Diabetes Medication: Metformin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Metformin Plus Saxagliptin for Type 2 Diabetes
Treatment evaluation Metformin plus saxagliptin for type 2 diabetes André J. Scheen Division of Diabetes, Nutrition and Metabolic Disorders and Division of Clinical Pharmacology, Department of Medicine, CHU Sart Tilman, University of Liège, Liège, Belgium Running title : Saxagliptin plus metformin Word count : Abstract : 148 Main text : 2404 Tables : 4 Figures : 0 Address for correspondence : Pr André J. SCHEEN Department of Medicine CHU Sart Tilman (B35) B-4000 LIEGE 1 BELGIUM Phone : 32-4-3667238 FAX : 32-4-3667068 Page 1 Email : andre.scheen @ chu.ulg.ac.be SUMMARY Metformin is considered as the first-line drug therapy for the management of type 2 diabetes. Dipeptidyl peptidase-4 (DPP-4) inhibitors, by promoting insulin secretion and reducing glucagon secretion in a glucose-dependent manner, offer new opportunities for oral therapy after failure of metformin. Saxagliptin, a DPP-4 inhibitor, and metformin may be administered together, separately or in fixed-dose combination (FDC), either as saxagliptin added to metformin or as initial combination in drug-naive patients. Both compounds exert complementary pharmacodynamic actions leading to better improvement in blood glucose control (fasting plasma glucose, postprandial glucose, HbA1c) than either compound separately. Adding saxagliptin to metformin monthotherapy results in a consistent, sustained and safe reduction in HbA1c levels. Tolerance is excellent without hypoglycemia or weight gain. The combination saxaglitpin plus metformin may be used as first-line or second-line therapy in the management of type 2 diabetes, especially as a valuable alternative to the classical metformin-sulfonylurea combination. Key-words : DPP-4 inhibitor – Fixed-dose combination - Metformin – Saxagliptin - Type 2 diabetes mellitus Page 2 1. -

CD26/DPP-4: Type 2 Diabetes Drug Target with Potential Influence On
cancers Review CD26/DPP-4: Type 2 Diabetes Drug Target with Potential Influence on Cancer Biology Emi Kawakita 1 , Daisuke Koya 2,3 and Keizo Kanasaki 1,3,* 1 Internal Medicine 1, Shimane University Faculty of Medicine, 89-1 Enya-cho, Izumo 693-8501, Japan; [email protected] 2 Department of Diabetology & Endocrinology, Kanazawa Medical University, Uchinada 920-0293, Japan; [email protected] 3 Division of Anticipatory Molecular Food Science and Technology, Medical Research Institute, Kanazawa Medical University, Uchinada 920-0293, Japan * Correspondence: [email protected]; Tel.: +81-853-20-2183 Simple Summary: Dipeptidyl peptidase (DPP)-4 inhibitor is widely used for type 2 diabetes. Al- though DPP-4/CD26 has been recognized as both a suppressor and inducer in tumor biology due to its various functions, how DPP-4 inhibitor affects cancer progression in diabetic patients is still unknown. The aim of this review is to summarize one unfavorable aspect of DPP-4 inhibitor in cancer-bearing diabetic patients. Abstract: DPP-4/CD26, a membrane-bound glycoprotein, is ubiquitously expressed and has diverse biological functions. Because of its enzymatic action, such as the degradation of incretin hormones, DPP-4/CD26 is recognized as the significant therapeutic target for type 2 diabetes (T2DM); DPP- 4 inhibitors have been used as an anti-diabetic agent for a decade. The safety profile of DPP-4 inhibitors for a cardiovascular event in T2DM patients has been widely analyzed; however, a clear association between DPP-4 inhibitors and tumor biology is not yet established. Previous preclinical Citation: Kawakita, E.; Koya, D.; Kanasaki, K. -

