Is Bendamustine-Rituximab a Reasonable Treatment in Selected Older Patients with Diffuse Large B Cell Lymphoma? Results from a Multicentre, Retrospective Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hodgkin Lymphoma Treatment Regimens
HODGKIN LYMPHOMA TREATMENT REGIMENS (Part 1 of 5) Clinical Trials: The National Comprehensive Cancer Network recommends cancer patient participation in clinical trials as the gold standard for treatment. Cancer therapy selection, dosing, administration, and the management of related adverse events can be a complex process that should be handled by an experienced health care team. Clinicians must choose and verify treatment options based on the individual patient; drug dose modifications and supportive care interventions should be administered accordingly. The cancer treatment regimens below may include both U.S. Food and Drug Administration-approved and unapproved indications/regimens. These regimens are provided only to supplement the latest treatment strategies. These Guidelines are a work in progress that may be refined as often as new significant data become available. The NCCN Guidelines® are a consensus statement of its authors regarding their views of currently accepted approaches to treatment. Any clinician seeking to apply or consult any NCCN Guidelines® is expected to use independent medical judgment in the context of individual clinical circumstances to determine any patient’s care or treatment. The NCCN makes no warranties of any kind whatsoever regarding their content, use, or application and disclaims any responsibility for their application or use in any way. Classical Hodgkin Lymphoma1 Note: All recommendations are Category 2A unless otherwise indicated. Primary Treatment Stage IA, IIA Favorable (No Bulky Disease, <3 Sites of Disease, ESR <50, and No E-lesions) REGIMEN DOSING Doxorubicin + Bleomycin + Days 1 and 15: Doxorubicin 25mg/m2 IV push + bleomycin 10units/m2 IV push + Vinblastine + Dacarbazine vinblastine 6mg/m2 IV over 5–10 minutes + dacarbazine 375mg/m2 IV over (ABVD) (Category 1)2-5 60 minutes. -

HODGKIN LYMPHOMA TREATMENT REGIMENS (Part 1 of 2)
HODGKIN LYMPHOMA TREATMENT REGIMENS (Part 1 of 2) The selection, dosing, and administration of anticancer agents and the management of associated toxicities are complex. Drug dose modifications and schedule and initiation of supportive care interventions are often necessary because of expected toxicities and because of individual patient variability, prior treatment, and comorbidities. Thus, the optimal delivery of anticancer agents requires a healthcare delivery team experienced in the use of such agents and the management of associated toxicities in patients with cancer. The cancer treatment regimens below may include both FDA-approved and unapproved uses/regimens and are provided as references only to the latest treatment strategies. Clinicians must choose and verify treatment options based on the individual patient. NOTE: GREY SHADED BOXES CONTAIN UPDATED REGIMENS. REGIMEN DOSING Classical Hodgkin Lymphoma—First-Line Treatment General treatment note: Routine use of growth factors is not recommended. Leukopenia is not a factor for treatment delay or dose reduction (except for escalated BEACOPP).1 CR=complete response IPS=International Prognostic Score PD=progressive disease PFTs=pulmonary function tests PR=partial response RT=radiation therapy SD=stable disease Stage IA, IIA Favorable ABVD (doxorubicin [Adriamycin] Days 1 and 15: Doxorubicin 25mg/m2 IV + bleomycin 10mg/m2 IV + vinblastine + bleomycin + vinblastine + 6mg/m2 IV + dacarbazine 375mg/m2 IV. dacarbazine [DTIC-Dome]) + Repeat cycle every 4 weeks for 2–4 cycles. involved-field radiotherapy (IFRT)1–4 Follow with IFRT after completion of chemotherapy. Abbreviated Stanford V Weeks 1, 3, 5 and 7: Vinblastine 6mg/m2 IV + doxorubicin 25mg/m2 IV. (doxorubicin + vinblastine + Weeks 1 and 5: Mechlorethamine 6mg/m2. -

