Treatment Patterns, Persistence and Adherence Rates in Patients with Type 2 Diabetes Mellitus in Japan: a Claims- Based Cohort Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Renato Wilberto Zilli Eficácia Em Longo Prazo Das
RENATO WILBERTO ZILLI EFICÁCIA EM LONGO PRAZO DAS GLIFLOZINAS VERSUS GLIPTINAS NO TRATAMENTO DO DIABETES MELLITUS TIPO 2 APÓS FALÊNCIA DA METFORMINA COMO MONOTERAPIA: REVISÃO SISTEMÁTICA E METANÁLISE EM REDE Tese apresentada ao Programa de Ciências Médicas da Faculdade de Medicina da Universidade de São Paulo para obtenção do título de Doutor em Ciências. Área de Concentração: Processos Imunes e Infecciosos Orientador: Prof. Dr. Fabiano Pinheiro da Silva (Versão corrigida. Resolução CoPGr 6018/11, de 13 de outubro de 2011. A versão original está disponível na Biblioteca da FMUSP) São Paulo 2017 Dados Internacionais de Catalogação na Publicação (CIP) Preparada pela Biblioteca da Faculdade de Medicina da Universidade de São Paulo ©reprodução autorizada pelo autor Zilli, Renato Wilberto Eficácia em longo prazo das gliflozinas versus gliptinas no tratamento do diabetes mellitus tipo 2 após falência da metformina como monoterapia : revisão sistemática e metanálise em rede / Renato Wilberto Zilli ‐‐ São Paulo, 2017. Tese(doutorado)--Faculdade de Medicina da Universidade de São Paulo. Programa de Ciências Médicas. Área de concentração: Processos Imunes e Infecciosos. Orientador: Fabiano Pinheiro da Silva. Descritores: 1.Diabetes mellitus tipo 2 2.Metanálise 3.Terapia combinada 4.Falha de tratamento 5.Metformina 6.Inibidores da dipeptidil peptidase IV 7.Transportador 2 de glucose‐sódio/inibidores 8.Empagliflozina 9.Dapagliflozina 10.Saxagliptina USP/FM/DBD ‐302/17 Esta tese de doutorado está de acordo com as seguintes normas, em vigor no momento desta publicação: Referências: adaptado de International Committee of Medical Journals Editors (Vancouver). Guia de apresentação e dissertações, teses e monografias. Elaborado por Anneliese Cordeiro da Cunha, Maria Julia de A.L. -

Effect of Oral Hypoglycaemic Agents on Glucose Tolerance in Pancreatic Diabetes
Gut: first published as 10.1136/gut.13.4.285 on 1 April 1972. Downloaded from Gut, 1972, 13, 285-288 Effect of oral hypoglycaemic agents on glucose tolerance in pancreatic diabetes B. I. JOFFE, W. P. U. JACKSON, S. BANK, AND A. I. VINIK From the Department of Medicine, Witwatersrand University Medical School, Johannesburg, the Gastro- intestinal and Endocrine Research Units of Cape Town University Medical School, and the Chemical Pathology Department of Natal University, South Africa SUMMARY The short-term therapeutic effect of oral hypoglycaemic agents has been assessed in 12 patients with symptomatic diabetes secondary to chronic pancreatitis (pancreatic diabetes). In six patients who had moderate to severe carbohydrate intolerance, associated with severe insulino- paenia during arginine infusion, the potent sulphonylurea chlorpropamide produced no change in the fasting blood glucose level after two weeks of treatment. This contrasted with the significant reduction produced in a matched group of maturity-onset primary diabetics. The six patients with milder diabetes, and a greater (although still subnormal) insulin secretory capacity, showed an improvement in oral glucose tolerance during the first hour following glucose administration while on chlorpropamide. When the biguanide phenformin was substituted for chlorpropamide in five of these patients, a statistically insignificant improvement in glucose tolerance was observed during treatment. Applications of these findings to the practical management of pancreatic diabetes are briefly http://gut.bmj.com/ considered. Chronic pancreatitis is frequently complicated by and two women, ranging from 30 to 67 years of age. diabetes (pancreatic diabetes). Recent studies The diagnosis of pancreatitis was confirmed on the utilizing immunoassay procedures (Joffe, Bank, basis of a gross abnormality in at least two aspects of Jackson, Keller, O'Reilly, and Vinik, 1968; Anderson the pancreatic function test, namely, a low volume of on September 24, 2021 by guest. -