Komboglyze, INN-Saxagliptin, Metformin
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT Komboglyze 2.5 mg/850 mg film-coated tablets Komboglyze 2.5 mg/1,000 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Komboglyze 2.5 mg/850 mg film-coated tablets Each tablet contains 2.5 mg of saxagliptin (as hydrochloride) and 850 mg of metformin hydrochloride. Komboglyze 2.5 mg/1,000 mg film-coated tablets Each tablet contains 2.5 mg of saxagliptin (as hydrochloride) and 1,000 mg of metformin hydrochloride. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet (tablet). Komboglyze 2.5 mg/850 mg film-coated tablets Light brown to brown, biconvex, round, film-coated tablets, with “2.5/850” printed on one side and “4246” printed on the other side, in blue ink. Komboglyze 2.5 mg/1,000 mg film-coated tablets Pale yellow to light yellow, biconvex, oval shaped, film-coated tablets, with “2.5/1000” printed on one side and “4247” printed on the other side, in blue ink. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Komboglyze is indicated in adults with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: in patients inadequately controlled on their maximally tolerated dose of metformin alone in combination with other medicinal products for the treatment of diabetes, including insulin, in patients inadequately controlled with metformin and these medicinal products (see sections 4.4, 4.5 and 5.1 for available data on different combinations) in patients already being treated with the combination of saxagliptin and metformin as separate tablets. -

Management of Hyperglycaemia and Steroid (Glucocorticoid) Therapy
Management of Hyperglycaemia and Steroid (Glucocorticoid) Therapy October 2014 This document is coded JBDS 08 in the series of JBDS documents Other JBDS documents: Admissions avoidance and diabetes: guidance for clinical commissioning groups and clinical team; December 2013, JBDS 07 The management of the hyperosmolar hyperglycaemic state (HHS) in adults with diabetes; August 2012, JBDS 06 Glycaemic management during the inpatient enteral feeding of stroke patients with diabetes; June 2012, JBDS 05 Self-management of diabetes in hospital; March 2012, JBDS 04 Management of adults with diabetes undergoing surgery and elective procedures: improving standards; April 2011, JBDS 03 The Management of Diabetic Ketoacidosis in Adults; revised September 2013, JBDS 02 The hospital management of hypoglycaemia in adults with diabetes mellitus; revised September 2013, JBDS 01 These documents are available to download from: ABCD website: www.diabetologists-abcd.org.uk/JBDS/JBDS.htm Diabetes UK website: www.diabetes.org.uk Contents Page Foreword 4 Authorship and acknowledgments 5-6 Introduction 7 Steroids - mechanism of action 8 Steroid therapy – impact on blood glucose 9 Glucose targets 10 Glucose monitoring 11 Diabetes treatment options 12-13 Treatment of steroid induced hyperglycaemia 14-15 Hospital discharge 16-17 Steroid treatment in pregnancy 18 Steroid treatment in end of life 19 Audit standards 20 Controversial areas 21 References 22 Appendix 1 – Algorithm to show treatment of steroid 23 induced diabetes Appendix 2 – Algorithm to show management of patients 24 with diabetes on once daily steroids Appendix 3 – End of life steroid management 25 Appendix 4 – Patient letter – Glucose monitoring and 26 steroid use 3 Foreword This is the latest in the series of Joint British Diabetes Societies for Inpatient Care (JBDS-IP) guidelines, and focuses on steroid induced hyperglycaemia and steroid induced diabetes. -

Diabetes Medication Reference for Clinicians This Table Provides Clinicians a Brief Overview of Examples of Medications Used to Treat Diabetes
Diabetes Medication Reference for Clinicians This table provides clinicians a brief overview of examples of medications used to treat diabetes. This is not a complete list and is not intended to be used as a sole reference. Nursing responsibilities with ALL diabetes medications: Emphasize importance of self-monitoring of blood glucose (SMBG); teach to be aware of signs/symptoms of allergic reactions; teach to be aware of possible side effects and contraindications; and monitor A1C levels. Oral Medication Action Possible Side-effects Contraindications Nursing Responsibilities Biguanide • Lowers glucose levels • Anorexia, nausea, • Renal disease Patient education: • metformin by decreasing the vomiting, diarrhea - • Liver failure or • Take with food (Glucophage, amount of glucose usually occurs during alcohol abuse (can • Keep appointments Glucophage XR, produced by the liver initiation of the drug result in lactic for regular kidney Glumetza, Fortamet, • Increases glucose • Vitamin B-12 acidosis) function lab tests Riomet) uptake in muscle deficiency • Temporarily held on • Avoid alcohol • Multiple combinations cells • Lactic acidosis day of procedures • Report abnormal with other classes • Improves (severe but rare) with dye and glucose levels • First line therapy for hyperglycemia & • Should not cause withheld 48 hours • Report s/s lactic type 2 diabetes; hypertriglyceridemia hypoglycemia as after the procedure; acidosis (weakness, current in obese patients monotherapy restart after drowsiness, malaise) recommendation is to with diabetes; may confirmation of renal start upon diagnosis promote weight loss function This material was prepared by Quality Insights, the Medicare Quality Innovation Network-Quality Improvement Organization supporting the Home Health Quality Improvement National 1 Campaign, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. -

