Comparison of Local Cytokine Gene Expression and the Distribution Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of Ansel in Tracy Letts' Killer Joe: a Production Thesis in Acting
Louisiana State University LSU Digital Commons LSU Master's Theses Graduate School 2003 The oler of Ansel in Tracy Letts' Killer Joe: a production thesis in acting Ronald William Smith Louisiana State University and Agricultural and Mechanical College Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_theses Part of the Theatre and Performance Studies Commons Recommended Citation Smith, Ronald William, "The or le of Ansel in Tracy Letts' Killer Joe: a production thesis in acting" (2003). LSU Master's Theses. 3197. https://digitalcommons.lsu.edu/gradschool_theses/3197 This Thesis is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Master's Theses by an authorized graduate school editor of LSU Digital Commons. For more information, please contact [email protected]. THE ROLE OF ANSEL IN TRACY LETTS’ KILLER JOE: A PRODUCTION THESIS IN ACTION A Thesis Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the Requirements for the degree of Master of Fine Arts in The Department of Theatre by Ronald William Smith B.S., Clemson University, 2000 May 2003 Acknowledgements I would like to thank my professors, Bob and Annmarie Davis, Jo Curtis Lester, Nick Erickson and John Dennis for their knowledge, dedication, and care. I would like to thank my classmates: Deb, you are a friend and I’ve learned so much from your experiences. Fire, don’t ever lose the passion you have for life and art, it is beautiful and contagious. -

FY16 Purchase Orders
PO Numbe PO Date Quantity Unit Price PO Description Vendor Name Vendor Address1 Vendor City Vendor StateVendor Zip 16000001 07/01/2015 1.00$ 135.00 Chesapeake Waste CHESAPEAKE WASTE IND LLC PO BOX 2695 SALISBURY MD 21802 16000002 07/01/2015 1.00$ 204.67 FOR BID AWARD MAILING SERVICES MAIL MOVERS PO BOX 2494 SALISBURY MD 21802-2494 16000002 07/01/2015 1.00$ 7,000.00 FOR BID AWARD MAILING SERVICES MAIL MOVERS PO BOX 2494 SALISBURY MD 21802-2494 16000003 07/01/2015 1.00$ 260.00 BLANKET PO FOR MEMBERSHIP DUES CLIENT PROTECTION FUND OF THE BAR OF MD 200 HARRY S TRUMAN PKWY ANNAPOLIS MD 21401 16000004 07/01/2015 1.00$ 5,000.00 BLANKET PO FOR INSURANCE DEDUC LOCAL GOVERNMENT INS TRUST 7225 PARKWAY DR HANOVER MD 21076 16000005 07/01/2015 1.00$ 350.00 BLANKET PO FOR MEMBERSHIP DUES MD STATE BAR ASSOCIATION PO BOX 64747 BALTIMORE MD 21264-4747 16000006 07/01/2015 1.00$ 115,433.00 Replacement Chiller THE TRANE COMPANY PO BOX 406469 ATLANTA GA 30384 16000007 07/01/2015 1.00$ 500.00 BLANKET PO FOR LEGAL ADVERTISI THE DAILY TIMES PO BOX 742621 CINCINNATI OH 45274-2621 16000008 07/01/2015 1.00$ 5,000.00 BLANKET PO FOR INSURANCE DEDUC TRAVELERS 13607 COLLECTIONS CENTER DR CHICAGO IL 60693 16000009 07/01/2015 1.00$ 6,325.00 BLANKET PO FOR LEGAL DATABASE THOMSON REUTERS-WEST PUBLISHING CORP WEST PAYMENT CENTER CAROL STREAM IL 60197-6292 16000010 07/01/2015 1.00$ 100.00 BLANKET PO FOR MEMBERSHIP DUES WICOMICO COUNTY BAR ASSOCIATION PO BOX 4394 SALISBURY MD 21803-0389 16000011 07/01/2015 1.00$ 555.00 BLANKET PO FOR MEMBERSHIP DUES IMLA - INTERNATIONAL MUNICIPAL -

Permitting Activity 01/01/2020 Thru 8/2/2020 Date of Report: 08/03/2020 L-BUILD ONLY - Grouped by Type Then Subtype Page 1 of 228
Permitting Activity 01/01/2020 Thru 8/2/2020 Date of Report: 08/03/2020 L-BUILD ONLY - Grouped by Type then Subtype Page 1 of 228 Issued App. Permit Sq- Total Fees Date Status Number Sub Type Type Valuation Feet Contractor Owner Address Total Fees Due Commercial Permits: Addition Permits: LB2000140 Addition Commercial $30,000.00 518 L&L CONSTRUCTION SERVICESBANNERMAN LLC CROSSINGS II6668 LLC Thomasville Rd $287.46 $0.00 3/12/20 Issued LB2000383 Addition Commercial $95,000.00 2800 COMMERCIAL REPAIR & RENOVATIONSWESTON TRAWICK INC. INC 5392 Tower Rd $1,954.57 $0.00 5/7/20 Issued LB2000386 Addition Commercial $17,000.00 748 ADVANCED AWNING & DESIGN,JNC REALTY LLC ENTERPRISES6800 INC Thomasville Rd, Ste 106 $412.88 $0.00 4/20/20 Issued Addition Totals: 3 $142,000.00 $2,654.91 $0.00 Alteration Permits: LB1801185 Alteration