Comparison of Clinical Outcomes and Adverse Events Associated with Glucose-Lowering Drugs in Patients with Type 2 Diabetes: a Meta-Analysis
Online Supplementary Content Palmer SC, Mavridis D, Nicolucci A, et al. Comparison of clinical outcomes and adverse events associated with glucose-lowering drugs in patients with type 2 diabetes: a meta-analysis. JAMA. doi:10.1001/jama.2016.9400. eMethods. Summary of Statistical Analysis eTable 1. Search Strategies eTable 2. Description of Included Clinical Trials Evaluating Drug Classes Given as Monotherapy eTable 3. Description of Included Clinical Trials Evaluating Drug Classes Given as Dual Therapy Added to Metformin eTable 4. Description of Included Clinical Trials Evaluating Drug Classes Given as Triple Therapy When Added to Metformin Plus Sulfonylurea eTable 5. Risks of Bias in Clinical Trials Evaluating Drug Classes Given as Monotherapy eTable 6. Risks of Bias in Clinical Trials Evaluating Drug Classes Given as Dual Therapy Added to Metformin eTable 7. Risks of Bias in Clinical Trials Evaluating Drug Classes Given as Triple Therapy When Added to Metformin plus Sulfonylurea eTable 8. Estimated Global Inconsistency in Networks of Outcomes eTable 9. Estimated Heterogeneity in Networks eTable 10. Definitions of Treatment Failure Outcome eTable 11. Contributions of Direct Evidence to the Networks of Treatments eTable 12. Network Meta-analysis Estimates of Comparative Treatment Associations for Drug Classes Given as Monotherapy eTable 13. Network Meta-analysis Estimates of Comparative Treatment Associations for Drug Classes When Used in Dual Therapy (in Addition to Metformin) eTable 14. Network Meta-analysis Estimates of Comparative Treatment Effects for Drug Classes Given as Triple Therapy eTable 15. Meta-regression Analyses for Drug Classes Given as Monotherapy (Compared With Metformin) eTable 16. Subgroup Analyses of Individual Sulfonylurea Drugs (as Monotherapy) on Hypoglycemia eTable 17. -

Trelagliptin (SYR-472, Zafatek), Novel Once- Weekly Treatment for Type 2 Diabetes, Inhibits Dipeptidyl Peptidase-4 (DPP-4) Via a Non-Covalent Mechanism
RESEARCH ARTICLE Trelagliptin (SYR-472, Zafatek), Novel Once- Weekly Treatment for Type 2 Diabetes, Inhibits Dipeptidyl Peptidase-4 (DPP-4) via a Non-Covalent Mechanism Charles E. Grimshaw1*, Andy Jennings2, Ruhi Kamran1, Hikaru Ueno3, Nobuhiro Nishigaki3, Takuo Kosaka4, Akiyoshi Tani4, Hiroki Sano5, Yoshinobu Kinugawa5, Emiko Koumura5, Lihong Shi1¤, Koji Takeuchi3 a11111 1 Enzymology and Biophysical Chemistry, Takeda California, Inc., San Diego, California, United States of America, 2 Computational Sciences and Crystallography, Takeda California, Inc., San Diego, California, United States of America, 3 Cardiovascular and Metabolic Drug Discovery Unit, Pharmaceutical Research Division, Takeda Pharmaceutical Company Limited, Fujisawa, Kanagawa, Japan, 4 Bio-Molecular Research Laboratories, Pharmaceutical Research Division, Takeda Pharmaceutical Company Limited, Fujisawa, Kanagawa, Japan, 5 Takeda Development Center Japan, Takeda Pharmaceutical Company Limited, Osaka, Japan OPEN ACCESS ¤ Current address: Celgene Quanticel Research, San Diego, California, United States of America * Citation: Grimshaw CE, Jennings A, Kamran R, [email protected] Ueno H, Nishigaki N, Kosaka T, et al. (2016) Trelagliptin (SYR-472, Zafatek), Novel Once-Weekly Treatment for Type 2 Diabetes, Inhibits Dipeptidyl Peptidase-4 (DPP-4) via a Non-Covalent