Pisaf – Integrated Family Health Program Final Report March 2006 – November 2012
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

B E N I N Benin
Birnin o Kebbi !( !( Kardi KANTCHARIKantchari !( !( Pékinga Niger Jega !( Diapaga FADA N'GOUMA o !( (! Fada Ngourma Gaya !( o TENKODOGO !( Guéné !( Madécali Tenkodogo !( Burkina Faso Tou l ou a (! Kende !( Founogo !( Alibori Gogue Kpara !( Bahindi !( TUGA Suroko o AIRSTRIP !( !( !( Yaobérégou Banikoara KANDI o o Koabagou !( PORGA !( Firou Boukoubrou !(Séozanbiani Batia !( !( Loaka !( Nansougou !( !( Simpassou !( Kankohoum-Dassari Tian Wassaka !( Kérou Hirou !( !( Nassoukou Diadia (! Tel e !( !( Tankonga Bin Kébérou !( Yauri Atakora !( Kpan Tanguiéta !( !( Daro-Tempobré Dammbouti !( !( !( Koyadi Guilmaro !( Gambaga Outianhou !( !( !( Borogou !( Tounkountouna Cabare Kountouri Datori !( !( Sécougourou Manta !( !( NATITINGOU o !( BEMBEREKE !( !( Kouandé o Sagbiabou Natitingou Kotoponga !(Makrou Gurai !( Bérasson !( !( Boukombé Niaro Naboulgou !( !( !( Nasso !( !( Kounounko Gbangbanrou !( Baré Borgou !( Nikki Wawa Nambiri Biro !( !( !( !( o !( !( Daroukparou KAINJI Copargo Péréré !( Chin NIAMTOUGOU(!o !( DJOUGOUo Djougou Benin !( Guerin-Kouka !( Babiré !( Afekaul Miassi !( !( !( !( Kounakouro Sheshe !( !( !( Partago Alafiarou Lama-Kara Sece Demon !( !( o Yendi (! Dabogou !( PARAKOU YENDI o !( Donga Aledjo-Koura !( Salamanga Yérémarou Bassari !( !( Jebba Tindou Kishi !( !( !( Sokodé Bassila !( Igbéré Ghana (! !( Tchaourou !( !(Olougbé Shaki Togo !( Nigeria !( !( Dadjo Kilibo Ilorin Ouessé Kalande !( !( !( Diagbalo Banté !( ILORIN (!o !( Kaboua Ajasse Akalanpa !( !( !( Ogbomosho Collines !( Offa !( SAVE Savé !( Koutago o !( Okio Ila Doumé !( -

Online Appendix to “Can Informed Public Deliberation Overcome Clientelism? Experimental Evidence from Benin”
Online Appendix to “Can Informed Public Deliberation Overcome Clientelism? Experimental Evidence from Benin” by Thomas Fujiwara and Leonard Wantchekon 1. List of Sample Villages Table A1 provides a list of sample villages, with their experimental and dominant can- didates. 2. Results by Commune/Stratum Table A2.1-A2.3 presents the results by individual commune/stratum. 3. Survey Questions and the Clientelism Index Table A3.1 provides the estimates for each individual component of the clientelism index, while Table A3.2 details the questions used in the index. 4. Treatment Effects on Candidate Vote Shares Table A4 provides the treatment effect on each individual candidate vote share. 5. Estimates Excluding Communes where Yayi is the EC Table A5 reports results from estimations that drop the six communes where Yayi is the EC. Panel A provides estimates analogous from those of Table 2, while Panels B and C report estimates that are similar to those of Table 3. The point estimates are remarkably similar to the original ones, even though half the sample has been dropped (which explains why some have a slight reduction in significance). 1 6. Estimates Including the Commune of Toffo Due to missing survey data, all the estimates presented in the main paper exclude the commune of Toffo, the only one where Amoussou is the EC. However, electoral data for this commune is available. This allows us to re-estimate the electoral data-based treatment effects including the commune. Table A6.1 re-estimates the results presented on Panel B of Table 2. The qualitative results remain the same. -

