MYC Promotes Tryptophan Uptake and Metabolism by the Kynurenine Pathway in Colon Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Remodeling Adipose Tissue Through in Silico Modulation of Fat Storage For
Chénard et al. BMC Systems Biology (2017) 11:60 DOI 10.1186/s12918-017-0438-9 RESEARCHARTICLE Open Access Remodeling adipose tissue through in silico modulation of fat storage for the prevention of type 2 diabetes Thierry Chénard2, Frédéric Guénard3, Marie-Claude Vohl3,4, André Carpentier5, André Tchernof4,6 and Rafael J. Najmanovich1* Abstract Background: Type 2 diabetes is one of the leading non-infectious diseases worldwide and closely relates to excess adipose tissue accumulation as seen in obesity. Specifically, hypertrophic expansion of adipose tissues is related to increased cardiometabolic risk leading to type 2 diabetes. Studying mechanisms underlying adipocyte hypertrophy could lead to the identification of potential targets for the treatment of these conditions. Results: We present iTC1390adip, a highly curated metabolic network of the human adipocyte presenting various improvements over the previously published iAdipocytes1809. iTC1390adip contains 1390 genes, 4519 reactions and 3664 metabolites. We validated the network obtaining 92.6% accuracy by comparing experimental gene essentiality in various cell lines to our predictions of biomass production. Using flux balance analysis under various test conditions, we predict the effect of gene deletion on both lipid droplet and biomass production, resulting in the identification of 27 genes that could reduce adipocyte hypertrophy. We also used expression data from visceral and subcutaneous adipose tissues to compare the effect of single gene deletions between adipocytes from each -

METABOLIC EVOLUTION in GALDIERIA SULPHURARIA By
METABOLIC EVOLUTION IN GALDIERIA SULPHURARIA By CHAD M. TERNES Bachelor of Science in Botany Oklahoma State University Stillwater, Oklahoma 2009 Submitted to the Faculty of the Graduate College of the Oklahoma State University in partial fulfillment of the requirements for the Degree of DOCTOR OF PHILOSOPHY May, 2015 METABOLIC EVOLUTION IN GALDIERIA SUPHURARIA Dissertation Approved: Dr. Gerald Schoenknecht Dissertation Adviser Dr. David Meinke Dr. Andrew Doust Dr. Patricia Canaan ii Name: CHAD M. TERNES Date of Degree: MAY, 2015 Title of Study: METABOLIC EVOLUTION IN GALDIERIA SULPHURARIA Major Field: PLANT SCIENCE Abstract: The thermoacidophilic, unicellular, red alga Galdieria sulphuraria possesses characteristics, including salt and heavy metal tolerance, unsurpassed by any other alga. Like most plastid bearing eukaryotes, G. sulphuraria can grow photoautotrophically. Additionally, it can also grow solely as a heterotroph, which results in the cessation of photosynthetic pigment biosynthesis. The ability to grow heterotrophically is likely correlated with G. sulphuraria ’s broad capacity for carbon metabolism, which rivals that of fungi. Annotation of the metabolic pathways encoded by the genome of G. sulphuraria revealed several pathways that are uncharacteristic for plants and algae, even red algae. Phylogenetic analyses of the enzymes underlying the metabolic pathways suggest multiple instances of horizontal gene transfer, in addition to endosymbiotic gene transfer and conservation through ancestry. Although some metabolic pathways as a whole appear to be retained through ancestry, genes encoding individual enzymes within a pathway were substituted by genes that were acquired horizontally from other domains of life. Thus, metabolic pathways in G. sulphuraria appear to be composed of a ‘metabolic patchwork’, underscored by a mosaic of genes resulting from multiple evolutionary processes. -