Mechanism. Abstract PLoS ONE 11(6): e0157509. doi:10.1371/journal. Trelagliptin (SYR-472), a novel dipeptidyl peptidase-4 inhibitor, shows sustained efficacy by pone.0157509 once-weekly dosing in type 2 diabetes patients. In this study, we characterized in vitro proper- Editor: Alessandro Giuffrè, National Research ties of trelagliptin, which exhibited approximately 4- and 12-fold more potent inhibition against Council of Italy (CNR), ITALY human dipeptidyl peptidase-4 than alogliptin and sitagliptin, respectively, and >10,000-fold Received: February 10, 2016 selectivity over related proteases including dipeptidyl peptidase-8 and dipeptidyl peptidase-9. -

A Review on Impact of Glucose-Lowering Therapies on Cardiovascular System in Type 2 Diabetes Mellitus Patients
World Journal of Advanced Research and Reviews, 2020, 07(01), 162–173 World Journal of Advanced Research and Reviews e-ISSN: 2581-9615, Cross Ref DOI: 10.30574/wjarr Journal homepage: https://www.wjarr.com (REVIEW ARTICLE) A review on impact of glucose-lowering therapies on cardiovascular system in type 2 diabetes mellitus patients Khatoon Ruquiyyah and Hoda Quaisul * Lloyd Institute of Management and Technology (Pharm), Plot No. 11, Knowledge Park-2, Greater Noida, India. Publication history: Received on 01 July 2020; revised on 10 July 2020; accepted on 12 July 2020 Article DOI: https://doi.org/10.30574/wjarr.2020.7.1.0242 Abstract The prevalence of diabetes mellitus (DM), a well-renowned metabolic diseases that comes under Top-10 lethal and incurable disease of the world, is increasing day by day. It is well-reported that the mortality rate of diabetic patients due to comorbidities is higher. Diabetic patients suffer from several cardiovascular events and such risk increases with an intermediate metabolite HbA1c. Control in HbA1c and lowering it does not appear to yield the same benefit on macrovascular endpoints, as observed for microvascular endpoints. Moreover, secondary diseases caused by diabetes mellitus are many and diabetic patients have been found to be more susceptible to diseases like cardiac injury. For instance, rosiglitazone has been found to cause myocardial infarction and ultimately leads to heart failure. Glucagon like Peptide -1 (GLP-1) agonists and sodium- glucose co-transporter 2 (SGLT2) inhibitors causes several cardiac side effects like myocardial infarction and stroke. In this concern, USFDA officially announced in2008 that all new glucose-lowering agents should be tested for its cardiac safety. -

Risk of Any Hypoglycemia with New Antihyperglycemic Agents in Patients with Type 2 Diabetes: a Systematic Review and Meta-Analysis
Risk of Any Hypoglycemia with New Antihyperglycemic Agents in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis by Sanaz Kamalinia A thesis submitted in conformity with the requirements for the degree of Master of Science Institute of Medical Sciences University of Toronto © Copyright by Sanaz Kamalinia (2019) Risk of Any Hypoglycemia with New Antihyperglycemic Agents in Patients with Type 2 Diabetes: A Systematic Review and Meta- Analysis Sanaz Kamalinia Master of Science Institute of Medical Sciences University of Toronto 2019 Abstract Background : Evaluation of hypoglycemia risk relative to placebo with new antihyperglycemic agents (AHA) including the dipeptidyl peptidase-4 inhibitors (DPP4i), glucagon-like peptide-1 receptor agonists (GLP1RA) and sodium-glucose co-transporter- 2 inhibitors (SGLT2i) remains inconclusive. Objective: This systematic review and meta-analysis aimed to assess risk of any and severe hypoglycemia with new AHA relative to placebo by excluding studies with background sulfonylureas and insulin. Methods: Randomized, placebo-controlled studies, 12 weeks or greater in duration were considered