Commercial $12,000.00 BETACOM INCORPORATEDTALL TIMBERS RESEARCH, 4000INC County Rd 12 $224.17 $0.00 2/10/20 Issued LB1802065 Alteration Commercial $40,000.00 4021 HILL DEVELOPMENT MANAGEMENT,NGUYEN LOAN LLC T 4979 Blountstown Hwy $3,917.67 $0.00 3/11/20 Issued LB1900627 Alteration Commercial $75,000.00 THE DEEB COMPANIES CAMELLIA OAKS LLC 4330 Terebinth Trl $2,377.76 $0.00 5/5/20 Certificate of Occupancy LB1901330 Alteration Commercial $250,000.00 SOUTHEAST INDUSTRIAL RENTALCOLE CS AND TALLAHASSEE CLEANING FL INC 4067LLC Lagniappe Way $3,090.38 $0.00 2/3/20 Issued LB1901550 Alteration Commercial $200,000.00 WSD ENGINEERING GLOBAL SIGNAL ACQUISITIONS2008 IV Mckee LLC Rd $2,548.65 $0.00 6/9/20 Issued LB1901889 Alteration Commercial $56,050.00 1120 TAYLOR CONSTRUCTION &3219 RENOVATION TALLAHASSEE LLC 3219 N Monroe St $1,981.57 $0.00 2/17/20 Issued LB1902034 Alteration Commercial $20,632.00 2008 CHAPMAN CANOPY INCORPORATEDRIVERS RD EXPRESS #15 LLC6330 Crawfordville Rd $1,827.13 $0.00 2/5/20 Issued LB1902154 Alteration Commercial $20,000.00 SAC WIRELESS LLC CROWN CASTLE USA 1478 Capital Cir NW $568.64 $0.00 2/26/20 Issued LB1902168 Alteration Commercial $400,000.00 OLIVER SPERRY RENOVATIONLEON AND COUNTY CONSTRUCTION,1583 INC. -

Ansel Adams in the Human and Natural Environments of Yosemite
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Journal of the National Collegiate Honors Council --Online Archive National Collegiate Honors Council Spring 2005 Seeing Nature: Ansel Adams in the Human and Natural Environments of Yosemite Megan McWenie University of Arizona, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/nchcjournal Part of the Higher Education Administration Commons McWenie, Megan, "Seeing Nature: Ansel Adams in the Human and Natural Environments of Yosemite" (2005). Journal of the National Collegiate Honors Council --Online Archive. 161. https://digitalcommons.unl.edu/nchcjournal/161 This Article is brought to you for free and open access by the National Collegiate Honors Council at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Journal of the National Collegiate Honors Council --Online Archive by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Portz-Prize-Winning Essay, 2004 55 SPRING/SUMMER 2005 56 JOURNAL OF THE NATIONAL COLLEGIATE HONORS COUNCIL MEGAN MCWENIE Portz Prize-Winning Essay, 2004 Seeing Nature: Ansel Adams in the Human and Natural Environments of Yosemite MEGAN MCWENIE UNIVERSITY OF ARIZONA allace Stegner once hailed the legacy of Ansel Adams as bringing photography Wto the world of art as a unique “way of seeing.”1 What Adams saw through the lens of his camera, and what audiences see when looking at one of his photographs, does indeed constitute a particular way of seeing the world, a vision that is almost always connected to the natural environment. An Ansel Adams photograph evokes more than an aesthetic response to his work—it also stirs reflections about his involvement in the natural world that was so often his subject. -

Ansel Adams Wilderness Bass Lake Ranger District
PACIFIC SOUTHWEST REGION Restoring, Enhancing and Sustaining Forests in California, Hawaii and the Pacific Islands Sierra National Forest Ansel Adams Wilderness Bass Lake Ranger District The Ansel Adams Wilderness is a diverse and Southern portions of the Wilderness provide forests spectacular area comprised of 228,500 acres of huge pine and fir where few people visit. draped along the crest of the Sierra Nevada Highway 41 and 168 access western slope trail- within the Sierra and Inyo National Forests. This heads while Highways 120 (Tioga Pass through Yo- wilderness ecosystem includes a number of lake semite National Park) and Highway 395 access trail- and stream systems that are the headwaters of the heads on the East side of the Sierra. San Joaquin River. Vegetation is mixed conifer- Commercial pack stations provide services from ous and deciduous forests of pine and oak in low Agnew and Reds Meadow (Inyo National Forest) on elevation, and sub-alpine forests of lodgepole the eastern side of the range, and from Miller pine, mountain hemlock and red fir. Alpine Meadow and Florence and