(Rituxan®), Rituximab-Abbs (Truxima®), Rituximab-Pvvr (Ruxience®) Prior Authorization Drug Coverage Policy
1 Rituximab Products: Rituximab (Rituxan®), Rituximab-abbs (Truxima®), Rituximab-pvvr (Ruxience®) Prior Authorization Drug Coverage Policy Effective Date: 2/1/2021 Revision Date: n/a Review Date: 7/2/20 Lines of Business: Commercial Policy type: Prior Authorization This Drug Coverage Policy provides parameters for the coverage of rituximab (Rituxan®), rituximab-abbs (Truxima®), and rituximab-pvvr (Ruxience®). Consideration of medically necessary indications are based upon U.S. Food and Drug Administration (FDA) indications, recommended uses within the Centers of Medicare & Medicaid Services (CMS) five recognized compendia, including the National Comprehensive Cancer Network (NCCN) Drugs & Biologics Compendium (Category 1 or 2A recommendations), and peer-reviewed scientific literature eligible for coverage according to the CMS, Medicare Benefit Policy Manual, Chapter 15, section 50.4.5 titled, “Off- Label Use of Anti-Cancer Drugs and Biologics.” This policy evaluates whether the drug therapy is proven to be effective based on published evidence-based medicine. Drug Description1-3 Rituximab (Rituxan®), rituximab-abbs (Truxima®), and rituximab-pvvr (Ruxience®) are monoclonal antibodies that target the CD20 antigen expressed on the surface of pre-B and mature B- lymphocytes. Upon binding to cluster of differentiation (CD) 20, rituximab mediates B-cell lysis. Possible mechanisms of cell lysis include complement dependent cytotoxicity (CDC) and antibody dependent cell mediated cytotoxicity (ADCC). B cells are believed to play a role in the pathogenesis of rheumatoid arthritis (RA) and associated chronic synovitis. In this setting, B cells may be acting at multiple sites in the autoimmune/inflammatory process, including through production of rheumatoid factor (RF) and other autoantibodies, antigen presentation, T-cell activation, and/or proinflammatory cytokine production. -
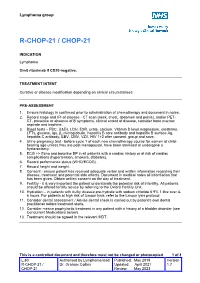
R-Chop-21 / Chop-21
Lymphoma group R-CHOP-21 / CHOP-21 INDICATION Lymphoma Omit rituximab if CD20-negative. TREATMENT INTENT Curative or disease modification depending on clinical circumstances PRE-ASSESSMENT 1. Ensure histology is confirmed prior to administration of chemotherapy and document in notes. 2. Record stage and IPI of disease - CT scan (neck, chest, abdomen and pelvis), and/or PET- CT, presence or absence of B symptoms, clinical extent of disease, consider bone marrow aspirate and trephine. 3. Blood tests – FBC, U&Es, LDH, ESR, urate, calcium, Vitamin D level,magnesium, creatinine, LFTs, glucose, Igs, β2 microglobulin, hepatitis B core antibody and hepatitis B surface Ag, hepatitis C antibody, EBV, CMV, VZV, HIV 1+2 after consent, group and save. 4. Urine pregnancy test • before cycle 1 of each new chemotherapy course for women of child- bearing age unless they are post-menopausal, have been sterilised or undergone a hysterectomy. 5. ECG +/- Echo and baseline BP in all patients with a cardiac history or at risk of cardiac complications (hypertension, smokers, diabetes). 6. Record performance status (WHO/ECOG). 7. Record height and weight. 8. Consent - ensure patient has received adequate verbal and written information regarding their disease, treatment and potential side effects. Document in medical notes all information that has been given. Obtain written consent on the day of treatment. 9. Fertility - it is very important the patient understands the potential risk of infertility. All patients should be offered fertility advice by referring to the Oxford Fertility Unit. 10. Hydration – in patients with bulky disease pre-hydrate with sodium chloride 0.9% 1 litre over 4- 6 hours. -