for inclusion. Studies allowing background use of any other AHA, apart from metformin, were excluded. This study is registered with PROSPERO (CRD42018095458). Results: 141 studies included in the meta-analysis demonstrate that relative to placebo, risk of any and severe hypoglycemia did not significantly differ for any new AHA. ii Acknowledgments First and foremost, I wish to express my sincere gratitude to my program advisor committee members. To my supervisor Dr Tobe, thank you for accepting me as your student and presenting me with this challenge. I thoroughly enjoyed it. Especially given your positive words of encouragement and insightful guidance for every step of this journey. -
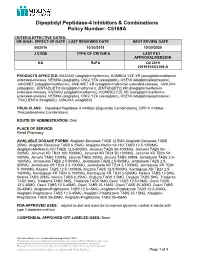
Dipeptidyl Peptidase-4 Inhibitors and Combinations
Dipeptidyl Peptidase-4 Inhibitors & Combinations Policy Number: C5169A CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DATE 06/2016 10/30/2019 10/30/2020 J CODE TYPE OF CRITERIA LAST P&T APPROVAL/VERSION NA RxPA Q4 2019 20191030C5169-A PRODUCTS AFFECTED: KAZANO (alogliptin/metformin), KOMBIGLYZE XR (saxagliptin/metformin extended-release), NESINA (alogliptin), ONGLYZA (saxagliptin), OSENI (alogliptin/pioglitazone), JANUMET (sitagliptin/metformin), JANUMET XR (sitagliptin/metformin extended-release), JANUVIA (sitagliptin), JENTADUETO (linagliptin/metformin), JENTADUETO XR (linagliptin/metformin extended-release), KAZANO (alogliptin/metformin), KOMBIGLYZE XR (saxagliptin/metformin extended-release), NESINA (alogliptin), ONGLYZA (saxagliptin), OSENI (alogliptin/pioglitazone) TRADJENTA (linagliptin), JANUVIA (sitagliptin) DRUG CLASS: Dipeptidyl Peptidase-4 Inhibitor-(Biguanide Combinations), DPP-4 Inhibitor- Thiazolidinedione Combinations ROUTE OF ADMINISTRATION: Oral PLACE OF SERVICE: Retail Pharmacy AVAILABLE DOSAGE FORMS: Alogliptin Benzoate TABS 12.5MG,Alogliptin Benzoate TABS 25MG, Alogliptin Benzoate TABS 6.25MG, Alogliptin-Metformin HCl TABS 12.5-1000MG Alogliptin-Metformin HCl TABS 12.5-500MG, Janumet TABS 50-1000MG, Janumet TABS 50- 500MG, Janumet XR TB24 100-1000MG, Janumet XR TB24 50-1000MG, Janumet XR TB24 50- 500MG, Januvia TABS 100MG, Januvia TABS 25MG, Januvia TABS 50MG, Jentadueto TABS 2.5- 1000MG, Jentadueto TABS 2.5-500MG, Jentadueto TABS 2.5-500MG, Jentadueto TABS 2.5- 850MG, Jentadueto -

Polyhexamethylene Biguanide Hydrochloride) As Used in Cosmetics
Safety Assessment of Polyaminopropyl Biguanide (polyhexamethylene biguanide hydrochloride) as Used in Cosmetics Status: Tentative Report for Public Comment Release Date: September 26, 2017 Panel Date: December 4-5, 2017 All interested persons are provided 60 days from the above date to comment on this safety assessment and to identify additional published data that should be included or provide unpublished data which can be made public and included. Information may be submitted without identifying the source or the trade name of the cosmetic product containing the ingredient. All unpublished data submitted to CIR will be discussed in open meetings, will be available at the CIR office for review by any interested party and may be cited in a peer-reviewed scientific journal. Please submit data, comments, or requests to the CIR Executive Director, Dr. Bart Heldreth. The 2017 Cosmetic Ingredient Review Expert Panel members are: Chair, Wilma F. Bergfeld, M.D., F.A.C.P.; Donald V. Belsito, M.D.; Ronald A. Hill, Ph.D.; Curtis D. Klaassen, Ph.D.; Daniel C. Liebler, Ph.D.; James G. Marks, Jr., M.D.; Ronald C. Shank, Ph.D.; Thomas J. Slaga, Ph.D.; and Paul W. Snyder, D.V.M., Ph.D. The CIR Executive Director is Bart Heldreth, Ph.D. This report was prepared by Wilbur Johnson, Jr., M.S., Senior Scientific Analyst and Ivan Boyer, Ph.D., former Senior Toxicologist. © Cosmetic Ingredient Review 1620 L STREET, NW, SUITE 1200 ◊ WASHINGTON, DC 20036-4702 ◊ PH 202.331.0651 ◊ FAX 202.331.0088 ◊ [email protected] ABSTRACT: The Cosmetic Ingredient Review (CIR) Expert Panel (Panel) reviewed the safety of Polyaminopropyl Biguanide (polyhexamethylene biguanide hydrochloride), which functions as a preservative in cosmetic products. -