AVANDIA (Rosiglitazone Maleate Tablets), for Oral Use Ischemic Cardiovascular (CV) Events Relative to Placebo, Not Confirmed in Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION ----------------------- WARNINGS AND PRECAUTIONS ----------------------- These highlights do not include all the information needed to use • Fluid retention, which may exacerbate or lead to heart failure, may occur. AVANDIA safely and effectively. See full prescribing information for Combination use with insulin and use in congestive heart failure NYHA AVANDIA. Class I and II may increase risk of other cardiovascular effects. (5.1) • Meta-analysis of 52 mostly short-term trials suggested a potential risk of AVANDIA (rosiglitazone maleate tablets), for oral use ischemic cardiovascular (CV) events relative to placebo, not confirmed in Initial U.S. Approval: 1999 a long-term CV outcome trial versus metformin or sulfonylurea. (5.2) • Dose-related edema (5.3) and weight gain (5.4) may occur. WARNING: CONGESTIVE HEART FAILURE • Measure liver enzymes prior to initiation and periodically thereafter. Do See full prescribing information for complete boxed warning. not initiate therapy in patients with increased baseline liver enzyme levels ● Thiazolidinediones, including rosiglitazone, cause or exacerbate (ALT >2.5X upper limit of normal). Discontinue therapy if ALT levels congestive heart failure in some patients (5.1). After initiation of remain >3X the upper limit of normal or if jaundice is observed. (5.5) AVANDIA, and after dose increases, observe patients carefully for signs • Macular edema has been reported. (5.6) and symptoms of heart failure (including excessive, rapid weight gain; • Increased incidence of bone fracture was observed in long-term trials. dyspnea; and/or edema). If these signs and symptoms develop, the heart (5.7) failure should be managed according to current standards of care. -

What You Need to Know: Centers for Medicare & Medicaid Services Part D Measure — Statin Use in Persons with Diabetes
T:8.5” What You Need to Know: Centers for Medicare & Medicaid Services Part D Measure — Statin Use in Persons With Diabetes UnitedHealthcare recognizes the time and effort you put into managing the health of your patients with diabetes. To help you be as efficient as possible, we’re offering this guide with detailed information about the Statin Use in Persons With Diabetes (SUPD) Part D measure from the Centers for Medicare & Medicaid Services (CMS). Defining the SUPD measure CMS defines this measure as the percentage of Medicare members with diabetes ages 40–75 who receive at least one fill of a statin medication in the measurement year. Members with diabetes are defined as those who have at least two fills of diabetes medications during the measurement year. Only pharmacy claims are used to identify and close care opportunities for this measure. Members who have end-stage renal disease (ESRD) and/or are in hospice care are excluded from the SUPD measure. Understanding measure rationale The SUPD measure is based on cholesterol guidelines from the American College of Cardiology/American Heart T:11” Association (ACC/AHA). The guidelines recommend moderate- to high-intensity statin therapy for patients ages 40–75 with diabetes to help prevent atherosclerotic cardiovascular disease (ASCVD).1,2 The guidelines: • Recognize patients ages 40–75 with diabetes are at a substantially higher lifetime risk for ASCVD events and experience greater morbidity and worse survival rates following the start of clinical ASCVD. • Indicate statins have been shown to be effective in reducing the risk for cardiovascular events. • Align with the American Diabetes Association in recommending statin therapy for patients ages 40–75 with diabetes to help prevent ASCVD.3 Reaching the SUPD target goal To successfully meet CMS requirements, men and women who fit the measure definition must be on a statin medication for the prevention of ASCVD, if clinically appropriate. -

