Caffeine Citrate Improves Outcomes of Apnea of Prematurity Based on Gestational Ages
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effect of Aminophylline on Diaphragmatic Contractility in the Piglet
003 1-3998/90/2803-0196$02.00/0 PEDIATRIC RESEARCH Vol. 28, No. 3, 1990 Copyright 0 1990 International Pediatric Research Foundation, Inc. Printed in (I.S.A. Effect of Aminophylline on Diaphragmatic Contractility in the Piglet DENNIS E. MAYOCK, THOMAS A. STANDAERT, JON F. WATCHKO, AND DAVID E. WOODRUM1 University of Washington School of Medicine, Department of Pediatrics, Division of Neonatal and Respiratory Diseases, Seattle, Washington 98195 ABSTRACT. Minute ventilation, arterial blood gases, ar- of arterial oxygen > 8 kPa (60 torr) in room air, and a partial terial pH, cardiac output, and transdiaphragmatic force pressure of the arterial carbon dioxide 5 6.7 kPa (50 torr) were generation, both during spontaneous ventilation and in accepted for study. The animals were anesthetized with an i.v. response to phrenic nerve stiwulation during airway occlu- combination of chloralose (30 mg/kg) and urethane (1 50 mg/ sion at end expiration, were measured in nine anesthetized, kg) and studied in the supine position. Subsequent infusions of tracheostomized piglets before and 30 min after parenteral anesthetic were used if the piglet developed jaw clonus. A trache- infusion of 20 mg/kg aminophylline. Serum theophylline ostomy was placed and connected to a two-way nonrebreathing levels averaged 109 f 21 ~mol/L(19.7 f 3.7 ~g/mL)at valve (model 2384, Hans Rudolph, Inc., Kansas City, MO). 30 min postinfusion. No significant changes were noted in Inspiratory flow was detected by a hot-wire anemometer and pH, blood gases, blood Pressure, or ventilatory measures integrated to provide tidal volume. All animals breathed 50% after aminophylline. -

Aminophylline Catalog Number A1755 Storage
Aminophylline Catalog Number A1755 Storage Temperature –20 °C Replacement for Catalog Number 216895 CAS RN 317-34-0 Storage/Stability Synonyms: theophylline hemiethylenediamine complex; Aminophylline should be kept tightly closed to prevent 3,7-dihydro-1,3-demethyl-1H-purine-2,6-dione CO2 absorption from the atmosphere, which leads to compound with 1,2-ethanediamine (2:1); formation of theophylline and decreased solubility in 1,2 3 (theophylline)2 • ethylenediamine aqueous solutions. Stock solutions should be protected from light and prevented from contact with Product Description metals.2 Molecular Formula: C7H8N4O2 ·1/2 (C2H8N2) Molecular Weight: 210.3 References 1. The Merck Index, 12th ed., Entry# 485. Aminophylline is a xanthine derivative which is a 2. Martindale: The Extra Pharmacopoeia, 31st ed., combination of theophylline and ethylenediamine that is Reynolds, J. E. F., ed., Royal Pharmaceutical more water soluble than theophylline alone. Society (London, England: 1996), pp. 1651-1652. Aminophylline has been widely used as an inhibitor of 3. Data for Biochemical Research, 3rd ed., Dawson, cAMP phosphodiesterase.3 R. M. C., et al., Oxford University Press (New York, NY: 1986), pp. 316-317. Aminophylline has been shown to limit 4. Pelech, S. L., et al., cAMP analogues inhibit phosphatidylcholine biosynthesis in cultured rat phosphatidylcholine biosynthesis in cultured rat hepatocytes.4 It has been used in studies of acute hepatocytes. J. Biol. Chem., 256(16), 8283-8286 hypoxemia in newborn and older guinea pigs.5 The (1981). effect of various xanthine derivatives, including 5. Crisanti, K. C., and Fewell, J. E., Aminophylline aminophylline, on activation of the cystic fibrosis alters the core temperature response to acute transmembrane conductance regulator (CFTR) chloride hypoxemia in newborn and older guinea pigs. -