Implications Current Drugs for Type 2 Diabetes Mellitus
Pharmacology and therapeutic implications of current drugs for type 2 diabetes mellitus Abd A. Tahrani1,2, Anthony H. Barnett1,2 and Clifford J. Bailey3 Abstract |6[RG|FKCDGVGUOGNNKVWU 6&/ KUCINQDCNGRKFGOKEVJCVRQUGUCOCLQTEJCNNGPIGVQ JGCNVJECTGU[UVGOU+ORTQXKPIOGVCDQNKEEQPVTQNVQCRRTQCEJPQTOCNIN[ECGOKC YJGTG RTCEVKECN ITGCVN[DGPGHKVUNQPIVGTORTQIPQUGUCPFLWUVKHKGUGCTN[GHHGEVKXGUWUVCKPGFCPF UCHGV[EQPUEKQWUKPVGTXGPVKQP+ORTQXGOGPVUKPVJGWPFGTUVCPFKPIQHVJGEQORNGZRCVJQIGPGUKU QH6&/JCXGWPFGTRKPPGFVJGFGXGNQROGPVQHINWEQUGNQYGTKPIVJGTCRKGUYKVJEQORNGOGPVCT[ OGEJCPKUOUQHCEVKQPYJKEJJCXGGZRCPFGFVTGCVOGPVQRVKQPUCPFHCEKNKVCVGFKPFKXKFWCNK\GF OCPCIGOGPVUVTCVGIKGU1XGTVJGRCUVFGECFGUGXGTCNPGYENCUUGUQHINWEQUGNQYGTKPICIGPVU JCXGDGGPNKEGPUGFKPENWFKPIINWECIQPNKMGRGRVKFG|TGEGRVQT ).24 CIQPKUVUFKRGRVKF[N RGRVKFCUG| &22 KPJKDKVQTUCPFUQFKWOINWEQUGEQVTCPURQTVGT| 5).6 KPJKDKVQTU6JGUG CIGPVUECPDGWUGFKPFKXKFWCNN[QTKPEQODKPCVKQPYKVJYGNNGUVCDNKUJGFVTGCVOGPVUUWEJCU DKIWCPKFGUUWNHQP[NWTGCUCPFVJKC\QNKFKPGFKQPGU#NVJQWIJPQXGNCIGPVUJCXGRQVGPVKCN CFXCPVCIGUKPENWFKPINQYTKUMQHJ[RQIN[ECGOKCCPFJGNRYKVJYGKIJVEQPVTQNNQPIVGTOUCHGV[ JCU[GVVQDGGUVCDNKUJGF+PVJKU4GXKGYYGCUUGUUVJGRJCTOCEQMKPGVKEURJCTOCEQF[PCOKEUCPF UCHGV[RTQHKNGUKPENWFKPIECTFKQXCUEWNCTUCHGV[QHEWTTGPVN[CXCKNCDNGVJGTCRKGUHQTOCPCIGOGPV QHJ[RGTIN[ECGOKCKPRCVKGPVUYKVJ6&/YKVJKPVJGEQPVGZVQHFKUGCUGRCVJQIGPGUKUCPFPCVWTCN JKUVQT[+PCFFKVKQPYGDTKGHN[FGUETKDGVTGCVOGPVCNIQTKVJOUHQTRCVKGPVUYKVJ6&/CPFNGUUQPU HTQORTGUGPVVJGTCRKGUVQKPHQTOVJGFGXGNQROGPVQHHWVWTGVJGTCRKGU Type 2 diabetes mellitus (T2DM) is a global epidemic with an dysfunction, as -

Title Long-Term Safety and Efficacy of a Novel Once-Weekly Oral Trelagliptin As Monotherapy Or in Combination with an Existing O
Long-term safety and efficacy of a novel once-weekly oral trelagliptin as monotherapy or in combination with an existing Title oral antidiabetic drug in patients with type 2 diabetes mellitus: A 52-week open-label, phase 3 study Inagaki, Nobuya; Sano, Hiroki; Seki, Yoshifumi; Kuroda, Author(s) Shingo; Kaku, Kohei Citation Journal of Diabetes Investigation (2016), 7(5): 718-726 Issue Date 2016-09 URL http://hdl.handle.net/2433/215204 © 2016 The Authors. Journal of Diabetes Investigation published by Asian Association for the Study of Diabetes (AASD) and John Wiley & Sons Australia, Ltd; This is an open access article under the terms of the Creative Commons Right Attribution-NonCommercial-NoDerivs License, which permits use and distribution in any medium, provided the original work is properly cited, the use is non-commercial and no modifications or adaptations are made. Type Journal Article Textversion publisher Kyoto University CLINICAL TRIAL Long-term safety and efficacy of a novel once- weekly oral trelagliptin as monotherapy or in combination with an existing oral antidiabetic drug in patients with type 2 diabetes mellitus: A 52-week open-label, phase 3 study Nobuya Inagaki1*, Hiroki Sano2,YoshifumiSeki2, Shingo Kuroda2, Kohei Kaku3 1Department of Diabetes, Endocrinology and Nutrition, Kyoto University Graduate School of Medicine, Kyoto, 2Takeda Development Center Japan, Takeda Pharmaceutical Company Limited, Osaka, and 3Department of Internal Medicine, Kawasaki Medical School, Okayama, Japan Keywords ABSTRACT Long-term safety and efficacy, Aims/Introduction: Trelagliptin is a novel once-weekly oral dipeptidyl peptidase-4 inhi- Trelagliptin, Type 2 diabetes mellitus bitor for type 2 diabetes mellitus that was first approved in Japan. -

