Metformin History Diabetologia Bailey 2017 V3 R1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Metformin Selectively Targets Redox Control of Complex I Energy Transduction
Heriot-Watt University Research Gateway Metformin selectively targets redox control of complex I energy transduction Citation for published version: Cameron, AR, Logie, L, Patel, K, Erhardt, S, Bacon, S, Middleton, P, Harthill, J, Forteath, C, Coats, JT, Kerr, C, Curry, H, Stewart, D, Sakamoto, K, Repišák, P, Paterson, MJ, Hassinen, I, McDougall, GJ & Rena, G 2018, 'Metformin selectively targets redox control of complex I energy transduction', Redox Biology, vol. 14, pp. 187-197. https://doi.org/10.1016/j.redox.2017.08.018 Digital Object Identifier (DOI): 10.1016/j.redox.2017.08.018 Link: Link to publication record in Heriot-Watt Research Portal Document Version: Publisher's PDF, also known as Version of record Published In: Redox Biology General rights Copyright for the publications made accessible via Heriot-Watt Research Portal is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy Heriot-Watt University has made every reasonable effort to ensure that the content in Heriot-Watt Research Portal complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 24. Sep. 2021 Redox Biology 14 (2018) 187–197 Contents lists available at ScienceDirect Redox Biology journal homepage: www.elsevier.com/locate/redox Research paper Metformin selectively targets redox control of complex I energy transduction MARK Amy R. -

The Importance of Synthetic Drugs for Type 2 Diabetes Drug Discovery
Review The importance of synthetic drugs for type 2 diabetes drug discovery † Maliheh Safavi, Alireza Foroumadi & Mohammad Abdollahi † 1. Introduction Tehran University of Medical Sciences, Faculty of Pharmacy and Pharmaceutical Sciences Research Center, Tehran, Iran 2. Pathophysiology of T2DM 3. Overview of current synthetic Introduction: Type 2 diabetes mellitus (T2DM) is a major metabolic, drugs in the treatment of multi-causal and heterogeneous disorder which causes significant morbid- T2DM ity and mortality with considerable burden to healthcare resources. The 4. New synthetic compounds as number of deaths due to T2DM highlights the insufficiency of the cur- DPP-4 inhibitors rently available drugs for controlling the disease and its complications and more needs to be done. 5. New synthetic compounds as Areas covered: SGLT2 inhibitors This paper reviews the updated pathobiology of T2DM that should be targeted in drug discovery. Further, the article provides discussion 7. Conclusion on the mechanism of action, side effects and structure of the currently avail- 8. Expert opinion able synthetic drugs. The authors specifically evaluate two newer classes of anti-diabetic agents: dipeptidyl peptidase IV (DPP-4) and sodium-glucose transporter-2 (SGLT2). They also present information on newer synthetic com- pounds. The article also highlights the key interactions between synthetic compounds and DPP-4 active site residues for rational drug design. Expert opinion: Numerous anti-hyperglycaemic drugs are currently available but many are limited by their adverse effects. The identification of the 3D structure of DPP-4 has opened new avenues for design, thus aiming to pro- duce drugs that directly exploit the structural characteristics of this binding site. -

Use of Metformin in the Setting of Mild-To-Moderate Renal Insufficiency
Reviews/Commentaries/ADA Statements REVIEW Use of Metformin in the Setting of Mild-to-Moderate Renal Insufficiency 1 KASIA J. LIPSKA, MD hepatic gluconeogenesis without raising 2 CLIFFORD J. BAILEY, PHD, FRCP fi 3 insulin levels, it rarely leads to signi cant SILVIO E. INZUCCHI, MD hypoglycemia when used as a monother- apy (8,11). As a result, metformin is widely considered an ideal first-line agent for the treatment of type 2 diabetes, as common clinical conundrum faces despite multiple trials of intensive glu- recommended by several clinical guide- all U.S. practitioners treating pa- cose control using a variety of glucose- lines (12–14). A fi tients with type 2 diabetes. Today’s lowering strategies, there is