COVID-19 Control Strategies and Intervention Effects in Resource Limited Settings: a Modeling Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Public Open Spaces in Crisis: Appraisal and Observation from Metropolitan Kathmandu, Nepal
Vol. 13(4), pp. 77-90, October-December, 2020 DOI: 10.5897/JGRP2020.0797 Article Number: B74E25D65143 ISSN 2070-1845 Copyright © 2020 Author(s) retain the copyright of this article Journal of Geography and Regional Planning http://www.academicjournals.org/JGRP Full Length Research Paper Public open spaces in Crisis: Appraisal and observation from metropolitan Kathmandu, Nepal Krishna Prasad Timalsina Department of Geography, Trichandra Multiple Campus, Faculty of Humanities and Social Science, Tribhuvan University (TU), Nepal. Received 10 September, 2020; Accepted 13 October, 2020 There is an emerging debate in the literature of urbanism that public open space is in crisis in the cities of developing countries due to the increasing trends of urbanization and in-migration. With the significant growth of the urban population and rapid expansion of the city, the land demand for housing and other infrastructure development is very high. The high rate of urbanization due to which encroachment, high speculation, use change, etc. are the major reasons for decreasing public open spaces. There are many inferences that public open spaces are decreasing in Kathmandu Metropolitan City (KMC) as Tundikhel; an important public open space located in the heart of Kathmandu is decreasing in its size and has changed in its use over time. At present, KMC does not have a sizable public open space for emergency uses such as evacuation, relief, recovery, and reconstruction during the catastrophic hazards. Analysis of historical imagery and the changing patterns of land use reveal that the decreasing trends of open spaces may lead more vulnerable to the city as it does not have public open space for disaster management in an emergency need. -
Training on Structural and Seismic Engineering Report 2016
Training on Structural and Seismic Engineering Report 2016 C2C on Post-earthquake support on reconstruction C2C ON POST-EARTHQUAKE SUPPORT ON RECONSTRUCTION 1 Table of Contents I. Understanding Earthquakes .......................................................................... 4 II. History of Earthquakes in Nepal .................................................................... 6 III. Architectural Trends in Nepal ........................................................................ 6 IV. Technical Assessment ................................................................................... 8 V. Trainings ........................................................................................................ 8 i 1st Training, Yokohama ii. 2nd Training, Kathmandu iii. 3rd Training, Kathmandu VI. Challenges .....................................................................................................11 VII. Way Forward ..................................................................................................11 2 TRAINING ON STRUCTURAL AND SEISMIC ENGINEERING Messages Mr. Shinken Sakawa Mr. Indra Man Singh Suwal Director General Head of Department Housing and Architecture Bureau Disaster Management Department City of Yokohama Kathmandu Metropolitan City Office I would like to express our condolences On behalf of Kathmandu Metropolitan City to the people who were affected by the Office, it is my pleasure to contribute to this earthquake. Japan is another country that first issue of the Training on Structural and experiences -
2Nd WORLD ASSEMBLY of Local and Regional Governments
table of FOREWORD contents Dr. Bernadia Tjandradewi Secretary General of UCLG ASPAC 2 FOREWORD Local governments are critical to global development due to their direct responsibility for citizens’ well-being in all respects. Their roles and experience 3 TABLE OF CONTENTS provide unique perspectives on how we should respond to rapid transformation from rural to urban world that is happening worldwide. Local governments 4-5 ENHANCING THE UNITED VOICE OF CITIES AND LOCAL GOVERNMENTS IN ASIA-PACIFIC REGION IN MEETING THE are up for higher expectations and have been accelerating their work and GLOBAL CHALLENGES collaboration for opportunities and challenges ahead. 