Indirect Exposure to Colonial Education and Intergenerational
The Strength of Weak Ties: Indirect Exposure to Colonial Education and Intergenerational Mobility in Benin ⇤ Leonard Wantchekon† April 12, 2019 Abstract We use historical micro-level data from the first regional schools in colonial Benin to esti- mate the e↵ect of education on social mobility over three generations. Since school location and student cohorts were selected quasi-randomly, the e↵ect of education can be estimated by comparing the treated to the untreated living in the same village as well as those from villages with no school (Wantchekon et al. [2015]). We find positive treatment e↵ects of education on social mobility across three generations. Surprisingly, the e↵ect is strongest for descendants of grandparents who were exposed to education only through their social networks (the untreated living in villages with a school). We interpret this result as evidence of “the strength of weak ties” (Grannoveter [1977]). Finally, exploring the underlying mechanism of our results, we find that mobility from the first to the second generation is driven by parental aspiration, which is sustained by the risk attitudes and mobility of the third generation. ⇤This paper was prepared for the NYU Development Research Institute success project. I would like to thank James Hollyer, James Feigenbaum, James Habyarimana, Nathan Nunn, Dozie Okoye, Marc Ratkovic, Matthew Salganik, Stellios Michalopoulos, Marcella Alsan, and conference participants at ASE (SIER), Brown, George Washington University, NYU, Princeton, Toulouse School of Economics, Stanford University, and World Bank for comments. I would also like to thank the research team of Institute for Empirical Research in Political Economy (IERPE) in Benin, especially Romuald Anago, Kassim Assouma, Benjamin Dji↵a, Andre Gueguehoun, and Clement Litchegbe, for leading the data collection. -

Disposal of Persistent Organic Pollutants and Obsolete Pesticides and Strengthening Life-Cycle Management of Pesticides in Benin”
Project evaluation series Mid-term evaluation of “Disposal of Persistent Organic Pollutants and Obsolete Pesticides and Strengthening Life-cycle Management of Pesticides in Benin” Project evaluation series Mid-term evaluation of “Disposal of persistent organic pollutants and obsolete pesticides and strengthening life-cycle management of pesticides in Benin” GCP/BEN/056/GFF FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS Rome, 2019 Required citation: FAO. 2019. Mid-term evaluation of “Disposal of Persistent Organic Pollutants and Obsolete Pesticides and Strengthening Life-cycle Management of Pesticides in Benin”. Rome. The designations employed and the presentation of material in this information product do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations (FAO) concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or products of manufacturers, whether or not these have been patented, does not imply that these have been endorsed or recommended by FAO in preference to others of a similar nature that are not mentioned. The views expressed in this information product are those of the author(s) and do not necessarily reflect the views or policies of FAO. © FAO, 2019 Some rights reserved. This work is made available under the Creative Commons Attribution- NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/ licenses/by-nc-sa/3.0/igo/legalcode/legalcode). Under the terms of this licence, this work may be copied, redistributed and adapted for non-commercial purposes, provided that the work is appropriately cited. -

Identification 2- Education
CURRICULUM VITAE 1- Identification Name (First, Family) : Constant Kodjo, ADJIEN Sex : Male Date and place of birth : April,9th 1962, Lomé (TOGO) Civil status : Married, four children Nationality: : Beninese Permanent address : 08 BP 1045 Tri postal, Cotonou Tél : + 229 95 56 10 76 Email : [email protected] 2- Education ✓ Professor of Neurology of African and Malagasy Universities/Council for Higher Education (CAMES), Bangui, July 2019 ✓ Senior Lecturer in Neurology at CAMES, Yaounde, 2014 ✓ Certification of registration on the Aptitude List for The Functions of Master Assistant Côte A. Ouagadougou, 2010 ✓ Inter-University Diploma (IUD) of Epileptology, Nancy, 2007 ✓ In-depth Specialized Training Certificate in Neurology, Marseille, 2006 ✓ Certificate of Clinical and Epidemiology Research Methodology, Limoges,2001 ✓ University Diploma (UD) of Clinical Neurophysiological Explorations, Paris VI, 2001 ✓ Certificate of Special Studies (CES) in Neurology, Abidjan, 2002 ✓ State PhD in Medicine, Cotonou, 1994 1- Employement record - Since February 2018: Head of Training and Medical Research at the of Medical Affairs Direction (MAD) of CNHU-HKM - Since November 2014: Associate Lecturer at the University Neurology Clinic (CUN) at CNHU-HKM in Cotonou - 2010-2014: Master - Assistant Clinic Manager at the CUN at CNHU- HKM in Cotonou - 2009 2007: Assistant Head of Clinic at the University Clinic of Neurology (CUN) at CNHU-HKM in Cotonou - 2006-2007: Neurologist, Neurophysiologist and Epileptologist at CNHU in Cotonou - 2005-2006: Doing Intern function (FFI) at the Centre Saint Paul- Henri Gastaut Hospital (AFSA internship in Neurology and IUD in Epileptology, 2 semesters, in Marseille, France) - 2002-2005: Neurologist at C.N.H.U in Cotonou, Benin - 2000-2001: Associate In the Neurology Department, CHRU Dupuytren de Limoges (France) 2- Research fields 1. -