a paucity of In addition to such bene ts, metfor- U.S. Food and Drug Administration pre- data to support specificadvantageswith min reduces the risk of developing di- scribing guidelines for metformin contra- other agents on cardiovascular outcomes abetes in individuals at high risk for the indicate its use in men and women with (5–7). disease (15) and has been considered as a serum creatinine concentrations $1.5 In the original UK Prospective Di- reasonable “off-label” approach in se- and $1.4 mg/dL ($132 and $123 abetes Study (UKPDS), 342 overweight lected individuals for diabetes prevention mmol/L), respectively. In a patient toler- patients with newly diagnosed diabetes (16). ating and controlled with this medication, were randomly assigned to metformin should it automatically be discontinued therapy (8). After a median period of 10 — as the creatinine rises beyond these cut years, this subgroup experienced a 39% HISTORICAL PERSPECTIVE De- fi points over time? Stopping metformin of- (P = 0.010) risk reduction for myocardial spite these proven bene ts, metformin ten results in poorly controlled glycemia infarction and a 36% reduction for total remains contraindicated in a large seg- and/or the need for other agents with their mortality (P = 0.011) compared with con- ment of the type 2 diabetic population, own adverse-effect profiles. -
Treatment Patterns, Persistence and Adherence Rates in Patients with Type 2 Diabetes Mellitus in Japan: a Claims- Based Cohort Study
Open access Research BMJ Open: first published as 10.1136/bmjopen-2018-025806 on 1 March 2019. Downloaded from Treatment patterns, persistence and adherence rates in patients with type 2 diabetes mellitus in Japan: a claims- based cohort study Rimei Nishimura,1 Haruka Kato,2 Koichi Kisanuki,2 Akinori Oh,2 Shinzo Hiroi,2 Yoshie Onishi,3 Florent Guelfucci,4 Yukio Shimasaki2 To cite: Nishimura R, Kato H, ABSTRACT Strengths and limitations of this study Kisanuki K, et al. Treatment Objective To determine real-world trends in antidiabetic patterns, persistence and drug use, and persistence and adherence, in Japanese ► This retrospective evaluation of administrative adherence rates in patients patients with type 2 diabetes mellitus (T2DM). with type 2 diabetes mellitus claims data (2011–2015) using the Japan Medical Design Retrospective evaluation of administrative claims in Japan: a claims-based Data Center (JMDC) and Medical Data Vision (MDV) data (2011–2015) using the Japan Medical Data Center cohort study. BMJ Open databases was conducted to determine real-world (JMDC) and Medical Data Vision (MDV) databases. 2019;9:e025806. doi:10.1136/ trends in antidiabetic drug use, and persistence and Setting Analysis of two administrative claims databases bmjopen-2018-025806 adherence, in Japanese patients with type 2 dia- for Japanese patients with T2DM. betes mellitus (T2DM); 40 908 and 90 421 patients ► Prepublication history and Participants Adults (aged ≥18 years) with an International additional material for this were included from the JMDC and MDV databases, Classification of Diseases, 10th Revision code of T2DM and paper are available online. To respectively. at least one antidiabetic drug prescription. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

The Na+/Glucose Co-Transporter Inhibitor Canagliflozin Activates AMP-Activated Protein Kinase by Inhibiting Mitochondrial Function and Increasing Cellular AMP Levels
Page 1 of 37 Diabetes Hawley et al Canagliflozin activates AMPK 1 The Na+/glucose co-transporter inhibitor canagliflozin activates AMP-activated protein kinase by inhibiting mitochondrial function and increasing cellular AMP levels Simon A. Hawley1†, Rebecca J. Ford2†, Brennan K. Smith2, Graeme J. Gowans1, Sarah J. Mancini3, Ryan D. Pitt2, Emily A. Day2, Ian P. Salt3, Gregory R. Steinberg2†† and D. Grahame Hardie1†† 1Division of Cell Signalling & Immunology, School of Life Sciences, University of Dundee, Dundee, Scotland, UK 2Division of Endocrinology and Metabolism, Department of Medicine, McMaster University, Hamilton, Ontario, Canada 3Institute of Cardiovascular and Medical Sciences, College of