Expression and Regulation of the Rate-Limiting Enzymes of the Kynurenine Pathway in the Mouse Brain by Alexandra Kelly Brooks Di
EXPRESSION AND REGULATION OF THE RATE-LIMITING ENZYMES OF THE KYNURENINE PATHWAY IN THE MOUSE BRAIN BY ALEXANDRA KELLY BROOKS DISSERTATION Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Neuroscience in the Graduate College of the University of Illinois at Urbana-Champaign, 2017 Urbana, Illinois Doctoral Committee: Research Assistant Professor Robert H. McCusker, Chair Assistant Professor Andrew J. Steelman Assistant Professor Monica Uddin Professor Rodney W. Johnson P a g e | ii ABSTRACT During the mid-1900’s, early anti-depressants were developed to increase levels of catecholamines within the brain, leading to the theory that depression symptomology was a result of an imbalance of neurotransmitters within the brain. To date, the catecholamine theory of depression is still held to be the prevailing theory as selective serotonin reuptake inhibitors being the most commonly prescribed anti-depressants. However, the incidence of depression is still rising with a vast amount of patients failing to respond to current treatments, and with this knowledge, additional theories of the neurobiology of depression have arisen over the past 30 years. A leading theory is Kynurenine Pathway activation in relation to inflammation- or stress- induced depression-like behaviors. There has been a tremendous amount of data connecting activated immune system (or hypothalamic-pituitary-adrenal axis), increased kynurenine production and depression symptomology. Thus, understanding the factors that activate this -

Tryptophan and Kynurenine Enhances the Stemness and Osteogenic Differentiation of Bone Marrow-Derived Mesenchymal Stromal Cells in Vitro and in Vivo
materials Article Tryptophan and Kynurenine Enhances the Stemness and Osteogenic Differentiation of Bone Marrow-Derived Mesenchymal Stromal Cells In Vitro and In Vivo Hai Thanh Pham 1,2 , Mitsuaki Ono 3,*, Emilio Satoshi Hara 4,* , Ha Thi Thu Nguyen 1,2,3, Anh Tuan Dang 1,2,3, Hang Thuy Do 1,2,3, Taishi Komori 1, Ikue Tosa 1, Yuri Hazehara-Kunitomo 1,3, Yuya Yoshioka 1, Yasutaka Oida 1, Kentaro Akiyama 1 and Takuo Kuboki 1 1 Department of Oral Rehabilitation and Regenerative Medicine, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama 700-8558, Japan; [email protected] (H.T.P.); [email protected] (H.T.T.N.); [email protected] (A.T.D.); [email protected] (H.T.D.); [email protected] (T.K.); [email protected] (I.T.); [email protected] (Y.H.-K.); [email protected] (Y.Y.); [email protected] (Y.O.); [email protected] (K.A.); [email protected] (T.K.) 2 Faculty of Dentistry, Hai Phong University of Medicine and Pharmacy, Haiphong 04211, Vietnam 3 Department of Molecular Biology and Biochemistry, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama 700-8558, Japan 4 Department of Biomaterials, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama 700-8558, Japan * Correspondence: [email protected] (M.O.); [email protected] (E.S.H.); Tel.: +81-86-235-7127 (M.O.); +81-86-235-6667 (E.S.H.); Fax: +81-86-222-7768 (M.O.); +81-86-235-6669 (E.S.H.) Abstract: Aging tissues present a progressive decline in homeostasis and regenerative capacities, Citation: Pham, H.T.; Ono, M.; Hara, which has been associated with degenerative changes in tissue-specific stem cells and stem cell E.S.; Nguyen, H.T.T.; Dang, A.T.; Do, niches. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -
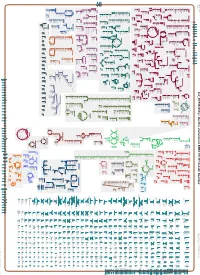
Generate Metabolic Map Poster
Authors: Pallavi Subhraveti Ron Caspi Peter Midford Peter D Karp An online version of this diagram is available at BioCyc.org. Biosynthetic pathways are positioned in the left of the cytoplasm, degradative pathways on the right, and reactions not assigned to any pathway are in the far right of the cytoplasm. Transporters and membrane proteins are shown on the membrane. Ingrid Keseler Periplasmic (where appropriate) and extracellular reactions and proteins may also be shown. Pathways are colored according to their cellular function. Gcf_001591825Cyc: Bacillus vietnamensis NBRC 101237 Cellular Overview Connections between pathways are omitted for legibility. Anamika Kothari sn-glycerol phosphate phosphate pro phosphate phosphate phosphate thiamine molybdate D-xylose D-ribose glutathione 3-phosphate D-mannitol L-cystine L-djenkolate lanthionine α,β-trehalose phosphate phosphate [+ 3 more] α,α-trehalose predicted predicted ABC ABC FliY ThiT XylF RbsB RS10935 UgpC TreP PutP RS10200 PstB PstB RS10385 RS03335 RS20030 RS19075 transporter transporter of molybdate of phosphate α,β-trehalose 6-phosphate L-cystine D-xylose D-ribose sn-glycerol D-mannitol phosphate phosphate thiamine glutathione α α phosphate phosphate phosphate phosphate L-djenkolate 3-phosphate , -trehalose 6-phosphate pro 1-phosphate lanthionine molybdate phosphate [+ 3 more] Metabolic Regulator Amino Acid Degradation Amine and Polyamine Biosynthesis Macromolecule Modification tRNA-uridine 2-thiolation Degradation ATP biosynthesis a mature peptidoglycan a nascent β an N-terminal- -