Monographie Des Départements Du Zou Et Des Collines
Spatialisation des cibles prioritaires des ODD au Bénin : Monographie des départements du Zou et des Collines Note synthèse sur l’actualisation du diagnostic et la priorisation des cibles des communes du département de Zou Collines Une initiative de : Direction Générale de la Coordination et du Suivi des Objectifs de Développement Durable (DGCS-ODD) Avec l’appui financier de : Programme d’appui à la Décentralisation et Projet d’Appui aux Stratégies de Développement au Développement Communal (PDDC / GIZ) (PASD / PNUD) Fonds des Nations unies pour l'enfance Fonds des Nations unies pour la population (UNICEF) (UNFPA) Et l’appui technique du Cabinet Cosinus Conseils Tables des matières 1.1. BREF APERÇU SUR LE DEPARTEMENT ....................................................................................................... 6 1.1.1. INFORMATIONS SUR LES DEPARTEMENTS ZOU-COLLINES ...................................................................................... 6 1.1.1.1. Aperçu du département du Zou .......................................................................................................... 6 3.1.1. GRAPHIQUE 1: CARTE DU DEPARTEMENT DU ZOU ............................................................................................... 7 1.1.1.2. Aperçu du département des Collines .................................................................................................. 8 3.1.2. GRAPHIQUE 2: CARTE DU DEPARTEMENT DES COLLINES .................................................................................... 10 1.1.2. -

CHAPTER II 1. Entry Summaries Page 2
1 CHAPTER I Table of Contents: CHAPTER II 1. Entry summaries Page 2 – 9 CHAPTER III 1. Abjata Khalif: Human trafficking Page10-12 2. Andualem Sisay: Ethiopia‘s crippled agriculture Page 13-15 3. Benjamin Tetteh: At mercy of the sea Page 16-18 4. Bibi-Aisha Wadualla: Religious bias in Egpy‘s universities Page 19-20 5. Deogratius Mmana: How dangerous criminals get out of jail before time to cause more havoc in public Page 21- 23 6. Kassim Mohamed: Pirates: Social bandits in Africa Page 24-27 7. Ken Opala: Lush Mrima Hill may be a death trap for unsuspecting residents Page 28-30 8. Khadija The Great Billion Dollar Drug Scam Page 31 - 35 9. Kipchumba Some: Police killings of youth Page 36-37 10. Muhyadin Ahmed Roble: What it Takes to Cover a Story in Somalia Page 38-40 11. Nicholas Ibekwe: Gowen and Bayero worked for Pfizer Page 41-43 12. Olu Jacob: The Muslim who risked all his Christian neighbours Page 44 -46 13. Patrick Mayoyo: Kenyan firms make killing from piracy Page 47 -48 14. Peter Nkanga: Last minute oil deals that cost Nigeria dear Page 49-52 15. Ramata Sore: Racist coverage of Africa in the US at the time of the World CupPage 53-55 16. Stephen Nartey: Ivorian girls trade sex for food Page 56 - 56 17. Tereza Ndanga: Cashing in on illegal abortions in Malawi Page 57 -58 18. Toyosi Ogunseye: Public school toilets, pits of the death and diseases Page 59 - 62 19. Estacio Valoi: Leaders complicit in the looting of wood in Zambezia Page 63 - 65 20. -
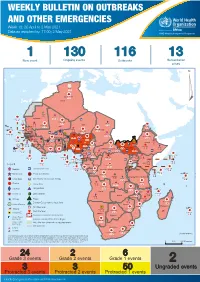
Weekly Bulletin on Outbreaks
WEEKLY BULLETIN ON OUTBREAKS AND OTHER EMERGENCIES Week 18: 26 April to 2 May 2021 Data as reported by: 17:00; 2 May 2021 REGIONAL OFFICE FOR Africa WHO Health Emergencies Programme 1 130 116 13 New event Ongoing events Outbreaks Humanitarian crises 64 0 122 522 3 270 Algeria ¤ 36 13 612 0 5 901 175 Mauritania 7 2 13 915 489 110 0 7 0 Niger 18 448 455 Mali 3 671 10 567 0 6 0 2 079 4 4 828 170 Eritrea Cape Verde 40 433 1 110 Chad Senegal 5 074 189 61 0 Gambia 27 0 3 0 24 368 224 1 069 5 Guinea-Bissau 847 17 7 0 Burkina Faso 236 49 258 384 3 726 0 165 167 2 063 Guinea 13 319 157 12 3 736 67 1 1 23 12 Benin 30 0 Nigeria 1 873 72 0 Ethiopia 540 2 556 5 6 188 15 Sierra Leone Togo 3 473 296 52 14 Ghana 70 607 1 064 6 411 88 Côte d'Ivoire 10 583 115 14 484 479 65 0 40 0 Liberia 17 0 South Sudan Central African Republic 1 029 2 49 0 97 17 25 0 22 333 268 46 150 287 92 683 779 Cameroon 7 0 28 676 137 843 20 3 1 160 422 2 763 655 2 91 0 123 12 6 1 488 6 4 057 79 13 010 7 694 112 Equatorial Guinea Uganda 1 0 542 8 Sao Tome and Principe 32 11 2 066 85 41 973 342 Kenya Legend 7 821 99 Gabon Congo 2 012 73 Rwanda Humanitarian crisis 2 310 35 25 253 337 Measles 23 075 139 Democratic Republic of the Congo 11 016 147 Burundi 4 046 6 Monkeypox Ebola virus disease Seychelles 29 965 768 235 0 420 29 United Republic of Tanzania Lassa fever Skin disease of unknown etiology 191 0 5 941 26 509 21 Cholera Yellow fever 63 1 6 257 229 26 993 602 cVDPV2 Dengue fever 91 693 1 253 Comoros Angola Malawi COVID-19 Leishmaniasis 34 096 1 148 862 0 3 840 146 Zambia 133 -