Edison Lakes (Sierra Na- meadows grace the higher elevations with wild- tional Forest) on the western slope. flowers and crystal streams. Elevations range from hot dry canyons at REGULATIONS AND PERMIT REQUIRE- 3,500 feet in the San Joaquin River gorge to MENTS 13,157 foot Mount Ritter. Precipitation is from A wilderness Visitor Permit is required for all over- 18 to 50 inches, with snow depth averages about night trips into the wilderness. Important travel in- 171 inches. formation is available concerning bear encounters, The John Muir Trail, which starts in Yosem- fire danger, current weather, snow and hazard condi- ite National Park, crosses Donahue Pass (11,056 tions, and to assist visitors in understanding how to feet), into the Ansel Adams Wilderness and south properly use the wilderness and leave no trace. -
GEDCOM 5.5.2 With
THE GEDCOM SPECIFICATION Includes GEDXML format DRAFT Release 5.6 Prepared by the Family History Department The Church of Jesus Christ of Latter-day Saints 18 December 2000 Suggestions and Correspondence: Email: Mail: [email protected] Family History Department GEDCOM Coordinator—3T Telephone: 50 East North Temple Street 801-240-4534 Salt Lake City, UT 84150 801-240-3442 USA Copyright © 2000 by The Church of Jesus Christ of Latter-day Saints. This document may be copied for purposes of review or programming of genealogical software, provided this notice is included. All other rights reserved. TABLE OF CONTENTS Introduction ................................................................................. 5 Purpose and Content of The GEDCOM Standard ................................................. 5 Purposes for Version 5.x ................................................................... 6 Modifications in Version 5.6 ................................................................ 6 Chapter 1 Data Representation Grammar ............................................................... 9 Concepts ............................................................................... 9 Grammar .............................................................................. 10 Description of Grammar Components ........................................................ 14 Chapter 2 Lineage-Linked Grammar ................................................................. 19 Record Structures of the Lineage-Linked Form ................................................ -

Ansi Z39.47-1985
ANSI® * Z39.47-1985 ISSN: 8756-0860 American National Standard for Information Sciences - Extended Latin Alphabet Coded Character Set for Bibliographic Use Secretariat Council of National Library and Information Associations Approved September 4, 1984 American National Standards Institute, Inc Abstract This standard establishes computer codes for an extended Latin alphabet character set to be used in bibliographic work when handling non-English items. This standard establishes the 7-bit and 8-bit code values. 3 sawvwn nkhhoiw jo umMm im Generated on 2013-01-28 18:16 GMT / http://hdl.handle.net/2027/mdp.39015079886241 Public Domain, Google-digitized / http://www.hathitrust.org/access_use#pd-google Por^XA/OrH fW* Foreword is not part of American National Standard Z39.47-1985.) This standard for the extended Latin alphabet coded character set for bibliographic use l\ <-. was developed by Subcommittee N on Coded Character Sets for Bibliographic Informa- tion Interchange of the American National Standards Committee on Library and Informa- tion Sciences and Related Publishing Practices, Z39, now the National Information Stan- . dards Organization (Z39). / L O I The codes given in this standard may be identified by the use of the notation ANSEL. The notation ANSEL should be taken to mean the codes prescribed by the latest edition of this standard. To explicitly designate a particular edition, the last two digits of the year of the issue may be appended, as in ANSEL 85. The standard establishes both the 7-bit and the 8-bit code values for the computer codes for characters used in bibliographic work when handling non-English items. -
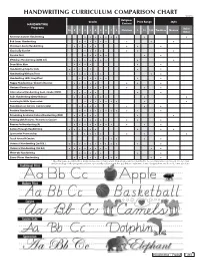
Handwriting Curriculum Comparison Chart