The Neurochemical Consequences of Aromatic L-Amino Acid Decarboxylase Deficiency
The neurochemical consequences of aromatic L-amino acid decarboxylase deficiency Submitted By: George Francis Gray Allen Department of Molecular Neuroscience UCL Institute of Neurology Queen Square, London Submitted November 2010 Funded by the AADC Research Trust, UK Thesis submitted for the degree of Doctor of Philosophy, University College London (UCL) 1 I, George Allen confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis. Signed………………………………………………….Date…………………………… 2 Abstract Aromatic L-amino acid decarboxylase (AADC) catalyses the conversion of 5- hydroxytryptophan (5-HTP) and L-3,4-dihydroxyphenylalanine (L-dopa) to the neurotransmitters serotonin and dopamine respectively. The inherited disorder AADC deficiency leads to a severe deficit of serotonin and dopamine as well as an accumulation of 5-HTP and L-dopa. This thesis investigated the potential role of 5- HTP/L-dopa accumulation in the pathogenesis of AADC deficiency. Treatment of human neuroblastoma cells with L-dopa or dopamine was found to increase intracellular levels of the antioxidant reduced glutathione (GSH). However inhibiting AADC prevented the GSH increase induced by L-dopa. Furthermore dopamine but not L-dopa, increased GSH release from human astrocytoma cells, which do not express AADC activity. GSH release is the first stage of GSH trafficking from astrocytes to neurons. This data indicates dopamine may play a role in controlling brain GSH levels and consequently antioxidant status. The inability of L-dopa to influence GSH concentrations in the absence of AADC or with AADC inhibited indicates GSH trafficking/metabolism may be compromised in AADC deficiency. -

(P -Value<0.05, Fold Change≥1.4), 4 Vs. 0 Gy Irradiation
Table S1: Significant differentially expressed genes (P -Value<0.05, Fold Change≥1.4), 4 vs. 0 Gy irradiation Genbank Fold Change P -Value Gene Symbol Description Accession Q9F8M7_CARHY (Q9F8M7) DTDP-glucose 4,6-dehydratase (Fragment), partial (9%) 6.70 0.017399678 THC2699065 [THC2719287] 5.53 0.003379195 BC013657 BC013657 Homo sapiens cDNA clone IMAGE:4152983, partial cds. [BC013657] 5.10 0.024641735 THC2750781 Ciliary dynein heavy chain 5 (Axonemal beta dynein heavy chain 5) (HL1). 4.07 0.04353262 DNAH5 [Source:Uniprot/SWISSPROT;Acc:Q8TE73] [ENST00000382416] 3.81 0.002855909 NM_145263 SPATA18 Homo sapiens spermatogenesis associated 18 homolog (rat) (SPATA18), mRNA [NM_145263] AA418814 zw01a02.s1 Soares_NhHMPu_S1 Homo sapiens cDNA clone IMAGE:767978 3', 3.69 0.03203913 AA418814 AA418814 mRNA sequence [AA418814] AL356953 leucine-rich repeat-containing G protein-coupled receptor 6 {Homo sapiens} (exp=0; 3.63 0.0277936 THC2705989 wgp=1; cg=0), partial (4%) [THC2752981] AA484677 ne64a07.s1 NCI_CGAP_Alv1 Homo sapiens cDNA clone IMAGE:909012, mRNA 3.63 0.027098073 AA484677 AA484677 sequence [AA484677] oe06h09.s1 NCI_CGAP_Ov2 Homo sapiens cDNA clone IMAGE:1385153, mRNA sequence 3.48 0.04468495 AA837799 AA837799 [AA837799] Homo sapiens hypothetical protein LOC340109, mRNA (cDNA clone IMAGE:5578073), partial 3.27 0.031178378 BC039509 LOC643401 cds. [BC039509] Homo sapiens Fas (TNF receptor superfamily, member 6) (FAS), transcript variant 1, mRNA 3.24 0.022156298 NM_000043 FAS [NM_000043] 3.20 0.021043295 A_32_P125056 BF803942 CM2-CI0135-021100-477-g08 CI0135 Homo sapiens cDNA, mRNA sequence 3.04 0.043389246 BF803942 BF803942 [BF803942] 3.03 0.002430239 NM_015920 RPS27L Homo sapiens ribosomal protein S27-like (RPS27L), mRNA [NM_015920] Homo sapiens tumor necrosis factor receptor superfamily, member 10c, decoy without an 2.98 0.021202829 NM_003841 TNFRSF10C intracellular domain (TNFRSF10C), mRNA [NM_003841] 2.97 0.03243901 AB002384 C6orf32 Homo sapiens mRNA for KIAA0386 gene, partial cds. -