Anaplastic Large Cell Lymphoma (ALCL)
Helpline (freephone) 0808 808 5555 [email protected] www.lymphoma-action.org.uk Anaplastic large cell lymphoma (ALCL) This page is about anaplastic large-cell lymphoma (ALCL), a type of T-cell lymphoma. On this page What is ALCL? Who gets it? Symptoms Treatment Relapsed and refractory ALCL Research and targeted treatments We have separate information about the topics in bold font. Please get in touch if you’d like to request copies or if you would like further information about any aspect of lymphoma. Phone 0808 808 5555 or email [email protected]. What is ALCL? Anaplastic large cell lymphoma (ALCL) is a type of T-cell lymphoma – a non-Hodgkin lymphoma that develops from white blood cells called T cells. Under a microscope, the cancerous cells in ALCL look large, undeveloped and very abnormal (‘anaplastic’). There are four main types of ALCL. They have complicated names based on their features and the types of proteins they make: • ALK-positive ALCL (also known as ALK+ ALCL) is the most common type. In ALK-positive ALCL, the abnormal T cells have a genetic change (mutation) that means they make a protein called ‘anaplastic lymphoma kinase’ (ALK). In other words, they test positive for ALK. ALK-positive ALCL is a fast-growing (high-grade) lymphoma. Page 1 of 6 © Lymphoma Action • ALK-negative ALCL (also known as ALK- ALCL) is a high-grade lymphoma that accounts for around 3 in every 10 cases of ALCL. The abnormal T cells do not make the ALK protein – they test negative for ALK. -
![Bendamustine and Cytosine Arabinoside: a Highly Synergistic Combination Visco C*, Carli G and Rodeghiero F Further DNA Synthesis [24]](https://docslib.b-cdn.net/cover/9877/bendamustine-and-cytosine-arabinoside-a-highly-synergistic-combination-visco-c-carli-g-and-rodeghiero-f-further-dna-synthesis-24-599877.webp)
Bendamustine and Cytosine Arabinoside: a Highly Synergistic Combination Visco C*, Carli G and Rodeghiero F Further DNA Synthesis [24]
Open Access Austin Journal of Cancer and Clinical Research Editorial Bendamustine and Cytosine Arabinoside: A Highly Synergistic Combination Visco C*, Carli G and Rodeghiero F further DNA synthesis [24]. The synergistic effect of bendamustine Department of Cell Therapy and Hematology, San Bortolo and cytarabine could be related to the individual mechanism of Hospital, Italy action of the two drugs, whose serial administration would avoid *Corresponding author: Carlo Visco, Department of the saturation of the common pathways. Cells escaping the cell cycle Cell Therapy and Hematology, San Bortolo Hospital, Via arrest induced by bendamustine and trying to repair their damage Rodolfi 37, 36100 Vicenza, Italy, Tel: +39 0444 753626; would be prone to incorporate the metabolite ara-CTP into DNA, Fax: +39 0444 920708; Email: [email protected] as reported by Staib [19] in acute myeloid leukemia cells. Indeed, the Received: January 07, 2015; Accepted: March 16, sequential treatment with bendamustine followed by cytarabine was 2015; Published: April 03, 2015 proven to be more effective than simultaneous addition of the two