Rosemary)-Derived Ingredients As Used in Cosmetics
Safety Assessment of Rosmarinus Officinalis (Rosemary)-Derived Ingredients as Used in Cosmetics Status: Tentative Amended Report for Public Comment Release Date: March 28, 2014 Panel Meeting Date: June 9-10, 2014 All interested persons are provided 60 days from the above release date to comment on this safety assessment and to identify additional published data that should be included or provide unpublished data which can be made public and included. Information may be submitted without identifying the source or the trade name of the cosmetic product containing the ingredient. All unpublished data submitted to CIR will be discussed in open meetings, will be available at the CIR office for review by any interested party and may be cited in a peer-reviewed scientific journal. Please submit data, comments, or requests to the CIR Director, Dr. Lillian J. Gill. The 2014 Cosmetic Ingredient Review Expert Panel members are: Chairman, Wilma F. Bergfeld, M.D., F.A.C.P.; Donald V. Belsito, M.D.; Ronald A. Hill, Ph.D.; Curtis D. Klaassen, Ph.D.; Daniel C. Liebler, Ph.D.; James G. Marks, Jr., M.D.; Ronald C. Shank, Ph.D.; Thomas J. Slaga, Ph.D.; and Paul W. Snyder, D.V.M., Ph.D. The CIR Director is Lillian J. Gill, D.P.A. This safety assessment was prepared by Monice M. Fiume, Assistant Director/Senior Scientific Analyst. © Cosmetic Ingredient Review 1620 L Street, NW, Suite 1200♢ Washington, DC 20036 ♢ ph 202.331.0651 ♢ fax 202.331.0088 ♢ [email protected] TABLE OF CONTENTS Abstract ...................................................................................................................................................................................................................................... -
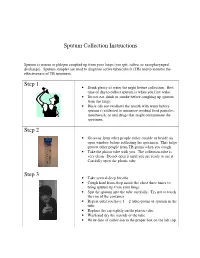
Sputum Collection Instructions Step 1 Step 2 Step 3
Sputum Collection Instructions Sputum is mucus or phlegm coughed up from your lungs (not spit, saliva, or nasopharyngeal discharge). Sputum samples are used to diagnose active tuberculosis (TB) and to monitor the effectiveness of TB treatment. Step 1 • Drink plenty of water the night before collection. Best time of day to collect sputum is when you first wake. • Do not eat, drink or smoke before coughing up sputum from the lungs. • Rinse (do not swallow) the mouth with water before sputum is collected to minimize residual food particles, mouthwash, or oral drugs that might contaminate the specimen. Step 2 • Go away from other people either outside or beside an open window before collecting the specimen. This helps protect other people from TB germs when you cough. • Take the plastic tube with you. The collection tube is very clean. Do not open it until you are ready to use it. Carefully open the plastic tube. Step 3 • Take several deep breaths. • Cough hard from deep inside the chest three times to bring sputum up from your lungs. • Spit the sputum into the tube carefully. Try not to touch the rim of the container. • Repeat until you have 1 – 2 tablespoons of sputum in the tube. • Replace the cap tightly on the plastic tube. • Wash and dry the outside of the tube. • Write date of collection in the proper box on the lab slip. Step 4 • Place the primary specimen container (usually a conical centrifuge tube) in the clear plastic baggie that has the biohazard symbol imprint. • Place the white absorbent sheet in the plastic baggie. -

Perinatal/Neonatal Case Presentation
Perinatal/Neonatal Case Presentation &&&&&&&&&&&&&& Urinary Tract Infection With Trichomonas vaginalis in a Premature Newborn Infant and the Development of Chronic Lung Disease David J. Hoffman, MD vaginal bleeding with suspected abruption resulted in delivery of Gerard D. Brown, DO the infant by Cesarean section. The Apgar scores were 1, 5, and 9 Frederick H. Wirth, MD at 1, 5, and 10 minutes of life, respectively. Betsy S. Gebert, CRNP After delivery, the infant was managed with mechanical Cathy L. Bailey, MS, CRNP ventilation with pressure support and volume guarantee for Endla K. Anday, MD respiratory distress syndrome. She received exogenous surfactant We report a case of a low-birth-weight infant with an infection of the urinary tract with Trichomonas vaginalis, who later developed cystic chronic lung disease suggestive of Wilson-Mikity syndrome. Although she had mild respiratory distress syndrome at birth, the extent of the chronic lung disease was out of proportion to the initial illness. We speculate that maternal infection with this organism may have resulted in an inflammatory response that led to its development. Journal of Perinatology (2003) 23, 59 – 61 doi:10.1038/sj.jp.7210819 CASE PRESENTATION A 956-g, appropriate-for-gestational-age, African–American female was delivered by Cesarean section following 27 5/7 weeks of gestation in breech presentation after a period of advanced cervical dilatation and uterine contractions. Her mother was a 20-year-old gravida 5, para 2022 woman whose prenatal laboratory data were significant for vaginal colonization with Streptococcus agalactiae, treatment for Chlamydia trachomatis, and a history of cocaine and marijuana usage confirmed by urine toxicology. -