HANDWRITING CURRICULUM COMPARISON CHART ©2018 Religious Grades Price Range Style HANDWRITING Content Programs Italic/ PK K 1 2 3 4 5 6 7 8 Christian $ $$ $$$ Tradition Modern Other American Cursive Handwriting • • • • • • • • • Bob Jones Handwriting • • • • • • • • • Christian Liberty Handwriting • • • • • • • • Classically Cursive • • • • • • • Cursive First • • • • • • • D'Nealian Handwriting (2008 ed.) • • • • • • • • • Draw Write Now • • • • • • Handwriting Help for Kids • • • • • • • Handwriting Without Tears • • • • • • • • • Handwriting Skills Simplified • • • • • • • • Happy Handwriting / Cheerful Cursive • • • • • • • • Horizons Penmanship • • • • • • • • • International Handwriting Cont. Stroke (HMH) • • • • • • • Italic Handwriting (Getty-Dubay) • • • • • • • • • Learning to Write Spencerian • • • • • • • • • New American Cursive (cursive only) • • • • • • • Pentime Handwriting • • • • • • • • • • • Preventing Academic Failure Handwriting (PAF) • • • • • • • Printing with Pictures / Pictures in Cursive • • • • • • • • • • Reason for Handwriting (A) • • • • • • • • • • • Sailing Through Handwriting • • • • • • • • • Spencerian Penmanship • • • • • • • Teach Yourself Cursive • • • • • • Universal Handwriting (2nd Ed.) • • • • • • • • • • • • Universal Handwriting (3rd Ed.) • • • • • • • • • • Write-On Handwriting • • • • • • • Zaner-Bloser Handwriting • • • • • • • • • • • *This chart was assembled by Rainbow Resource Curriculum Consultants and is intended to be a comparative tool based on our own understanding of the programs -

Wise Men Make Proverbs Ten Minute Play
WISE MEN MAKE PROVERBS TEN MINUTE PLAY By Andy Haynes Copyright © MMXII by Andy Haynes All Rights Reserved Heuer Publishing LLC, Cedar Rapids, Iowa The writing of plays is a means of livelihood. Unlawful use of a playwright’s work deprives the creator of his or her rightful income. The playwright is compensated on the full purchase price and the right of performance can only be secured through purchase of at least four (4) copies of this work. PERFORMANCES ARE LIMITED TO ONE VENUE FOR ONE YEAR FROM DATE OF PURCHASE. The possession of this script without direct purchase from the publisher confers no right or license to produce this work publicly or in private, for gain or charity. On all programs and advertising this notice must appear: “Produced by special arrangement with Heuer Publishing LLC of Cedar Rapids, Iowa.” This dramatic work is fully protected by copyright. No part of this work may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without permission of the publisher. Copying (by any means) or performing a copyrighted work without permission constitutes an infringement of copyright. The right of performance is not transferable and is strictly forbidden in cases where scripts are borrowed or purchased second hand from a third party. All rights including, but not limited to the professional, motion picture, radio, television, videotape, broadcast, recitation, lecturing, tabloid, publication, and reading are reserved. COPYING OR REPRODUCING ALL OR ANY PART OF THIS BOOK IN ANY MANNER IS STRICTLY FORBIDDEN BY LAW. -
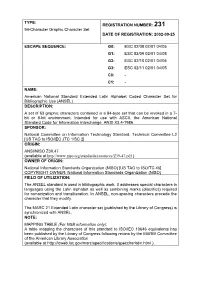
TYPE: 94-Character Graphic Character Set REGISTRATION
TYPE: REGISTRATION NUMBER: 231 94-Character Graphic Character Set DATE OF REGISTRATION: 2002-09-25 ESCAPE SEQUENCE: G0: ESC 02/08 02/01 04/05 G1: ESC 02/09 02/01 04/05 G2: ESC 02/10 02/01 04/05 G3: ESC 02/11 02/01 04/05 C0: - C1: - NAME: American National Standard Extended Latin Alphabet Coded Character Set for Bibliographic Use (ANSEL) DESCRIPTION: A set of 63 graphic characters contained in a 94-byte set that can be invoked in a 7- bit or 8-bit environment. Intended for use with ASCII, the American National Standard Code for Information Interchange, ANSI X3.4-1986. SPONSOR: National Committee on Information Technology Standard, Technical Committee L2 [US TAG to ISO/IEC JTC 1/SC 2] ORIGIN: ANSI/NISO Z39.47 (available at http://www.niso.org/standards/resources/Z39-47.pdf ) OWNER OF ORIGIN: National Information Standards Organization (NISO) [US TAG to ISO/TC 46] COPYRIGHT OWNER: National Information Standards