Type 2 Diabetes Adult Outpatient Insulin Guidelines
Diabetes Coalition of California TYPE 2 DIABETES ADULT OUTPATIENT INSULIN GUIDELINES GENERAL RECOMMENDATIONS Start insulin if A1C and glucose levels are above goal despite optimal use of other diabetes 6,7,8 medications. (Consider insulin as initial therapy if A1C very high, such as > 10.0%) 6,7,8 Start with BASAL INSULIN for most patients 1,6 Consider the following goals ADA A1C Goals: A1C < 7.0 for most patients A1C > 7.0 (consider 7.0-7.9) for higher risk patients 1. History of severe hypoglycemia 2. Multiple co-morbid conditions 3. Long standing diabetes 4. Limited life expectancy 5. Advanced complications or 6. Difficult to control despite use of insulin ADA Glucose Goals*: Fasting and premeal glucose < 130 Peak post-meal glucose (1-2 hours after meal) < 180 Difference between premeal and post-meal glucose < 50 *for higher risk patients individualize glucose goals in order to avoid hypoglycemia BASAL INSULIN Intermediate-acting: NPH Note: NPH insulin has elevated risk of hypoglycemia so use with extra caution6,8,15,17,25,32 Long-acting: Glargine (Lantus®) Detemir (Levemir®) 6,7,8 Basal insulin is best starting insulin choice for most patients (if fasting glucose above goal). 6,7 8 Start one of the intermediate-acting or long-acting insulins listed above. Start insulin at night. When starting basal insulin: Continue secretagogues. Continue metformin. 7,8,20,29 Note: if NPH causes nocturnal hypoglycemia, consider switching NPH to long-acting insulin. 17,25,32 STARTING DOSE: Start dose: 10 units6,7,8,11,12,13,14,16,19,20,21,22,25 Consider using a lower starting dose (such as 0.1 units/kg/day32) especially if 17,19 patient is thin or has a fasting glucose only minimally above goal. -
Taking Metformin for Gestational Diabetes This Information Sheet Will Help You Understand More About Taking Metformin for Gestational Diabetes
Taking metformin for gestational diabetes This information sheet will help you understand more about taking metformin for gestational diabetes. This information sheet is not a substitute for talking with your midwife, doctor, nurse or pharmacist. Gestational diabetes Risks for your baby: Gestational diabetes means you have too much • may grow larger than normal (this increases the glucose (a type of sugar) in your blood when you risk of injury during birth) are pregnant. Insulin controls the amount of • born too early (premature) glucose in your blood. Sometimes you don’t make • low blood glucose after birth enough insulin or it doesn’t work as well when you are pregnant. • may need treatment in hospital • jaundice (yellow skin) that needs treatment Gestational diabetes is common. Up to eight pregnant women in every 100 get gestational • breathing problems. diabetes. Taking metformin helps reduce these risks. It can be hard to tell if you have gestational You can see how many women and babies are diabetes. Some women find that they: affected and how treatment helps in the picture • lack energy on the next page. • feel thirsty a lot • go to the toilet a lot Metformin is safe to take for • get lots of infections. gestational diabetes Metformin has been tested in clinical studies and Some women have no symptoms. This is why all is safe to take for gestational diabetes. pregnant women are tested for diabetes so they Metformin helps keep both your weight gain and can get treatment. blood pressure down. Metformin The main side effect is stomach upsets such as Metformin is a medicine that has been used feeling sick and diarrhoea. -
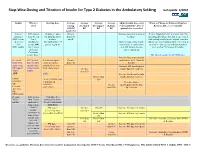
Step-Wise Dosing and Titration of Insulin for Type 2 Diabetes in the Ambulatory Setting Last Update 5/2010
Step -Wise Dosing and Titration of Insulin for Type 2 Diabetes in the Ambulatory Setting last update 5/2010 Insulin When to Starting dose Average Average Average Average Adjust Insulin dose every When to Change to Different Regimen start fasting Pre-lunch Pre-supper Bedtime 3 days until BG < 130, or Recheck A1C every 3 months AM BG BG BG BG optimal dose is reached Goal<130 Lantus A1C greater 10 units or up to Greater Increase dose by 2-4 units at If after 3 months if A1c is greater than 7% (glargine) than 8% on 0.2 units/kg SQ at than 130 bedtime. and optimal bedtime dose has been reached OR Levemir 2 or 3 bedtime mg/dL with fasting blood glucose at goal, consider (detemir) antidiabetic (DC sulfonylurea if Optimal long acting (basal) adding a pre-meal bolus insulin at the largest OR agents OR part of regimen) insulin dose keeps bedtime meal of the day, pre-meal bolus insulin at NPH insulin 1 or 2 agents and AM fasting glucose each meal or 70/30 premix insulin. if Serum values consistent. Creatinine greater than 2 DC all oral agents except Metformin. Increase long acting (basal) Pre-meal A1C greater 2-4 units of rapid Greater insulin dose by 2-4 units at bolus with than 7% with acting or regular than 130 bedtime rapid acting optimal long insulin SQ at each Increase AM rapid/regular OR regular acting (basal) meal (base dose) Greater insulin dose by 2-4 units. insulin insulin. than 130 AND with Increase lunch rapid/regular Greater than insulin dose by 2-4 units. -