Download Product Insert (PDF)
PRODUCT INFORMATION Proxyphylline Item No. 20937 CAS Registry No.: 603-00-9 Formal Name: 3,7-dihydro-7-(2-hydroxypropyl)-1,3- N dimethyl-1H-purine-2,6-dione O N Synonym: NSC 163343 C H N O MF: 10 14 4 3 N FW: 238.2 N Purity: ≥98% O UV/Vis.: λmax: 273, 324 nm Supplied as: A crystalline solid OH Storage: -20°C Stability: As supplied, 2 years from the QC date provided on the Certificate of Analysis, when stored properly Laboratory Procedures Proxyphylline is supplied as a crystalline solid. A stock solution may be made by dissolving the proxyphylline in the solvent of choice. Proxyphylline is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF), which should be purged with an inert gas. The solubility of proxyphylline in ethanol is approximately 1 mg/ml and approximately 10 mg/ml in DMSO and DMF. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of proxyphylline can be prepared by directly dissolving the crystalline solid in aqueous buffers. The solubility of proxyphylline in PBS, pH 7.2, is approximately 1 mg/ml. We do not recommend storing the aqueous solution for more than one day. Description Proxyphylline is a methylxanthine derivative that has bronchodilatory actions.1 It has also been reported 2 to have vasodilatory and cardiac stimulatory effects. -

Caffeine Versus Aminophylline for Apnea of Prematurity: a Randomized Clinical Trial
World Journal of Peri & Neonatology Vol. 2, No. 2, Fall 2019 Original Article http://wjpn.ssu.ac.ir Caffeine versus Aminophylline for Apnea of Prematurity: A Randomized Clinical Trial Mohamad Hosein Lookzadeh 1,2, Elaha Jafari-Abeshoori 2*, Mahmood Noorishadkam 1,2, Seyed Reza Mirjalili 1,2, Hamid Reza Mohammadi 3, Fatemeh Emambakhshsani 2 1 Department of Pediatrics, Shahid Sadoughi University of Medical Sciences, Yazd, Iran 2 Mother and Newborn Health Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran 3 Cardiovascular Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran Received: 04 April 2020 Revised: 16 June 2020 Accepted: 20 July 2020 ARTICLE INFO ABSTRACT Corresponding author: Background: Apnea of prematurity is often found in preterm neonates Elaha Jafari-Abeshoori with gestational age less than 34-37 weeks or birth weight (BW) less than 1000 grams. The American Academy of Pediatrics defines apnea as a Email: [email protected] respiratory halt lasting at least 20 seconds, with bradycardia or cyanosis. Methylxanthines reduce the incidence of apnea. The purpose of this study Keywords: was to compare the effect of caffeine and aminophylline on the incidence Aminophylline, of the apnea in premature infants. Caffeine, Methods: This randomized clinical trial study was conducted on 80 Apnea, premature neonates at Shahid Sadoughi hospital in Yazd. The first group Prematurity received the initial dose of 5 mg/kg aminophylline diluted in 5% dextrose with a maintenance dose of 2 mg/kg every 8 hours, while the second group received 30 mg/kg of caffeine diluted in 5% dextrose with a 24-hour maintenance dose of 10 mg/kg. -