6-7 GOING BACK IN TIME: 2013-2018 MILESTONES As a platform of cities and local governments in the Asia-Pacific region, UCLG ASPAC sees our significant contribution as cooperation enabler, considering 8-9 GETTING TO KNOW THE MEMBERSHIP the strong and extensive network that we have built through decades of our work in the region. Amidst the increasingly active municipalities, UCLG ASPAC 10-11 LEADING CHANGE: UCLG ASPAC GOVERNANCE STRUCTURE take pride in the fact that we are among trusted partners that help cities and local governments develop their own solutions to development challenges. 12-13 GOVERNING BODIES To set out our way forward, UCLG ASPAC prepared a 2015-2020 Strategic Plan, 14-15 REACHING THE AUDIENCES referred to as a Manifesto, to provide guidelines and stimulate the needed 16-17 improvements to fulfil our vision and missions. This document was developed THE SECRETARIAT AND FINANCIAL HIGHLIGHTS upon UCLG ASPAC’s members’ response to an online need assessment survey 18-19 CONVENING WITH LEADERS: STATUTORY MEETINGS AND that the Secretariat conducted in January-May 2014. -

(Rehabilitation and Recovery from Nepal Earthquake) Project
Session 2: Weaving BBB Principle into Reconstruction and Recovery Overview of Japanese Assistance for Reconstruction and Recovery in Nepal Mr. Ichiro Kobayashi, Project Leader, JICA RRNE Project 1/50 Table of Contents 1. Overview of JICA Projects 2. Housing 3. School 4. Cultural Heritage 5. Other Infrastructure & Livelihood Recovery 6. Understanding Disaster Risk 7. Plan Formulation 8. Conclusion and Way Forward 2/50 1. Overview of JICA Projects 3/50 Basic Strategy of JICA BBB Concept Recovery of damaged houses, schools, infrastructure, livelihood Gorkha Resilient Earthquake Nepal Disaster Risk Analysis 2015 Present Future JICA’s unique contribution: Parallel implementation of recovery projects and disaster risk analysis for DRR actions to reduce future vulnerability. 4/50 Timeline 2015 2016 2017 2018 2019 2020 2021 Housing School Hospital, Bridge Water Supply Recovery Small-scale Infra. Livelihood KV Risk Assessment KV Resilience Plan Rehabilitation and Risk Analysis Analysis Risk & DRR Action & DRR Recovery Plan 5/50 Location Map of JICA Projects Source: Survey Department, Made by JICA Project Team 6/50 Financial Input Amount Target Modality (Mill USD) Housing Loan 96 School Loan 112 Cultural Heritage Counterpart Fund 3 Hospital, Bridge, Grant 32 Water Supply Others 31 Total 275 Source: JICA 7/50 2. Housing Reconstruction Providing financial assistance is USD 96 million in two districts Technical support for establishment of standard housing design including structural analysis ‒ Housing Catalogue ‒ Minimum Requirements Handbook, Guidebook and Video for safe houses Training for masons, engineers and house owners 8/50 Structural Calculation and Analysis Source: JICA Project Team(RRNE) Static & FEM (Finite Element Method) were conducted and results were applied to the model design in the catalogue. -
Shivapuri Nagarjun Brouchre
provide opportunities for recreation, hiking , spiritual fitness and Visitors Facilities wilderness. The park is virtually surrounded by a 130 km long stone wall, The Kathmandu based tour/trek operators conduct regular having 95 km long graveled-road and 83 km foot trails constructed tourism activities like a day-hike to Shivapuri Peak, viewig a snow for trekking. There are few hotels/lodges in buffer zone. Trained pear panorama of other Himalaya and visit Nagi gumba. The other and experienced nature guides are available in different entrance popular activities within the park are bird watcing, jungle walk, cycling, hiking and trekking. gates. Major Hiking Routes Park regulations to follow or • Nagarkot-Jhule-Chisapani things to remember • Sundarijal-Manichur-Jhule-Chisapani • Entering the park without a permit is illegal. Park personnel may • Sundarijal-Mulkharka-Chisapani ask for the permit, so visitors are requested to keep the permit with • Sundarijal-Mulkharka-Shivapuri them at all times. • Panimuhan-Nagigumba-Baghdwar-Shivapuri Peak • Entering into the park is one’s own responsibility. • Panimuhan-Bagdwar-Shivapuri Peak • The entry permit is non-refundable, non-transferable and is for single entry only. • Panimuhan-Chhapbhanjyang-Shivapuri Peak • Don’t injure, kill or uproot plants and animals. All flora and fauna • Panimuhan-Chhapbhanjyang-Sikre are fully protected and must not be disturbed. http//:www.dnpwc.gov.np • Panimuhan-Baghdwar-Rholche-Chisapani • Rubbish must be placed out, buried or disposed off in designated www.snnp.gov.np • Tokha-Jagat-Gurjebhanjyang-GurungGaun areas. • Kakani-Gurje-Chhapbhanjyang-Shivapuri Peak • Vehicles need not blow horn inside the park. Website: • Panimuhan-Gurjebhanjyang-Kakani • Carrying arms, ammunitions, poisons and use of such things are Web: completely prohibited. -