Medical, Veterinary & Life Sciences, University of Glasgow, Glasgow, Scotland, UK Running title: Canagliflozin activates AMPK Corresponding authors: Dr. D. G. Hardie, Division of Cell Signalling & Immunology, School of Life Sciences, University of Dundee, Dow Street, Dundee, DD1 5EH, Scotland, UK; Dr. G.R. Steinberg, Division of Endocrinology and Metabolism, Department of Medicine, McMaster University, Hamilton, Ontario, Canada Tel: +44 (1382) 384253; FAX: +44 (1382) 385507; e-mail: [email protected] Tel: +1 (905) 525-9140 ext.21691; email: [email protected] Word count in main text: 3,996 Number of Figures: 7 †these authors made equal contributions to this study ††joint corresponding authors Diabetes Publish Ahead of Print, published online July 5, 2016 Diabetes Page 2 of 37 Hawley et al Canagliflozin activates AMPK 2 ABSTRACT Canagliflozin, dapagliflozin and empagliflozin, all recently approved for treatment of Type 2 diabetes, were derived from the natural product phlorizin. They reduce hyperglycemia by inhibiting glucose re- uptake by SGLT2 in the kidney, without affecting intestinal glucose uptake by SGLT1. -

Valsartan in Combination with Metformin and Gliclazide in Diabetic
Patra et al. Future Journal of Pharmaceutical Sciences (2021) 7:157 Future Journal of https://doi.org/10.1186/s43094-021-00307-2 Pharmaceutical Sciences RESEARCH Open Access Valsartan in combination with metformin and gliclazide in diabetic rat model using developed RP-HPLC method Rasmita Patra, Yedukondalu Kollati, Sampath Kumar NS and Vijaya R. Dirisala* Abstract Background: Oral administration of biguanides (metformin) and sulfonylureas (gliclazide) are the most common approach of management of type 2 diabetes in humans. Among these diabetic patients, approximately 40–60% suffers from hypertension. Hence, the need of the day is application of polytherapy. A major challenge in polytherapy is the drug-drug interactions that may arise. Hence, this study is focused to develop a reverse phase high-performance liquid chromatography (RP-HPLC) method for concurrent estimation of diabetic drug metformin and hypertension drug valsartan using C18 column and find any possible pharmacokinetic interactions between the two drug combinations strategies, i.e., metformin-valsartan and gliclazide-valsartan in streptozotocin-induced diabetic rats. Result: The bioanalysis of drug-drug interaction pharmacokinetic result showed no significant difference in the tmax of single treatment of gliclazide and single treatment of metformin or upon co-administration with valsartan. Conclusion: Our study has shown that polytherapy of valsartan, a drug administered for hypertension along with hypoglycemic drugs metformin and gliclazide, can be advantageous and safe in patients suffering from both diabetes and hypertension. Keywords: RP-HPLC, Metformin, Valsartan, Gliclazide, Hypertension, Diabetes mellitus Background disease if left undetected or untreated. Such patients re- Diabetes has become a growing epidemic, and the per- quire polytherapy wherein drug-drug interactions may centage of patient population is increasing in leaps and lead to adverse side effects [5, 6]. -

Effect of Oral Hypoglycaemic Agents on Glucose Tolerance in Pancreatic Diabetes
Gut: first published as 10.1136/gut.13.4.285 on 1 April 1972. Downloaded from Gut, 1972, 13, 285-288 Effect of oral hypoglycaemic agents on glucose tolerance in pancreatic diabetes B. I. JOFFE, W. P. U. JACKSON, S. BANK, AND A. I. VINIK From the Department of Medicine, Witwatersrand University Medical School, Johannesburg, the Gastro- intestinal and Endocrine Research Units of Cape Town University Medical School, and the Chemical Pathology Department of Natal University, South Africa SUMMARY The short-term therapeutic effect of oral hypoglycaemic agents has been assessed in 12 patients with symptomatic diabetes secondary to chronic pancreatitis (pancreatic diabetes). In six patients who had moderate to severe carbohydrate intolerance, associated with severe insulino- paenia during arginine infusion, the potent sulphonylurea chlorpropamide produced no change in the fasting blood glucose