Organization (NISO) FIELD OF UTILIZATION: The ANSEL standard is used in bibliographic work. It addresses special characters in languages using the Latin alphabet as well as combining marks (diacritics) required for romanization and transliteration. In ANSEL, non-spacing characters precede the character that they modify. The MARC 21 Extended Latin character set (published by the Library of Congress) is synchronized with ANSEL. NOTE: MAPPING TABLE (For NSB information only): A table mapping the characters of this standard to ISO/IEC 10646 equivalents has been published by the Library of Congress following review by the MARBI Committee of the American Library Association (available at http://lcweb.loc.gov/marc/specifications/speccharlatin.html ). -

Red Hat Linux 6.0
Red Hat Linux 6.0 The Official Red Hat Linux Installation Guide Red Hat Software, Inc. Durham, North Carolina Copyright c 1995, 1996, 1997, 1998, 1999 Red Hat Software, Inc. Red Hat is a registered trademark and the Red Hat Shadow Man logo, RPM, the RPM logo, and Glint are trademarks of Red Hat Software, Inc. Linux is a registered trademark of Linus Torvalds. Motif and UNIX are registered trademarks of The Open Group. Alpha is a trademark of Digital Equipment Corporation. SPARC is a registered trademark of SPARC International, Inc. Products bearing the SPARC trade- marks are based on an architecture developed by Sun Microsystems, Inc. Netscape is a registered trademark of Netscape Communications Corporation in the United States and other countries. TrueType is a registered trademark of Apple Computer, Inc. Windows is a registered trademark of Microsoft Corporation. All other trademarks and copyrights referred to are the property of their respective owners. ISBN: 1-888172-28-2 Revision: Inst-6.0-Print-RHS (04/99) Red Hat Software, Inc. 2600 Meridian Parkway Durham, NC 27713 P. O. Box 13588 Research Triangle Park, NC 27709 (919) 547-0012 http://www.redhat.com While every precaution has been taken in the preparation of this book, the publisher assumes no responsibility for errors or omissions, or for damages resulting from the use of the information con- tained herein. The Official Red Hat Linux Installation Guide may be reproduced and distributed in whole or in part, in any medium, physical or electronic, so long as this copyright notice remains intact and unchanged on all copies. -
Custom Panels Beautiful Basics and COM Retail Pricing Guide
Custom Panels Beautiful Basics and COM Retail Pricing Guide June 2016 Table of Contents 6 PLEATED PANELS 20 GROMMET PANELS 34 RIPPLE WAVE PANELS 48 ADDITIONAL ITEMS 49 TERMS AND CONDITIONS Carol's Roman Shades 130 Mason Circle, Suite K Concord, CA 94520 Tel 925-674-9622 Fax 800-295-2173 Toll Free 800-422-1210 carolsromanshades.com ©2016 Carol’s Roman Shades Inc. All Rights Reserved. Your Trusted Partner When you choose Carol’s Roman Shades, you choose a trusted partner. Our commitment is to enhance your reputation by providing the highest quality service and workmanship available in the design industry. That’s why, for over 35 years, design professionals have trusted us with their projects and customers. You will see our work proudly displayed throughout the country, in some of America’s finest homes. We have also earned high marks along the way, with our work in quaint Bed and Breakfasts, large resorts and many corporate and government offices. We invite you to learn more about our distinguished products and services and joining other design professionals who have discovered Carol’s Roman Shades as a trusted partner. Page 4 Phone 1-800-422-1210 carolsromanshades.com Beautiful Basics Fabric BEAUTY • QUALITY • CONVENIENCE Carol’s Roman Shades presents Beautiful Basics: an exquisite grouping of linens, cottons and blends chosen especially for our design professionals. This unique gathering of fabrics is every bit as varied as those seen in many showrooms, and includes many textiles which are woven exclusively for Carol’s Roman Shades. Our long term relationships with our mills enable us to stock all our fabrics so that each Beautiful Basics order can be manufactured as soon as we receive you request.