Benin• Floods Rapport De Situation #13 13 Au 30 Décembre 2010
Benin• Floods Rapport de Situation #13 13 au 30 décembre 2010 Ce rapport a été publié par UNOCHA Bénin. Il couvre la période du 13 au 30 Décembre. I. Evénements clés Le PDNA Team a organisé un atelier de consolidation et de finalisation des rapports sectoriels Le Gouvernement de la République d’Israël a fait don d’un lot de médicaments aux sinistrés des inondations La révision des fiches de projets du EHAP a démarré dans tous les clusters L’Organisation Ouest Africaine de la Santé à fait don d’un chèque de 25 millions de Francs CFA pour venir en aide aux sinistrés des inondations au Bénin L’ONG béninoise ALCRER a fait don de 500.000 F CFA pour venir en aide aux sinistrés des inondations 4 nouveaux cas de choléra ont été détectés à Cotonou II. Contexte Les eaux se retirent de plus en plus et les populations sinistrés manifestent de moins en moins le besoin d’installation sur les sites de déplacés. Ceux qui retournent dans leurs maisons expriment des besoins de tentes individuelles à installer près de leurs habitations ; une demande appuyée par les autorités locales. La veille sanitaire post inondation se poursuit, mais elle est handicapée par la grève du personnel de santé et les lots de médicaments pré positionnés par le cluster Santé n’arrivent pas à atteindre les bénéficiaires. Des brigades sanitaires sont provisoirement mises en place pour faire face à cette situation. La révision des projets de l’EHAP est en cours dans les 8 clusters et le Post Disaster Needs Assessment Team est en train de finaliser les rapports sectoriels des missions d’évaluation sur le terrain dans le cadre de l’élaboration du plan de relèvement. -