level after two weeks of treatment. This contrasted with the significant reduction produced in a matched group of maturity-onset primary diabetics. The six patients with milder diabetes, and a greater (although still subnormal) insulin secretory capacity, showed an improvement in oral glucose tolerance during the first hour following glucose administration while on chlorpropamide. When the biguanide phenformin was substituted for chlorpropamide in five of these patients, a statistically insignificant improvement in glucose tolerance was observed during treatment. Applications of these findings to the practical management of pancreatic diabetes are briefly http://gut.bmj.com/ considered. Chronic pancreatitis is frequently complicated by and two women, ranging from 30 to 67 years of age. diabetes (pancreatic diabetes). Recent studies The diagnosis of pancreatitis was confirmed on the utilizing immunoassay procedures (Joffe, Bank, basis of a gross abnormality in at least two aspects of Jackson, Keller, O'Reilly, and Vinik, 1968; Anderson the pancreatic function test, namely, a low volume of on September 24, 2021 by guest. -
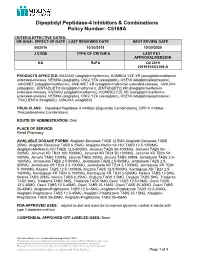
Dipeptidyl Peptidase-4 Inhibitors and Combinations
Dipeptidyl Peptidase-4 Inhibitors & Combinations Policy Number: C5169A CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DATE 06/2016 10/30/2019 10/30/2020 J CODE TYPE OF CRITERIA LAST P&T APPROVAL/VERSION NA RxPA Q4 2019 20191030C5169-A PRODUCTS AFFECTED: KAZANO (alogliptin/metformin), KOMBIGLYZE XR (saxagliptin/metformin extended-release), NESINA (alogliptin), ONGLYZA (saxagliptin), OSENI (alogliptin/pioglitazone), JANUMET (sitagliptin/metformin), JANUMET XR (sitagliptin/metformin extended-release), JANUVIA (sitagliptin), JENTADUETO (linagliptin/metformin), JENTADUETO XR (linagliptin/metformin extended-release), KAZANO (alogliptin/metformin), KOMBIGLYZE XR (saxagliptin/metformin extended-release), NESINA (alogliptin), ONGLYZA (saxagliptin), OSENI (alogliptin/pioglitazone) TRADJENTA (linagliptin), JANUVIA (sitagliptin) DRUG CLASS: Dipeptidyl Peptidase-4 Inhibitor-(Biguanide Combinations), DPP-4 Inhibitor- Thiazolidinedione Combinations ROUTE OF ADMINISTRATION: Oral PLACE OF SERVICE: Retail Pharmacy AVAILABLE DOSAGE FORMS: Alogliptin Benzoate TABS 12.5MG,Alogliptin Benzoate TABS 25MG, Alogliptin Benzoate TABS 6.25MG, Alogliptin-Metformin HCl TABS 12.5-1000MG Alogliptin-Metformin HCl TABS 12.5-500MG, Janumet TABS 50-1000MG, Janumet TABS 50- 500MG, Janumet XR TB24 100-1000MG, Janumet XR TB24 50-1000MG, Janumet XR TB24 50- 500MG, Januvia TABS 100MG, Januvia TABS 25MG, Januvia TABS 50MG, Jentadueto TABS 2.5- 1000MG, Jentadueto TABS 2.5-500MG, Jentadueto TABS 2.5-500MG, Jentadueto TABS 2.5- 850MG, Jentadueto -

Switch from Insulin Therapy to Intensive Combination Therapy with Pioglitazone and Other Oral Hypoglycemic Agents in Patients with Type 2 Diabetes
20 (696) 診療と新薬・第 52 巻 第7号(2015 年7月) SWITCH FROM INSULIN THERAPY TO INTENSIVE COMBINATION THERAPY WITH PIOGLITAZONE AND OTHER ORAL HYPOGLYCEMIC AGENTS IN PATIENTS WITH TYPE 2 DIABETES Masazumi FUJIWARA Department of Diabetes Medicine, Saijo Central Hospital, Ehime, Japan Abstract Aim: Insulin therapy is considered the final option for patients with progressive type 2 diabetes. This study investigated, whether reconverting patients from insulin therapy to oral medicine using thiazolidinedione pioglitazone is possible without further deterioration of glycemic control. Methods: One hundred sixty subjects (112 male and 48 female) aged 61.4 ± 13.8 years with an mean insulin dose of 28.3 ± 18.7 U/day, mainly using preprandial bolus dose of rapid- acting or ultra-rapid-acting insulin preparations, a duration of insulin therapy of 3.1 ± 1.0 years and an average hemoglobin A1c (A1c) of 9.9 ± 1.8% were switched from insulin therapy to combination therapy with pioglitazone and other oral hypoglycemic agents (biguanide, a-glucosidase inhibitor, and glinide). Results: During the observation period (3.2 ± 1.3 months), 113 patients (70.6%) treated with insulin injections (24.8 ± 14.3 U/day), could be successfully switched from insulin therapy to pioglitazone-based oral combination therapy. Their mean A1c significant decreased from 9.9 ± 2.0 to 6.2 ± 0.5%, and all patients could achieve A1c < 7.0%. Although the remaining 47 patients (29.4%) could not be successfully switched, their A1c significant decreased from 10.1 ± 1.47 to 7.4 ± 0.8% and their mean insulin dose significantly decreased from 36.7 ± 24.6 to 6.8 ± 10.1 U/day. -

