene biguanide hydrochloride) as Used in Cosmetics Status: Tentative Report for Public Comment Release Date: September 26, 2017 Panel Date: December 4-5, 2017 All interested persons are provided 60 days from the above date to comment on this safety assessment and to identify additional published data that should be included or provide unpublished data which can be made public and included. Information may be submitted without identifying the source or the trade name of the cosmetic product containing the ingredient. All unpublished data submitted to CIR will be discussed in open meetings, will be available at the CIR office for review by any interested party and may be cited in a peer-reviewed scientific journal. Please submit data, comments, or requests to the CIR Executive Director, Dr. Bart Heldreth. The 2017 Cosmetic Ingredient Review Expert Panel members are: Chair, Wilma F. Bergfeld, M.D., F.A.C.P.; Donald V. Belsito, M.D.; Ronald A. Hill, Ph.D.; Curtis D. Klaassen, Ph.D.; Daniel C. Liebler, Ph.D.; James G. Marks, Jr., M.D.; Ronald C. Shank, Ph.D.; Thomas J. Slaga, Ph.D.; and Paul W. Snyder, D.V.M., Ph.D. The CIR Executive Director is Bart Heldreth, Ph.D. This report was prepared by Wilbur Johnson, Jr., M.S., Senior Scientific Analyst and Ivan Boyer, Ph.D., former Senior Toxicologist. © Cosmetic Ingredient Review 1620 L STREET, NW, SUITE 1200 ◊ WASHINGTON, DC 20036-4702 ◊ PH 202.331.0651 ◊ FAX 202.331.0088 ◊ [email protected] ABSTRACT: The Cosmetic Ingredient Review (CIR) Expert Panel (Panel) reviewed the safety of Polyaminopropyl Biguanide (polyhexamethylene biguanide hydrochloride), which functions as a preservative in cosmetic products. -

Antidepressant Prescription Practices Among Primary Health Care Providers for Patients with Diabetes Mellitus
Research Article Curre Res Diabetes & Obes J Volume 2 Issue 4 - June 2017 Copyright © All rights are reserved by Gillian Bartlet DOI: 10.19080/CRDOJ.2017.2.555593 Antidepressant Prescription Practices among Primary Health Care Providers for Patients with Diabetes Mellitus Gagnon J, Lussier MT, Daskalopoulou SS, MacGibbon B, Bartlett G 1Department of Family Medicine, McGill University, Canada 2Department of Family Medicine and Emergency Medicine, Université de Montréal, Canada 3Department of Medicine, McGill University, Canada 4Department of Mathematics, Université du Québec à Montréal, Canada 5Department of Family Medicine, McGill University, Canada Submission: June 13, 2017; Published: June 27, 2017 *Corresponding author: Gillian Bartlett, Department of Family Medicine, McGill University, Canada, Tel: ; Fax: ; Email: Abstract Purpose: Depression is a common comorbidity in people with diabetes that increases the risk of poor diabetes control and diabetes- related complications. While treatment of depression is expected to help, some antidepressants have been associated with impaired glucose metabolism. Evidence is lacking in the scope of this problem for people with diabetes. The objective of this study is to describe the prescription of antidepressants for diabetic patients with a focus on medications suspected to impair glucose control. Methods: A cross-sectional study of electronic medical record data from 115 primary care practices in the Canadian Primary Care Sentinel Surveillance Network was conducted. Descriptive statistics were used to describe the prescription of antidepressants for people with diabetes between 2009 and 2014. Results: From the sample, 17,258 diabetic patients were prescribed at least one antidepressant (AD) between 2009 and 2014. In terms of pharmacological class, the greatest proportion of people were prescribed selective serotonin reuptake inhibitors (46.2%), followed by serotonin-norepinephrine reuptake inhibitors (24.3%) and tricyclic antidepressants (23.8%). -
Diabetes Management: Directory of Provider Resources (PDF)
DIABETES MANAGEMENT: DIRECTORY OF PROVIDER RESOURCES 2 Diabetes Management: Directory of Provider Resources ACKNOWLEDGMENTS Diabetes Management: Directory of Provider Resources was prepared with input from National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases; Centers for Medicare & Medicaid Services Advisory Panel on Outreach and Education; NORC at the University of Chicago; Jamie Murkey, MPH, PhD, Program Alignment and Partner Engagement Group 2019 summer intern; Asian Services in Action – International Community Health Center; Chinatown Public Health Center; Colorado Coalition for the Homeless; Garden City Community Health Center, Genesis Family Health; Jackson Medical Mall and Jackson Hinds Comprehensive Health Center; Montefiore Medical Center; Nash Health Care Systems; Sun Life Family Health Center; and Bryan W. Whitfield Memorial Hospital, Tombigbee Healthcare Authority. 3 Diabetes Management: Directory of Provider Resources PURPOSE The purpose of this directory is to support providers and care teams by identifying resources on the management of type 2 diabetes. It is particularly suited for providers who work with Medicare beneficiaries and vulnerable populations for whom the prevalence of type 2 diabetes and diabetes complications is higher. This directory will help the care team identify resources to improve diabetes management by promoting medication adherence. This directory also aims to equip primary care teams with tools to manage diabetes and that patients with more complex needs are appropriately referred to specialists. While some patients require care from endocrinologists, primary care teams can effectively manage many patients with prediabetes and type 2 diabetes.i Other health professionals and patients can play an important role in facilitating medication management and other diabetes self-care behaviors. -