drugs (Figure 2) [21-23]. The S phase of the cell cycle is a crucial step Editorial of replication in mantle cell lymphoma (MCL) cells, where cyclin D1 Bendamustine is a bifunctional compound that has shown clinical overexpression deregulates the cell cycle at the G1/S phase transition, activity against various human cancers including non-Hodgkin’s and and is likely the engine continuously pushing cells towards S-phase Hodgkin’s lymphoma [1,2], chronic lymphocytic leukemia (CLL) [3], (Figure 3). Indeed, both drugs are known to be particularly active in multiple myeloma [4,5], breast cancer [6], and small-cell lung cancer patients with MCL. -
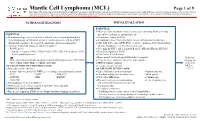
Mantle Cell Lymphoma (MCL)
Mantle Cell Lymphoma (MCL) Page 1 of 9 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. PATHOLOGIC DIAGNOSIS INITIAL EVALUATION ESSENTIAL: ● Physical exam: attention to node-bearing areas, including Waldeyer's ring, ESSENTIAL: size of liver and spleen, and patient’s age ● Hematopathology review of all slides with at least one tumor paraffin block. ● Performance status (ECOG) Hematopathology confirmation of classic versus aggressive variant of MCL ● B symptoms (fever, drenching night sweats, unintentional weight loss) (blastoid/pleomorphic). Re-biopsy if consult material is non-diagnostic. ● CBC with differential, LDH, BUN, creatinine, albumin, AST, total bilirubin, 1 ● Adequate immunophenotype to confirm diagnosis alkaline phosphatase, serum calcium, uric acid ○ Paraffin panel: ● Screening for HIV 1 and 2, hepatitis B and C (HBcAb, HBaAg, HCVAb) - Pan B-cell marker (CD19, CD20, PAX5), CD3, CD5, CD10, and cyclin D1 ● Beta-2 microglobulin (B2M) - Ki-67 (proliferation rate) ● Chest x-ray, PA and lateral or ● Bone marrow bilateral biopsy with unilateral aspirate Induction ○ Flow cytometry immunophenotyping: -
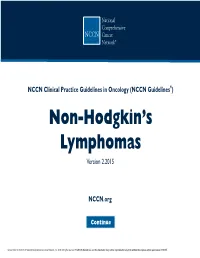
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines® ) Non-Hodgkin’S Lymphomas Version 2.2015
NCCN Guidelines Index NHL Table of Contents Discussion NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines® ) Non-Hodgkin’s Lymphomas Version 2.2015 NCCN.org Continue Version 2.2015, 03/03/15 © National Comprehensive Cancer Network, Inc. 2015, All rights reserved. The NCCN Guidelines® and this illustration may not be reproduced in any form without the express written permission of NCCN® . Peripheral T-Cell Lymphomas NCCN Guidelines Version 2.2015 NCCN Guidelines Index NHL Table of Contents Peripheral T-Cell Lymphomas Discussion DIAGNOSIS SUBTYPES ESSENTIAL: · Review of all slides with at least one paraffin block representative of the tumor should be done by a hematopathologist with expertise in the diagnosis of PTCL. Rebiopsy if consult material is nondiagnostic. · An FNA alone is not sufficient for the initial diagnosis of peripheral T-cell lymphoma. Subtypes included: · Adequate immunophenotyping to establish diagnosisa,b · Peripheral T-cell lymphoma (PTCL), NOS > IHC panel: CD20, CD3, CD10, BCL6, Ki-67, CD5, CD30, CD2, · Angioimmunoblastic T-cell lymphoma (AITL)d See Workup CD4, CD8, CD7, CD56, CD57 CD21, CD23, EBER-ISH, ALK · Anaplastic large cell lymphoma (ALCL), ALK positive (TCEL-2) or · ALCL, ALK negative > Cell surface marker analysis by flow cytometry: · Enteropathy-associated T-cell lymphoma (EATL) kappa/lambda, CD45, CD3, CD5, CD19, CD10, CD20, CD30, CD4, CD8, CD7, CD2; TCRαβ; TCRγ Subtypesnot included: · Primary cutaneous ALCL USEFUL UNDER CERTAIN CIRCUMSTANCES: · All other T-cell lymphomas · Molecular analysis to detect: antigen receptor gene rearrangements; t(2;5) and variants · Additional immunohistochemical studies to establish Extranodal NK/T-cell lymphoma, nasal type (See NKTL-1) lymphoma subtype:βγ F1, TCR-C M1, CD279/PD1, CXCL-13 · Cytogenetics to establish clonality · Assessment of HTLV-1c serology in at-risk populations. -