Post-Cairo Reproductive Health Policies and Programs: a Study of Five Francophone African Countries
The POLICY Project Justine Tantchou Ellen Wilson Post-Cairo Reproductive Health Policies and Programs: A Study of Five Francophone African Countries August 2000 Photo Credits All photos are printed with permission from the JHU/Center for Communication Programs. Post-CairoPost-Cairo ReproductiveReproductive HealthHealth PoliciesPolicies andand Programs:Programs: AA StudyStudy ofof FiveFive FrancophoneFrancophone AfricanAfrican CountriesCountries IntroductionIntroduction situation regarding reproductive health. In addition, given that all respondents are Since the ICPD in 1994, reproductive prominent in the reproductive health field, health has been a focus of health programs their perspectives actually influence the worldwide. Many countries have worked development of policies and programs in to revise reproductive health policy in their respective countries. accordance with the ICPD Programme of In each country, two to three members Action. In 1997, POLICY conducted case of the Reproductive Health Research studies in eight countries—Bangladesh, Committee—the country’s local branch of Ghana, India, Jamaica, Jordan, Nepal, RESAR—conducted the study. Research Peru, and Senegal—to examine field teams included at least one medical experiences in developing and specialist and one social science specialist. implementing reproductive health policies. The team carried out the fieldwork for the In 1998, RESAR conducted similar case case studies between October and studies in five Francophone African countries—Benin, Burkina Faso, Cameroon, Côte d’Ivoire, and Mali. RESAR’s purpose in conducting the studies was not to provide quantitative measurements of reproductive health indicators or an exhaustive inventory of reproductive health laws and policies but to improve understanding of reproductive health policy formulation and implementation. The study was qualitative, drawing on the perspectives of key informants—individuals who play an important role in formulating and implementing reproductive health policies and plans. -

Les Communes Du Benin En Chiffres
REPUBLIQUE DU BENIN Fraternité – Justice -Travail ********** COMMISSION NATIONALE DES FINANCES LOCALES ********** SECRETARIAT PERMANENT LES COMMUNES DU BENIN EN CHIFFRES 2010 IMAGE LES COMMUNES DU BENIN EN CHIFFRES 2010 1 Préface Les collectivités territoriales les ressources liées à leurs compétences et jusque- un maillon important dans le ministériels, participe de cette volonté de voir les développementdécentralisées sontde la Nation. aujourd’hui La communeslà mises disposer en œuvre de ressources par les départements financières volonté de leur mise en place suffisantes pour assumer la plénitude des missions qui sont les leurs. des Forces Vives de la Nation de février 1990. Les Si en 2003, au début de la mise en effective de la articles 150, 151,remonte 152 et 153à l’historique de la Constitution Conférence du 11 décembre 1990 a posé le principe de leur libre aux Communes représentaient environ 2% de leursdécentralisation, recettes de les fonctionnementtransferts financiers et de5% l’Etat en décentralisation dont les objectifs majeurs sont la promotionadministration de consacrantla démocratie ainsi l’avènementà la base etde lela transferts ont sensiblement augmenté et développement local. représententmatière d’investissement, respectivement 13%aujourd’hui et 73%. En cesdix Depuis dix (10) ans déjà, nos collectivités administration de leur territoire, assumant ainsi environ quatreans vingtd’expérience (80) milliards en matière de F CFA deen lesterritoriales missions quivivent sont l’apprentissage les leurs. Ces missionsde la libre ne dehorsdécentralisation, des interventions l’Etat a transféré directes auxréalisées communes dans sont guère aisées surtout au regard des ces communes. multiples et pressants besoins à la base, face aux ressources financières souvent limitées. doiventCes efforts en prendrede l’Etat la qui mesure se poursuivront pour une utilisation sans nul YAYI Bon a bien pri sainedoute etméritent transparente d’être de salués ces ressources. -

BENIN FY2020 Annual Work Plan
USAID’s Act to End NTDs | West Benin FY20 WORK PLAN USAID’s Act to End Neglected Tropical Diseases | West Program BENIN FY2020 Annual Work Plan Annual Work Plan October 1, 2019 to September 30, 2020 1 USAID’s Act to End NTDs | West Benin FY20 WORK PLAN Contents ACRONYM LIST ............................................................................................................................................... 3 NARRATIVE ..................................................................................................................................................... 6 1. National NTD Program Overview....................................................................................................... 6 2. IR1 PLANNED ACTIVITIES: LF, TRA, OV ............................................................................................... 8 i. Lymphatic Filariasis ........................................................................................................................ 8 ii. Trachoma ..................................................................................................................................... 12 iii. Onchocerciasis ............................................................................................................................. 14 3. SUSTAINABILITY STRATEGY ACTIVITIES (IR2 and IR3) ...................................................................... 16 i. DATA SECURITY AND MANAGEMENT .......................................................................................... 16 ii.