Polyhexamethylene Biguanide Hydrochloride) As Used in Cosmetics
Safety Assessment of Polyaminopropyl Biguanide (polyhexamethylene biguanide hydrochloride) as Used in Cosmetics Status: Tentative Report for Public Comment Release Date: September 26, 2017 Panel Date: December 4-5, 2017 All interested persons are provided 60 days from the above date to comment on this safety assessment and to identify additional published data that should be included or provide unpublished data which can be made public and included. Information may be submitted without identifying the source or the trade name of the cosmetic product containing the ingredient. All unpublished data submitted to CIR will be discussed in open meetings, will be available at the CIR office for review by any interested party and may be cited in a peer-reviewed scientific journal. Please submit data, comments, or requests to the CIR Executive Director, Dr. Bart Heldreth. The 2017 Cosmetic Ingredient Review Expert Panel members are: Chair, Wilma F. Bergfeld, M.D., F.A.C.P.; Donald V. Belsito, M.D.; Ronald A. Hill, Ph.D.; Curtis D. Klaassen, Ph.D.; Daniel C. Liebler, Ph.D.; James G. Marks, Jr., M.D.; Ronald C. Shank, Ph.D.; Thomas J. Slaga, Ph.D.; and Paul W. Snyder, D.V.M., Ph.D. The CIR Executive Director is Bart Heldreth, Ph.D. This report was prepared by Wilbur Johnson, Jr., M.S., Senior Scientific Analyst and Ivan Boyer, Ph.D., former Senior Toxicologist. © Cosmetic Ingredient Review 1620 L STREET, NW, SUITE 1200 ◊ WASHINGTON, DC 20036-4702 ◊ PH 202.331.0651 ◊ FAX 202.331.0088 ◊ [email protected] ABSTRACT: The Cosmetic Ingredient Review (CIR) Expert Panel (Panel) reviewed the safety of Polyaminopropyl Biguanide (polyhexamethylene biguanide hydrochloride), which functions as a preservative in cosmetic products. -

Objectives Anti-Hyperglycemic Therapeutics
9/22/2015 Some Newer Non-Insulin Therapies for Type 2 Diabetes:Present and future Faculty/presenter disclosure Speaker’s name: Dr. Robert G. Josse SGLT2 Inhibitors Grants/research support: Astra Zeneca, BMS, Boehringer Dopamine D2 Receptor Agonist Ingelheim, Eli Lilly, Janssen, Merck, NovoNordisk, Roche, Bile acid sequestrant sanofi, Consulting Fees: Astra Zeneca, BMS, Eli Lilly, Janssen, Merck, Dr Robert G Josse Division of Endocrinology & Metabolism Speakers bureau: Janssen, Astra Zeneca, BMS, Merck, St. Michael’s Hospital Professor of Medicine Stocks and Shares:None University of Toronto 100-year History of Objectives Anti-hyperglycemic Therapeutics 14 Discuss the mechanism of action of SGLT2 inhibitors, SGLT-2 inhibitor 12 Bromocriptine-QR dopamine D2 receptor agonists and bile acid sequestrants Bile acid sequestrant in the management of type 2 diabetes Number of 10 DPP-4 inhibitor classes of GLP-1 receptor agonist Amylinomimetic anti- 8 Glinide Basal insulin analogue Identify the benefits and risks of the newer non-insulin hyperglycemic Thiazolidinedione agents 6 Alpha-glucosidase inhibitor treatment options Phenformin Human Rapid-acting insulin analogue 4 Sulphonylurea insulin Metformin Intermediate-acting insulin Phenformin Describe the potential uses of these therapies in the 2 withdrawn Soluble insulin treatment of type 2 diabetes 0 1920 1940 1960 1980 2000 2020 Year UGDP, DCCT and UKPDS studies. Buse, JB © 1 9/22/2015 Renal handling of glucose Collecting (180 L/day) Glomerulus duct (1000 mg/L) Proximal =180 g/day Distal tubule S1 tubule Glucose ~90% filtration SGLT2 Inhibitors ~10% S3 Glucose reabsorption Loop No/minimal of Henle glucose excretion S1 segment of proximal tubule S3 segment of proximal tubule - ~90% glucose reabsorbed - ~10% glucose reabsorbed - Facilitated by SGLT2 - Facilitated by SGLT1 SGLT = Sodium-dependent glucose transporter Adapted from: 1.