THE ROLE of KYNURENINE, a TRYPTOPHAN METABOLITE THAT INCREASES with AGE, in MUSCLE ATROPHY and LIPID PEROXIDATION) by Helen Eliz
THE ROLE OF KYNURENINE, A TRYPTOPHAN METABOLITE THAT INCREASES WITH AGE, IN MUSCLE ATROPHY AND LIPID PEROXIDATION) By Helen Elizabeth Kaiser Submitted to the Faculty of the Graduate School of Augusta University in partial fulfillment of the Requirements of the Degree of (Doctor of Philosophy in Cellular Biology and Anatomy) April 2020 COPYRIGHT© 2020 by Helen Kaiser ACKNOWLEDGEMENTS I wish to express my deepest gratitude to my mentor Dr. Mark Hamrick. His support and advice were invaluable to my learning and development as a scientist. I would like to especially recognize Dr. Hamrick’s honesty to data, and kindness to everyone around him. It was an honor to work as his student, and to be a part of this project. I would like to thank my committee members, Drs. Carlos Isales, Meghan McGee-Lawrence, and Yutao Liu, for their continued support, guidance, and helpful suggestions. They have helped to shape and focus this project, and have augmented my experience as a student during the development of my dissertation. Additionally, I want to recognize and thank Dr. Sadanand Fulzele for sharing his wealth of knowledge in techniques, and always keeping his door open for student’s questions. Next, a most heartfelt thanks to my lab mates: Andrew Khayrullin, Bharati Mendhe, Ling Ruan and Emily Parker. This project has been a team effort, all of them have been fundamental to its success. I further want to show my appreciation for the rest of the department of Cellular Biology and Anatomy at Augusta University. The histology core members Donna Kumiski and Penny Roon for their direct help in sectioning, and contributions to this project. -

An Integrated Meta-Analysis of Peripheral Blood Metabolites and Biological Functions in Major Depressive Disorder
Molecular Psychiatry https://doi.org/10.1038/s41380-020-0645-4 ARTICLE An integrated meta-analysis of peripheral blood metabolites and biological functions in major depressive disorder 1,2,3 1,2,3 1,2,3 1,3 1,3 4,5 1,3 1,3 Juncai Pu ● Yiyun Liu ● Hanping Zhang ● Lu Tian ● Siwen Gui ● Yue Yu ● Xiang Chen ● Yue Chen ● 1,2,3 1,3 1,3 1,3 1,3 1,2,3 Lining Yang ● Yanqin Ran ● Xiaogang Zhong ● Shaohua Xu ● Xuemian Song ● Lanxiang Liu ● 1,2,3 1,3 1,2,3 Peng Zheng ● Haiyang Wang ● Peng Xie Received: 3 June 2019 / Revised: 24 December 2019 / Accepted: 10 January 2020 © The Author(s) 2020. This article is published with open access Abstract Major depressive disorder (MDD) is a serious mental illness, characterized by high morbidity, which has increased in recent decades. However, the molecular mechanisms underlying MDD remain unclear. Previous studies have identified altered metabolic profiles in peripheral tissues associated with MDD. Using curated metabolic characterization data from a large sample of MDD patients, we meta-analyzed the results of metabolites in peripheral blood. Pathway and network analyses were then performed to elucidate the biological themes within these altered metabolites. We identified 23 differentially 1234567890();,: 1234567890();,: expressed metabolites between MDD patients and controls from 46 studies. MDD patients were characterized by higher levels of asymmetric dimethylarginine, tyramine, 2-hydroxybutyric acid, phosphatidylcholine (32:1), and taurochenode- soxycholic acid and lower levels of L-acetylcarnitine, creatinine, L-asparagine, L-glutamine, linoleic acid, pyruvic acid, palmitoleic acid, L-serine, oleic acid, myo-inositol, dodecanoic acid, L-methionine, hypoxanthine, palmitic acid, L-tryptophan, kynurenic acid, taurine, and 25-hydroxyvitamin D compared with controls. -