KOMBIGLYZE XR Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION ------------------------WARNINGS AND PRECAUTIONS----------------------- These highlights do not include all the information needed to use Lactic acidosis: Warn patients against excessive alcohol intake. KOMBIGLYZE XR safely and effectively. See full prescribing KOMBIGLYZE XR not recommended in hepatic impairment and information for KOMBIGLYZE XR. contraindicated in renal impairment. Ensure normal renal function KOMBIGLYZE XR (saxagliptin and metformin HCl extended-release) before initiating and at least annually thereafter. Temporarily tablets discontinue KOMBIGLYZE XR in patients undergoing radiologic Initial U.S. Approval: 2010 studies with intravascular administration of iodinated contrast materials or any surgical procedures necessitating restricted intake of food and WARNING: LACTIC ACIDOSIS fluids. (4, 5.1, 5.3, 5.4, 5.7, 5.10, 5.11) See full prescribing information for complete boxed warning. There have been postmarketing reports of acute pancreatitis in patients Lactic acidosis can occur due to metformin accumulation. The taking saxagliptin. If pancreatitis is suspected, promptly discontinue risk increases with conditions such as sepsis, dehydration, excess KOMBIGLYZE XR. (5.2) alcohol intake, hepatic impairment, renal impairment, and acute Vitamin B12 deficiency: Metformin may lower vitamin B12 levels. congestive heart failure. (5.1) Measure hematological parameters annually. (5.5, 6.1) Symptoms include malaise, myalgias, respiratory distress, Hypoglycemia: When used with an insulin -

Antidepressant Prescription Practices Among Primary Health Care Providers for Patients with Diabetes Mellitus
Research Article Curre Res Diabetes & Obes J Volume 2 Issue 4 - June 2017 Copyright © All rights are reserved by Gillian Bartlet DOI: 10.19080/CRDOJ.2017.2.555593 Antidepressant Prescription Practices among Primary Health Care Providers for Patients with Diabetes Mellitus Gagnon J, Lussier MT, Daskalopoulou SS, MacGibbon B, Bartlett G 1Department of Family Medicine, McGill University, Canada 2Department of Family Medicine and Emergency Medicine, Université de Montréal, Canada 3Department of Medicine, McGill University, Canada 4Department of Mathematics, Université du Québec à Montréal, Canada 5Department of Family Medicine, McGill University, Canada Submission: June 13, 2017; Published: June 27, 2017 *Corresponding author: Gillian Bartlett, Department of Family Medicine, McGill University, Canada, Tel: ; Fax: ; Email: Abstract Purpose: Depression is a common comorbidity in people with diabetes that increases the risk of poor diabetes control and diabetes- related complications. While treatment of depression is expected to help, some antidepressants have been associated with impaired glucose metabolism. Evidence is lacking in the scope of this problem for people with diabetes. The objective of this study is to describe the prescription of antidepressants for diabetic patients with a focus on medications suspected to impair glucose control. Methods: A cross-sectional study of electronic medical record data from 115 primary care practices in the Canadian Primary Care Sentinel Surveillance Network was conducted. Descriptive statistics were used to describe the prescription of antidepressants for people with diabetes between 2009 and 2014. Results: From the sample, 17,258 diabetic patients were prescribed at least one antidepressant (AD) between 2009 and 2014. In terms of pharmacological class, the greatest proportion of people were prescribed selective serotonin reuptake inhibitors (46.2%), followed by serotonin-norepinephrine reuptake inhibitors (24.3%) and tricyclic antidepressants (23.8%).