A Review on Evolution in Triglyceride Determination
Available online at www.derpharmachemica.com ISSN 0975-413X Der Pharma Chemica, 2018, 10(5): 84-88 CODEN (USA): PCHHAX (http://www.derpharmachemica.com/archive.html) Sodium-glucose co-transporter 2 (SGLT2) Inhibitors: New Target for Type 2 Diabetes Mellitus (T2DM) Review Swapna Vadlamani* Asst. proffesor, NIPER, Hyderabad, Andhra Pradesh, India ABSTRACT Introduction: Knocking out type2 diabetes by new insulin independent renal glucose transporters as targets, reducing the side effects related to high rise in glucose levels is a more efficient way to manage diabetes. Sodium-glucose co-transporter 2 (SGLT2) inhibitors block reabsorption of glucose back into the blood and stimulate secretion in urine in a way controlling blood glucose levels. Areas discussed: We emphasize in this review an overview of type 2 diabetes. New insulin independent targets, SGLT family inhibitors and their mechanism of action are briefly discussed. Molecular modeling studies carried out for new analogues of SGLT2 were indicated and also about current marketed SGLT drugs their safety issues are briefly outlined. Conclusion: SGLT2 inhibitors are very promising drugs for near future, where insulin sensitization is a problem. A combination of drugs related to insulin dependent pathway and also independent pathway like SGLT2/SGLT1 drugs will be more effective in glycemic control with lesser side effects. Keywords: Type II Diabetes, SGLT2 inhibitors INTRODUCTION Present scenario of food habits and absolutely very less physical activity is becoming the major cause for obesity finally leading to diabetes. Diabetes is said to be a rich man disease and mostly occurs at the later age of 40, but now one in every 5 persons at early age diagnosed turned to be diabetic mainly because of lifestyle changes. -

Diabetes Medication: Metformin
FACT SHEET FOR PATIENTS AND FAMILIES Diabetes Medication: Metformin What is metformin? Metformin [met-FORE-min] is a medication that is used to treat type 2 diabetes and insulin resistance. Metformin is taken orally (by mouth) as a pill. Like other diabetes medications, it works best when you follow the rest of your treatment plan. This means checking your blood glucose regularly, following your meal plan, and exercising every day. What does it do? Metformin helps lower your blood glucose (blood sugar). It does this by: • Decreasing the amount of glucose released by your Does metformin cause hypoglycemia liver. Less glucose enters your bloodstream. (low blood glucose)? • Increasing the ability of your muscles to use glucose No. Metformin doesn’t cause hypoglycemia by itself. for energy. As more glucose is used, more glucose But combined with other medications, vigorous leaves your bloodstream. exercise, or too little food, it can make your blood glucose drop too low. Why is metformin important for my health? Since low blood glucose can be dangerous, make sure that you and your family know the symptoms. These Metformin can’t cure your diabetes. But, by helping include feeling shaky, sweaty, hungry, and irritable. control your blood glucose, it lowers the chance that If you have these symptoms, take some quick-acting your diabetes will cause serious problems. sugar. Good sources are 3 or 4 glucose tablets, a half- When you have diabetes, you tend to have high blood cup of fruit juice or regular soda, or a tablespoon of glucose. Over time, this can damage your blood honey or sugar. -

Type 2 Diabetes Treatment Recommendations Update
abetes & Di M f e o t a l b a o Cornell, J Diabetes Metab 2014, 5:8 n l r i s u m o DOI: 10.4172/2155-6156.1000414 J Journal of Diabetes and Metabolism ISSN: 2155-6156 Review Article Open Access Type 2 Diabetes Treatment Recommendations Update: Appropriate Use of Dipeptidyl Peptidase-4 Inhibitors Susan Cornell* Midwestern University, Chicago College of Pharmacy, Downers Grove, IL, USA Abstract In this article, recommendations from the 2012 American Diabetes Association (ADA)/European Association for the Study of Diabetes (EASD) position statement are discussed with an emphasis on the appropriate use of Dipeptidyl Peptidase-4 (DPP-4) inhibitors in individuals with Type 2 Diabetes Mellitus (T2DM). The 2012 ADA/EASD position statement emphasizes individualization of treatment, with glycated hemoglobin (A1C) targets being determined for each patient based on life expectancy, complications, disease duration, comorbidities, such as cardiovascular disease or cognitive impairment, and the risk of hypoglycemia and other adverse events. Patients’ attitudes and support systems should also be considered. Recommendations for pharmacotherapy are less prescriptive and should be based on a patient’s needs, preferences, and tolerances. In general, metformin is recommended as first- line therapy for most patients, although combination of 2 noninsulin agents or insulin alone should be considered in patients with baseline A1C ≥ 9.0%. Add-on therapy to metformin will likely be needed to achieve and maintain glycemic control as the disease progresses. It is important to avoid therapies that increase the risk of weight gain or and, especially in older patients, hypoglycemia. As discussed in this review, DPP-4 inhibitors are well tolerated and effectively lower A1C and improve β-cell function without increasing the risk of hypoglycemia and weight gain.