Regulation of Nuclear Epigenome by Mitochondrial DNA Heteroplasmy
Regulation of nuclear epigenome by mitochondrial DNA heteroplasmy Piotr K. Kopinskia,b,c, Kevin A. Janssend,e, Patrick M. Schaeferc, Sophie Trefelyf,g, Caroline E. Perryc, Prasanth Potluric, Jesus A. Tintos-Hernandezc, Larry N. Singhc, Kelly R. Karchd,e, Sydney L. Campbellf, Mary T. Doang, Helen Jiangg, Itzhak Nissime, Eiko Nakamaru-Ogisoe, Kathryn E. Wellenf, Nathaniel W. Snyderg, Benjamin A. Garciad,e, and Douglas C. Wallacec,h,1 aHoward Hughes Medical Institute, University of Pennsylvania, Philadelphia, PA 19104; bPerelman School of Medicine, University of Pennsylvania, Philadelphia, PA 19104; cCenter for Mitochondrial and Epigenomic Medicine, Children’s Hospital of Philadelphia, Philadelphia, PA 19104; dEpigenetics Institute, University of Pennsylvania, Philadelphia, PA 19104; eDepartment of Biochemistry and Biophysics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA 19104; fDepartment of Cancer Biology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA 19104; gA.J. Drexel Autism Institute, Drexel University, Philadelphia, PA 19104; and hDepartment of Pediatrics, Division of Human Genetics, The Children’s Hospital of Philadelphia, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA 19104 Contributed by Douglas C. Wallace, May 27, 2019 (sent for review April 23, 2019; reviewed by Yidong Bai, Scott W. Ballinger, and Victor Faundez) Diseases associated with mitochondrial DNA (mtDNA) mutations are cardiomyopathy, lactic acidosis, and stroke-like episodes, pre- highly variable in phenotype, in large part because of differences in the senting separately or when in aggregate referred to as the percentage of normal and mutant mtDNAs (heteroplasmy) present MELAS syndrome. At 90% to 100% mutant, individuals manifest within the cell. For example, increasing heteroplasmy levels of the perinatal lethal diseases such as Leigh syndrome. -

Urinary Metabolomics to Identify a Unique Biomarker Panel for Detecting Colorectal Cancer: a Multicenter Study
Published OnlineFirst May 31, 2019; DOI: 10.1158/1055-9965.EPI-18-1291 Research Article Cancer Epidemiology, Biomarkers Urinary Metabolomics to Identify a Unique & Prevention Biomarker Panel for Detecting Colorectal Cancer: A Multicenter Study Lu Deng1, Kathleen Ismond1,2, Zhengjun Liu3, Jeremy Constable4, Haili Wang2, Olusegun I. Alatise5, Martin R. Weiser4, T.P. Kingham4, and David Chang1,2 Abstract Background: Population-based screening programs are paring the metabolomic profiles from colorectal cancer versus credited with earlier colorectal cancer diagnoses and treat- controls. Multiple models were constructed leading to a good ment initiation, which reduce mortality rates and improve separation of colorectal cancer from controls. patient health outcomes. However, recommended screen- Results: A panel of 17 metabolites was identified as possible ing methods are unsatisfactory as they are invasive, are biomarkers for colorectal cancer. Using only two of the select- resource intensive, suffer from low uptake, or have poor ed metabolites, namely diacetylspermine and kynurenine, a diagnostic performance. Our goal was to identify a urine predictor for detecting colorectal cancer was developed with an metabolomic-based biomarker panel for the detection of AUC of 0.864, a specificity of 80.0%, and a sensitivity of colorectal cancer that has the potential for global popula- 80.0%. tion-based screening. Conclusions: We present a potentially "universal" metabo- Methods: Prospective urine samples were collected from lomic biomarker panel for colorectal cancer independent of study participants. Based upon colonoscopy and histopathol- cohort clinical features based on a North American popula- ogy results, 342 participants (colorectal cancer, 171; healthy tion. Further research is needed to confirm the utility of the controls, 171) from two study sites (Canada, United States) profile in a prospective, population-based colorectal cancer were included in the analyses.