Newsletter June, 2019
J U N E , 2 0 1 9 I S S U E # 1 V O L . 1 7 WILDLIFE CONSERVATION NEPAL Newsletter This issue covers our activities from January–June 2019 and it has been an exciting first half of the I N T H I S I S S U E year. WCN moved to a new location at Dhapasi Height. We are all geared up with old and new partnerships for new ventures and ideas. Green Schools in WCN partnered with the Ministry of Education, Nepal Science and Technology (MoEST) to reach out to all the community schools of Nepal to initiate Eco-Smart Schools green activities in their respective schools. Climate Action WCN is working with three municipalities (Budhanilkantha, Gokarneswor and Shankharapur) to develop an innovative local curricula comprising Celebrations of local environment, economics and culture. Collaborations Our Climate Action unit has been active in building the capacity of community forests user groups in Nawalparasi and Chitwan. Mass tree plantations were conducted.We are excited and trying our best to achieve our vision. We look forward for your support. WCN TEAM WCN Newsletter |Jun 2019 1 Issue 1 Volume 17 GREEN SCHOOLS IN NEPAL Amidst a massive gathering at Rastriya Sabhagriha, Kathmandu on the eve of World Environment Day, June 4, 2019 Honorable Minister for Education, Science and Technology (MOEST) Mr. Giriraj Mani Pokhrel launched the Green School Resource Handbook, a joint publication of Centre of Education and Human Resource Development (CEHRD) and WCN. The Green School Resource Handbook has been published by Nepal Government, based under the Government's Green School Directive 2075 formulated to involve and have every school in Nepal to undergo green initiatives. -

Government of Nepal
Government of Nepal District Transport Master Plan (DTMP) Ministry of Federal Affairs and Local Development Department of Local Infrastructure Development and Agricultural Roads (DOLIDAR) District Development Committee, KATHMANDU VOLUME-I (MAIN REPORT) AUGUST 2013 Submitted by SITARA Consult Pvt. Ltd. for the District Development Committee (DDC) and District Technical Office (DTO), Kathmandu with Technical Assistance from the Department of Local Infrastructure and Agricultural Roads (DOLIDAR) Ministry of Federal Affairs and Local Development and grant supported by DFID. ACKNOWLEDGEMENT This DTMP Final Report for Kathmandu District has been prepared on the basis of DOLIDAR’s DTMP Guidelines for the Preparation of District Transport Master Plan 2012. We would like to express our sincere gratitude to RTI Sector Maintenance Pilot and DOLIDAR for providing us an opportunity to prepare this DTMP. We would also like to acknowledge the valuable suggestions, guidance and support provided by DDC officials, DTO Engineers and DTICC members and all the participants present in various workshops organized during the preparation this DTMP without which this report would not be in the present form. At last but not the least, we would also like to express our sincere thanks to all the concerned who directly or indirectly helped us in preparing this DTMP. SITARA Consult Pvt. Ltd Kupondole, Lalitpur, Nepal i EXECUTIVE SUMMARY Kathmandu District is located in Bagmati Zone of the Central Development Region of Nepal. It borders with Bhaktapur and Kavrepalanchowk district to the East, Dhading and Nuwakot district to the West, Nuwakot and Sindhupalchowk district to the north, Lalitpur and Makwanpur district to the South. The district has one metropolitan city, one municipality and fifty-seven VDCs, ten constituency areas. -

C E N T R a L W E S T E