A Bendamustine Resistance Gene Signature in Diffuse Large B-Cell Lymphoma and Multiple Myeloma
Issa et al. Cancer Drug Resist 2021;4:208-22 Cancer DOI: 10.20517/cdr.2020.76 Drug Resistance Original Article Open Access A bendamustine resistance gene signature in diffuse large B-cell lymphoma and multiple myeloma Issa Ismail Issa1,2, Rasmus Froberg Brøndum1,2, Hanne Due1,2, Linnéa Schmidt1,2, Martin Bøgsted1,2, Karen Dybkær1,2 1Department of Haematology, Aalborg University Hospital, Aalborg 9000, Denmark. 2Department of Clinical Medicine, Aalborg University, Aalborg 9000, Denmark. Correspondence to: Prof. Karen Dybkær, Department of Haematology, Aalborg University Hospital, Sdr. Skovvej 15, Aalborg 9000, Denmark. E-mail: [email protected] How to cite this article: Issa II, Brøndum RF, Due H, Schmidt L, Bøgsted M, Dybkær K. A bendamustine resistance gene signature in diffuse large B-cell lymphoma and multiple myeloma. Cancer Drug Resist 2021;4:208-22. http://dx.doi.org/10.20517/cdr.2020.76 Received: 4 Sep 2020 First Decision: 12 Oct 2020 Revised: 30 Oct 2020 Accepted: 5 Nov 2020 Available online: 19 Mar 2021 Academic Editor: Godefridus J. Peters Copy Editor: Cai-Hong Wang Production Editor: Jing Yu Abstract Aim: Bendamustine is primarily used for treatment of indolent lymphomas but has shown efficacy in some patients with diffuse large B-cell lymphoma (DLBCL) and multiple myeloma (MM). Molecular-based patient stratification for identification of resistant patients, who will benefit from alternative treatments, is important. The aim of this study was to develop a resistance gene signature (REGS) from bendamustine dose-response assays in cultures of DLBCL and MM cell lines, enabling prediction of bendamustine response in DLBCL and MM patients. -

Analysis Compared with Classical Hodgkin Lymphoma
From bloodjournal.hematologylibrary.org by guest on July 21, 2014. For personal use only. 2014 123: 3567-3573 doi:10.1182/blood-2013-12-541078 originally published online April 8, 2014 Advanced-stage nodular lymphocyte predominant Hodgkin lymphoma compared with classical Hodgkin lymphoma: a matched pair outcome analysis Katharine H. Xing, Joseph M. Connors, Anky Lai, Mubarak Al-Mansour, Laurie H. Sehn, Diego Villa, Richard Klasa, Tamara Shenkier, Randy D. Gascoyne, Brian Skinnider and Kerry J. Savage Updated information and services can be found at: http://bloodjournal.hematologylibrary.org/content/123/23/3567.full.html Articles on similar topics can be found in the following Blood collections Clinical Trials and Observations (3892 articles) Free Research Articles (2531 articles) Lymphoid Neoplasia (1767 articles) Information about reproducing this article in parts or in its entirety may be found online at: http://bloodjournal.hematologylibrary.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://bloodjournal.hematologylibrary.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://bloodjournal.hematologylibrary.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved. From bloodjournal.hematologylibrary.org by guest on July 21, 2014. For personal use only. Regular Article CLINICAL TRIALS AND OBSERVATIONS Advanced-stage nodular lymphocyte predominant Hodgkin lymphoma compared with classical Hodgkin lymphoma: a matched pair outcome analysis Katharine H. -

Bendamustine Plus Rituximab: Is It a BRIGHT Idea?