A Review on Evolution in Triglyceride Determination
Available online at www.derpharmachemica.com ISSN 0975-413X Der Pharma Chemica, 2018, 10(5): 84-88 CODEN (USA): PCHHAX (http://www.derpharmachemica.com/archive.html) Sodium-glucose co-transporter 2 (SGLT2) Inhibitors: New Target for Type 2 Diabetes Mellitus (T2DM) Review Swapna Vadlamani* Asst. proffesor, NIPER, Hyderabad, Andhra Pradesh, India ABSTRACT Introduction: Knocking out type2 diabetes by new insulin independent renal glucose transporters as targets, reducing the side effects related to high rise in glucose levels is a more efficient way to manage diabetes. Sodium-glucose co-transporter 2 (SGLT2) inhibitors block reabsorption of glucose back into the blood and stimulate secretion in urine in a way controlling blood glucose levels. Areas discussed: We emphasize in this review an overview of type 2 diabetes. New insulin independent targets, SGLT family inhibitors and their mechanism of action are briefly discussed. Molecular modeling studies carried out for new analogues of SGLT2 were indicated and also about current marketed SGLT drugs their safety issues are briefly outlined. Conclusion: SGLT2 inhibitors are very promising drugs for near future, where insulin sensitization is a problem. A combination of drugs related to insulin dependent pathway and also independent pathway like SGLT2/SGLT1 drugs will be more effective in glycemic control with lesser side effects. Keywords: Type II Diabetes, SGLT2 inhibitors INTRODUCTION Present scenario of food habits and absolutely very less physical activity is becoming the major cause for obesity finally leading to diabetes. Diabetes is said to be a rich man disease and mostly occurs at the later age of 40, but now one in every 5 persons at early age diagnosed turned to be diabetic mainly because of lifestyle changes. -

Type 2 Diabetes Treatment Recommendations Update
abetes & Di M f e o t a l b a o Cornell, J Diabetes Metab 2014, 5:8 n l r i s u m o DOI: 10.4172/2155-6156.1000414 J Journal of Diabetes and Metabolism ISSN: 2155-6156 Review Article Open Access Type 2 Diabetes Treatment Recommendations Update: Appropriate Use of Dipeptidyl Peptidase-4 Inhibitors Susan Cornell* Midwestern University, Chicago College of Pharmacy, Downers Grove, IL, USA Abstract In this article, recommendations from the 2012 American Diabetes Association (ADA)/European Association for the Study of Diabetes (EASD) position statement are discussed with an emphasis on the appropriate use of Dipeptidyl Peptidase-4 (DPP-4) inhibitors in individuals with Type 2 Diabetes Mellitus (T2DM). The 2012 ADA/EASD position statement emphasizes individualization of treatment, with glycated hemoglobin (A1C) targets being determined for each patient based on life expectancy, complications, disease duration, comorbidities, such as cardiovascular disease or cognitive impairment, and the risk of hypoglycemia and other adverse events. Patients’ attitudes and support systems should also be considered. Recommendations for pharmacotherapy are less prescriptive and should be based on a patient’s needs, preferences, and tolerances. In general, metformin is recommended as first- line therapy for most patients, although combination of 2 noninsulin agents or insulin alone should be considered in patients with baseline A1C ≥ 9.0%. Add-on therapy to metformin will likely be needed to achieve and maintain glycemic control as the disease progresses. It is important to avoid therapies that increase the risk of weight gain or and, especially in older patients, hypoglycemia. As discussed in this review, DPP-4 inhibitors are well tolerated and effectively lower A1C and improve β-cell function without increasing the risk of hypoglycemia and weight gain.