Bhijer J u m l a Saldang N E P A L - W E S T E R N R E G I O N Patarasi Chhonhup f Zones, Districts and Village Development Committees, April 2015 Tinje Lo M anthang Kaingaon National boundary Zone boundary Village Development Comm ittee boundary Phoksundo Chhosar Region boundary District boundary Gothichour Charang Date Created: 28 Apr 2015 Contact: [email protected] Data sources: WFP, Survey Department of Nepal, SRTM Website: www.wfp.org 0 10 20 40 Rim i Prepared by: HQ, OSEP GIS The designations employed and the presentation of material in M I D - W E Dho S T E R N the map(s) do not imply the expression of any opinion on the Kilom eters part of WFP concerning the legal or constitutional status of any Map Reference: country, territory, city or sea, or concerning the delimitation of its ± frontiers or boundaries. Sarmi NPL_ADMIN_WesternRegion_A0L Pahada © World Food Programme 2015 Narku Chharka Liku Gham i Tripurakot Kalika K A R N A L I FAR-W ESTERN Lhan Raha MID-W ESTERN BJ a Hj a Er kRo It Surkhang Bhagawatitol Juphal D o l p a M u s t a n g W ESTERN Lawan Suhu Chhusang CENTRAL Gotam kot EASTERN Dunai Majhphal Mukot Kagbeni Sahartara Jhong Phu Nar Syalakhadhi Sisne Marpha Muktinath Jom som Tangkim anang Tukuche Ranm am aikot M a n a n g Baphikot Jang Pipal Pwang R u k u m Kowang Khangsar Ghyaru Mudi Pokhara M y a g d i Bhraka Sam agaun Gurja Ransi Hukam Syalpakha Kunjo Thoche W LeteE S T Manang E R N Chokhawang Kanda Narachyang Sankh Shova Chhekam par Kol Bagarchhap Pisang Kuinem angale Marwang Taksera Prok Dana Bihi Lulang Chim khola -

Assessment of Changes in Land Use/Land Cover and Land Surface Temperatures and Their Impact on Surface Urban Heat Island Phenomena in the Kathmandu Valley (1988–2018)
International Journal of Geo-Information Article Assessment of Changes in Land Use/Land Cover and Land Surface Temperatures and Their Impact on Surface Urban Heat Island Phenomena in the Kathmandu Valley (1988–2018) Md. Omar Sarif 1 , Bhagawat Rimal 2,3,* and Nigel E. Stork 4 1 Geographic Information System (GIS) Cell, Motilal Nehru National Institute of Technology Allahabad, Prayagraj 211004, India; [email protected] or [email protected] 2 College of Applied Sciences (CAS)-Nepal, Tribhuvan University, Kathmandu 44613, Nepal; [email protected] 3 The State Key Laboratory of Remote Sensing Science, Institute of Remote Sensing and Digital Earth, Chinese Academy of Sciences, Beijing 100101, China 4 Environmental Future Research Institute, Griffith School of Environment, Nathan Campus, Griffith University, 170, Kessels Road, Nathan, QLD 4111, Australia; nigel.stork@griffith.edu.au * Correspondence: [email protected] Received: 28 October 2020; Accepted: 23 November 2020; Published: 6 December 2020 Abstract: More than half of the world’s populations now live in rapidly expanding urban and its surrounding areas. The consequences for Land Use/Land Cover (LULC) dynamics and Surface Urban Heat Island (SUHI) phenomena are poorly understood for many new cities. We explore this issue and their inter-relationship in the Kathmandu Valley, an area of roughly 694 km2, at decadal intervals using April (summer) Landsat images of 1988, 1998, 2008, and 2018. LULC assessment was made using the Support Vector Machine algorithm. In the Kathmandu Valley, most land is either natural vegetation or agricultural land but in the study period there was a rapid expansion of impervious surfaces in urban areas. -
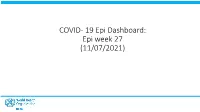
COVID- 19 Epi Dashboard: Epi Week 27 (11/07/2021) National COVID- 19 Cases and Deaths
COVID- 19 Epi Dashboard: Epi week 27 (11/07/2021) National COVID- 19 cases and deaths 655,449 22,285 10,827 9,382 319 1.43 Confirmed cases Cases per million Last 7 days Total Deaths Deaths per million CFR Daily Covid-19 cases Daily COVID- 19 deaths 10000 700 8000 600 500 6000 400 4000 300 200 2000 100 Number of cases 0 0 deaths of Number Date of reporting Date of reporting Cumulative Covid-19 cases Cumulative COVID- 19 deaths 700000 10000 600000 9000 8000 500000 7000 400000 6000 5000 300000 4000 200000 deaths of Number 3000 Number of cases 2000 100000 1000 0 0 Date of reporting Date of reporting 2 Province 1 COVID- 19 cases and deaths 76,696 15,725 2,535 1,253 257 1.63 Last 7 days Confirmed cases Cases per million Total Deaths Deaths per million CFR Daily Covid-19 cases Daily COVID- 19 deaths 1400 200 1200 1000 150 800 100 600 400 50 200 Number of cases 0 deaths of Number 0 Date of reporting Date of reporting Cumulative Covid-19 cases Cumulative COVID- 19 deaths 100000 1400 1200 80000 1000 60000 800 40000 600 20000 400 Number of deaths of Number Number of of cases Number 200 0 0 Date of reporting Date of reporting 3 Province 2 COVID- 19 cases and deaths 7,188 237 43,938 733 120 1.67 Confirmed cases Cases per million Last 7 days Total Deaths Deaths per million CFR Daily Covid-19 cases Daily COVID- 19 deaths 800 35 700 30 600 25 500 20 400 15 300 200 10 Number of cases 5 100 deaths of Number 0 0 Date of reporting Date of reporting Cumulative Covid-19 cases Cumulative COVID- 19 deaths 50000 800 45000 700 40000 600 35000 30000 500 -