Editorial Commentary Page 1 of 4 Bendamustine plus rituximab: is it a BRIGHT idea? Carlo Visco1, Francesca Maria Quaglia1, Chiara Bovo2, Maria Chiara Tisi3, Mauro Krampera1 1Department of Medicine, Section of Hematology, University of Verona, Verona, Italy; 2Medical Direction, University Hospital of Verona, Verona, Italy; 3Cell Therapy and Hematology, San Bortolo Hospital, Vicenza, Italy Correspondence to: Carlo Visco, MD. Associate Professor of Hematology, Department of Medicine, Section of Hematology, University of Verona, P.le L.A. Scuro 10, 37134 Verona, Italy. Email: [email protected]. Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Xinyi Du (Department of Hematology, Northern Jiangsu People’s Hospital, Yangzhou, China). Comment on: Flinn IW, van der Jagt R, Kahl B, et al. First-Line Treatment of Patients With Indolent Non-Hodgkin Lymphoma or Mantle-Cell Lymphoma With Bendamustine Plus Rituximab Versus R-CHOP or R-CVP: Results of the BRIGHT 5-Year Follow-Up Study. J Clin Oncol 2019;37:984-91. Submitted Sep 20, 2019. Accepted for publication Oct 14, 2019. doi: 10.21037/cco.2019.10.03 View this article at: http://dx.doi.org/10.21037/cco.2019.10.03 Flinn et al. have reported the results of the long-term in the BRIGHT study were eagerly awaited. As the Stil- follow-up for the BRIGHT trial, an international study 1 trial, the BRIGHT study (3) included patients with which compared the efficacy and the safety of bendamustine follicular lymphoma (grade 1 or 2, excluding grade 3A), plus rituximab (BR) with either rituximab plus lymphoplasmacytic lymphoma, splenic marginal zone B-cell cyclophosphamide, doxorubicin, vincristine, and prednisone lymphoma, extranodal marginal zone lymphoma (MZL) (R-CHOP) or rituximab plus cyclophosphamide, vincristine, of mucosa-associated lymphoid tissue type, nodal marginal and prednisone (R-CVP) for treatment-naive patients with zone B-cell lymphoma (371 patients with iNHL), or MCL indolent non-Hodgkin lymphoma (iNHL) or mantle-cell (74 patients). -

Bendamustine: Treanda®; Bendeka®; Belrapzo™
Bendamustine: Treanda®; Bendeka®; Belrapzo™ RTD (Intravenous) Document Number: IH-0130 Last Review Date: 03/01/2021 Date of Origin: 01/01/12 Dates Reviewed: 12/2011, 02/2013, 09/2013, 12/2013, 03/2014, 06/2014, 09/2014, 12/2014, 03/2015, 05/2015, 11/2015, 02/2016, 05/2016, 08/2016, 11/2016, 02/2017, 05/2017, 08/2017, 11/2017, 02/2018, 05/2018, 09/2018, 12/2018, 03/2019, 06/2019, 09/2019, 12/2019, 03/2020, 06/2020, 09/2020, 03/2021 I. Length of Authorization 1-3,5,8,13 • Non-Hodgkin’s Lymphoma (NHL), Chronic Lymphocytic Leukemia (CLL)/Small Lymphocytic Lymphoma (SLL), Waldenström’s Macroglobulinemia (WM)/Lymphoplasmacytic Lymphoma (LPL), Classic Hodgkin Lymphoma (cHL): o Coverage will be provided for six months and may NOT be renewed. • Multiple Myeloma: o Coverage will be provided for eight months and may NOT be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: Treanda 100 mg lyophilized powder for injection: 6 vials every 21 days Treanda 25 mg lyophilized powder for injection: 3 vials every 21 days Bendeka 100 mg/4 mL multi-dose vial: 6 vials every 21 days Belrapzo 100 mg/4 mL RTD multi-dose vial: 6 vials every 21 days B. Max Units (per dose and over time) [HCPCS Unit]: NHL: • 600 billable units every 21 days WM/LPL: • 450 billable units every 28 days cccHL:cHL: • 600 billable units every 28 days CLL/SLL & MMMultipleMultiple MMMyelomaMyelomayeloma:::: • 500 billable units every 28 days Proprietary & Confidential © 2021 Magellan Health, Inc. III. Initial Approval Criteria 1 Coverage is provided in the following