The Xanthines (Theobromine and Aminophyllin)
effect of this might conceivably escape detection in THE XANTHINES (THEOBROMINE AND individuals engaged in very heavy work. From this AMINOPHYLLINE) IN THE TREAT- point of view our subjects were particularly favorable for this since of as MENT OF CARDIAC PAIN study, most them, shown in the table, were not engaged in any occupation. HARRY M.D. GOLD, GLYCERYL TRINITRATE TEST NATHANIEL T. M.D. KWIT, Early in the course of the study it was believed AND desirable to HAROLD M.D. restrict the selection of patients to those OTTO, who could establish their qualifications for service in NEW YORK such a study as this by their ability to distinguish An endeavor was made in this study to secure evi- between the efficacy of glyceryl trinitrate taken under dence on the question of whether the xanthines relieve the tongue and a soluble placebo tablet taken in the cardiac pain. same manner for relief during attacks of pain. The SELECTION OF PATIENTS discovery of several patients who found the two equally effective those who had suffered an of The were 100 ambulant in attend- among attack subjects patients thrombosis and were to thoracic ance at the cardiac in whom the of coronary subject pain clinic, diagnosis on effort led us to abandon this restriction. arteriosclerotic heart disease with cardiac pain was made, in accordance with the nomenclature and criteria The results obtained in sixty patients in whom the the New York Heart Association.1 glyceryl trinitrate test was made are of some interest. adopted by These received trinitrate were selected from a total case load of patients glyceryl tablets, %0o They approxi- or cr 0.4 which were mately 700 patients, representing an average sample /4so grain (0.6 mg.), they of the cardiac clinic several racial directed to take under the tongue at the onset of an population, comprising attack of In of these of groups, both native and born. -

Chest Pain in Pediatrics
PEDIATRIC CARDIOLOGY 0031-3955/99 $8.00 + .OO CHEST PAIN IN PEDIATRICS Keith C. Kocis, MD, MS Chest pain is an alarming complaint in children, leading an often frightened and concerned family to a pediatrician or emergency room and commonly to a subsequent referral to a pediatric cardiologist. Because of the well-known associ- ation of chest pain with significant cardiovascular disease and sudden death in adult patients, medical personnel commonly share heightened concerns over pediatric patients presenting with chest pain. Although the differential diagnosis of chest pain is exhaustive, chest pain in children is least likely to be cardiac in origin. Organ systems responsible for causing chest pain in children include*: Idiopathic (12%-85%) Musculoskeletal (15%-31%) Pulmonary (12%-21%) Other (4%-21%) Psychiatric (5%-17%) Gastrointestinal (4'/0-7%) Cardiac (4%4%) Furthermore, chest pain in the pediatric population is rareZy associated with life-threatening disease; however, when present, prompt recognition, diagnostic evaluation, and intervention are necessary to prevent an adverse outcome. This article presents a comprehensive list of differential diagnostic possibilities of chest pain in pediatric patients, discusses the common causes in further detail, and outlines a rational diagnostic evaluation and treatment plan. Chest pain, a common complaint of pediatric patients, is often idiopathic in etiology and commonly chronic in nature. In one study,67 chest pain accounted for 6 in 1000 visits to an urban pediatric emergency room. In addition, chest pain is the second most common reason for referral to pediatric cardiologist^.^, 23, 78 Chest pain is found equally in male and female patients, with an average *References 13, 17, 23, 27, 32, 35, 44, 48, 49, 63-67, 74, and 78. -

Intravenous Aminophylline Treatment for Migraine
Original Observations and Research Personal Observation: Intravenous Aminophylline Treatment for Migraine Michael Kenyon MD, Barry Phillips MD, Christiaan DeWit MBBCh About the Authors Michael Kenyon (near right) and Barry Phillips (far right) are internists, and Christiaan De Wit is an emergency room physician, all practising at Mills Memorial Hospital, in Terrace, British Columbia. Correspondence may be directed to: [email protected] igraine is common condition, often affecting young inhibitor and adenosine antagonist. It has been shown in Mpatients and causing disruption in the home and dipyridamole (Persantine) MIBI studies that dipyridamole workplace alike. The impact of patients presenting to administration inhibits adenosine deaminase in red-cell emergency room services with intractable headache is membranes, increasing blood levels of adenosine. This induces significant, often tying up space and resources in the tedious coronary vasodilation through a low-affinity interaction with wait for a narcotic and sedative “cure.” In Canada alone, 3.2 the A2a receptor. The antidote, aminophylline, preferentially million adults suffer from migraines, and the condition costs binds to this receptor, displacing adenosine and curtailing its the Canadian economy an estimated $500 million annually. effect. 3,4 Absenteeism and loss of productivity resulting from migraines Aminophylline has traditionally and principally been used cost $20 every second. 1 as an intravenously or orally administered bronchodilator in Mills Memorial Hospital is a regional referral centre in asthmatics. Caution in its use should be observed in patients Terrace, British Columbia, serving a population of 70,000 with active peptic ulceration, a low seizure threshold, people. Between June 2011 and January 2012, 21 patients came hypokalemia, tachyarrhythmias, and acute congestive heart to the emergency room (ER) suffering from symptoms failure (CHF). -

Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT
University of Nebraska Medical Center DigitalCommons@UNMC Theses & Dissertations Graduate Studies Fall 12-18-2015 Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT Christopher C. Schultz University of Nebraska Medical Center Follow this and additional works at: https://digitalcommons.unmc.edu/etd Part of the Other Medical Specialties Commons Recommended Citation Schultz, Christopher C., "Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT" (2015). Theses & Dissertations. 54. https://digitalcommons.unmc.edu/etd/54 This Thesis is brought to you for free and open access by the Graduate Studies at DigitalCommons@UNMC. It has been accepted for inclusion in Theses & Dissertations by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. EVALUATION OF UPPER AIRWAY CHANGES FOLLOWING SURGICAL REMOVAL OF THE ADENOIDS USING 3-D CONE BEAM CT By Christopher C. Schultz, D.D.S A THESIS Presented to the Faculty of The Graduate College in the University of Nebraska In Partial Fulfillment of Requirements For the Degree of Master of Science Medical Sciences Interdepartmental Area Oral Biology University of Nebraska Medical Center Omaha, Nebraska December, 2015 Advisory Committee: Sundaralingam Premaraj, BDS, MS, PhD, FRCD(C) Sheela Premaraj, BDS, PhD Peter J. Giannini, DDS, MS Stanton D. Harn, PhD i ACKNOWLEDGEMENTS I would like to express my thanks and gratitude to the members of my thesis committee: Dr. Sundaralingam Premaraj, Dr. Sheela Premaraj, Dr. Peter Giannini, and Dr. Stanton Harn. Your advice and assistance has been vital for the completion of the project. -

Pjp1'2003.Vp:Corelventura
Copyright © 2003 by Institute of Pharmacology Polish Journal of Pharmacology Polish Academy of Sciences Pol. J. Pharmacol., 2003, 55, 103107 ISSN 1230-6002 SHORT COMMUNICATION INFLUENCE OF LY 300164, AN AMPA/KAINATE RECEPTOR ANTAGONIST UPON THE ANTICONVULSANT ACTION OF ANTIEPILEPTIC DRUGS AGAINST AMINOPHYLLINE-INDUCED SEIZURES IN MICE Mariusz Œwi¹der1, Hubert KuŸniar1, Zdzis³aw Kleinrok1 , Stanis³aw J. Czuczwar2,3,# Department of Pharmacology and Toxicology, Department of Pathophysiology, Medical University, Jaczewskiego 8, PL 20-090 Lublin, !Isotope Laboratory, Institute of Agricultural Medicine, Jaczewskiego 2, PL 20-950 Lublin, Poland Influence of LY 300164, an AMPA/kainate receptor antagonist, upon the anticonvulsant action of antiepileptic drugs against aminophylline-induced seizures in mice. M. ŒWI¥DER, H. KUNIAR, Z. KLEINROK , S.J. CZU- CZWAR. Pol. J. Pharmacol., 2003, 55, 103–107. LY 300164 {7-acetyl-3-(4-aminophenyl)-8,9-dihydro-8-methyl-7H-1,3- dioxazolo[4,5-h] [2,3]-benzodiazepine}, a novel AMPA/kainate receptor an- tagonist, administered intraperitoneally protected mice against aminophyl- line-induced seizures. At doses up to 0.5 mg/kg, which did not significantly affect the convulsant activity of aminophylline, it potentiated the protective activity of diazepam. On the other hand, LY 300164 used at the lowest pro- tective dose of 1.0 mg/kg enhanced anticonvulsant activity of all antiepilep- tic drugs tested in this seizure model. However, LY 300164 neither alone nor combined with antiepileptic drugs, reduced aminophylline-induced mortality. Key words: antiepileptic drugs, LY 300164, aminophylline-induced sei- zures correspondence; e-mail: [email protected] M. Œwi¹der, H. KuŸniar, Z.