A Reading Guide to Nepalese History John Whelpton
Himalaya, the Journal of the Association for Nepal and Himalayan Studies Volume 25 Article 5 Number 1 Himalaya No. 1 & 2 2005 A Reading Guide to Nepalese History John Whelpton Follow this and additional works at: http://digitalcommons.macalester.edu/himalaya Recommended Citation Whelpton, John (2005) "A Reading Guide to Nepalese History," Himalaya, the Journal of the Association for Nepal and Himalayan Studies: Vol. 25: No. 1, Article 5. Available at: http://digitalcommons.macalester.edu/himalaya/vol25/iss1/5 This Research Article is brought to you for free and open access by the DigitalCommons@Macalester College at DigitalCommons@Macalester College. It has been accepted for inclusion in Himalaya, the Journal of the Association for Nepal and Himalayan Studies by an authorized administrator of DigitalCommons@Macalester College. For more information, please contact [email protected]. jOHN WHELPTON A READING GUIDE TO NEPAL ESE HISTORY ·t.t. ' There is no single book or series that can be regarded as · an authoritative Chandra Shamsher and Family history of Nepal in the way that, This brief survey is intended as a list of works which Scientifique in France. This can be consulted online at for example, I have found especially useful myself or which I http://www.vjf.cnrs.fr/wwwisis/BIBLI0.02/form.htm the Cambridge think would be particularly suitable for readers wanting to follow up topics necessarily treated very · Ancient History BASIC NARRATIVES cursorily in my recent one-volume History of Nepal ' or the Oxford (Cambridge: Cambridge University Press, 2005). It There is no single book or series that can be regarded History of England includes some of the pre-1990 works listed in my as an authoritative history of Nepal in the way that, is accepted in the earlier Nepal (World Bibliographical Series, Oxford for example, the Cambridge Ancient History or the & Santa Barbara: Clio Press, 1990) and, though it Oxford History of England is accepted in the United United Kingdom. -

Chapter 10 Implementation Plan
The Project on Urban Transport Improvement for Kathmandu Valley in Federal Democratic Republic of Nepal Final Report May 2017 CHAPTER 10 IMPLEMENTATION PLAN 10.1 Transport Implementation Plan 10.1.1 Staging Plan (1) Basic Concept of Staging Plan Staging plan is divided into three phases, namely short term (-2020), middle term (2021-2025) and long term (2026-2030). The targets to be achieved in each phase are: Long term (2026 - 2030) - Establishment of sustainable transport with high mobility, safety and comfort. Middle Term (2021 – 2025) - Implementation of Priority Project - Establishment of all the systems necessary for achieving long term target Short Term (-2020) - Strengthening of institutional framework for planned development - Solving urgent issues - Commencement of disaster prevention measures Based on the targets, the concept in each phase for land use development, road development and public transport development is shown in Figure 10.1.1. Short Term Middle Term Long Term (-2020) (2021-2025) (2026-2030) Strengthening of institutional Implementation of priority Establishment of sustainable T framework for planned projects. transport with high mobility, a r development Establishment of all the safety and comfort get Solving urgent issues systems necessary for Commencement of disaster achieving the long term prevention measures target Selection of pilot urban Development of priority Development of all the new development area and urban area with land use urban area. Land Use Implementation. control and building Equipping necessary roads Enforcement and diffusion control. and open spaces in of land pooling system. Implementation of land urbanized area. Establishment of strict pooling system by PPP building and development scheme.