) Mortality and Morbidity Weekly Bulletin (MMWB
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bangladesh Needs Assessment Working Group (NAWG) Report on Landslides
Bangladesh Needs Assessment Working Group (NAWG) Report on Landslides Landslides, Bangladesh, June 2017 Report date: 19 June 2017 (Source: UNICEF) Md. Yousuf Ali, Director-MIM, DDM, Email: [email protected] Contact for Inquiries: Arshad Muhammad, Assistant Country Director – Programs , CARE, Email: [email protected] Landslides, Bangladesh June 2017 Contents Contents 2 Background 3 Key Findings 4 Context of the Affected Area 6 Key characteristics of the affected districts by the landslides 8 Situation Overview 10 Detailed Findings 15 Access and Infrastructure 15 Communication 16 Child Protection 18 Education 19 Food Security 20 Livelihoods and Income 20 Gender Based Violence 21 Gender 23 Health 23 Market 25 Nutrition 26 Shelter 27 Water, Sanitation and Hygiene (WASH) 28 Annex A: Affected people per Upazila 30 2 Landslides, Bangladesh June 2017 Background On June 13th the districts of Bandarban, Chittagong, Rangamati, Khagrachari and Cox’s Bazaar suffered from possibly the deadliest landslides in their history. The disaster killed an estimated 160 persons, including 115 persons in Rangamati alone. According to the Chittagong Divisional Health Office Control Room Report, a total of 187 injured persons were admitted in local level hospitals. Approximately 85% of patients were admitted in Rangamati. While landslide related disaster occurs nearly every year, the second highest death toll of 127 deceased persons was recorded in 2007 [Disaster Forum, June 2017]. Monsoon rains caused severe flooding in low-lying areas to significantly damage road and communication infrastructure. Flood water rendered remote communities in Bandarban, Chittagong, and Rangamati districts were inaccessible by road. On June 14th, mudslides in southeast Bangladesh claimed additional lives in Cox's Bazaar and Khagrachari districts to further damage homes and infrastructure. -
Impacts of the Rohingya Refugee Influx on Host Communities
Impacts of the Rohingya Refugee November 2018 Impacts of the Rohingya Refugee Influx on Host Communities November 2018 United Nations Development Programme www.bd.undp.org United Nations Development Programme UN Offices, 18th Floor, IDB Bhaban Agargaon, Sher-e-Bangla Nagar Dhaka 1207, Bangladesh www.bd.undp.org Standard Disclaimer: This report is a product of the UNDP Bangladesh Country Office. The findings, interpretations, and conclusions expressed in this report do not necessarily reflect the views of the Executive Board of the UNDP or the governments they represent. UNDP does not guarantee the accuracy of the data included in this work. The boundaries, colors, denominations, and other information shown on any map in this work do not imply any judgment on the part of UNDP concerning the legal status of any territory or the endorsement or acceptance of such boundaries. Copyright Statement: Copyright © United Nations Development Programme, Bangladesh Country Office UN Offices, 18th Floor, IDB Bhaban, Agargaon, Sher-e-Bangla Nagar, Dhaka 1207, Bangladesh Table of Contents Figures, tables and boxes IV CHAPTER 4 36 Acknowledgement VIII The Rohingya influx, GoB response and institutional set-up Acronyms IX 4.1. The refugee population profile 37 Executive summary 1 4.1.1. Definition 37 4.1.2. Previous inflows, repatriation and CHAPTER 1 16 37 remaining refugees Introduction 4.1.3. The latest influx 37 4.1.4. Demographic and other characteristics 37 CHAPTER 2 18 of refugees 4.2. Bangladesh government policy on the Rationale and methodology 39 Rohingya and response 2.1. Rationale 18 4.3. Organizational framework for the refugee 42 2.2. -

Ministry of Food and Disaster Management
Disaster Management Information Centre Disaster Management Bureau (DMB) Ministry of Food and Disaster Management Disaster Management and Relief Bhaban (6th Floor) 92-93 Mohakhali C/A, Dhaka-1212, Bangladesh Phone: +88-02-9890937, Fax: +88-02-9890854 Email:[email protected],H [email protected] Web:http://www.cdmp.org.bd,H www.dmb.gov.bd Emergency Situation Report on Weather, Flash Flood and Hill Slide Title: Emergency Bangladesh Location: 20°22'N-26°36'N, 87°48'E-92°41'E, Covering From : SUN-01-JUL-2012:1400 Period: To : MON-02-JUL-2012:1400 Transmission Date/Time: MON-02-JUL-2012:1630 Prepared DMIC, DMB by: Situation Report on Weather, Flash Flood and Hill Slide Warning Message A monsoon low has developed over North West Bay and adjoining area. Under its influence steep pressure gradient lies over North Bay and adjoining area. Squally weather may affect North Bay, adjoining coastal area and the maritime ports. Maritime ports of Chittagong, Cox’s Bazar and Mongla have been advised to hoist local cautionary signal no. THREE (R) THREE. All fishing boats and trawlers over North Bay have been advised to come close to the coast and proceed with caution till further notice. [Source: BMD – www.bmd.gov.bd; Data Date: Jul 02, 2012] The Disaster Management Information Centre is the information hub of the Ministry of Food and Disaster Management for risk reduction, hazard early warnings and emergency response and recovery activities Page 1 of 11 Weather Forecast Synoptic Situation: Monsoon is fairly active over Southern part and less active over Northern part of Bangladesh and moderate over North Bay. -
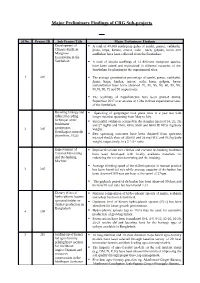
Major Preliminary Findings of CRG Sub-Projects
Major Preliminary Findings of CRG Sub-projects Sl No. Project ID Sub-Project Title Major Preliminary Findings Development of A total of 48,000 seeds/prop gules of sundri, passur, vathkathi, Climate Resilient jhana, kirpa, kankra, amoor, soila , baen, golpata, keora and Mangrove amdhekur have been collected from the Sundarban. Ecosystems in the Sundarban A total of 36,000 seedlings of 12 different mangrove species have been raised and maintained in different nurseries of the Sundarban for planting in the experimental sites. 1 301 The average germination percentage of sundri, passur, vathkathi, jhana, kirpa, kankra, amoor, soila, baen, golpata, keora andamdhekur have been observed 70, 80, 95, 90, 60, 90, 90, 80,70, 90, 75 and 90 respectively. The seedlings of Nypafruticans have been planted during September 2017 over an area of 1.2ha in three experimental sites of the Sundarban. Breeding biology and Spawning of gangmagur took place once in a year but with induced breeding longer duration spawning from May to July. technique of the Successful ovulation occurred in the females injected 24, 25, 26, freshwater and 27 mgPG and 3500, 4500, 5500 and 6500 IU HCG /kg body 2 305 gangmagur, weight. Hemibagrus menoda Best spawning outcomes have been obtained from spawners (Hamilton, 1822) injected double dose of 3500IU and 26 mg HCG and PG/kg body weight, respectively, in a 2♂:1♀ ratio. Improvement of Improved coconut tree climber and coconut de-husking machines Coconut Harvesting have been developed with locally available materials for and De-husking enhancing the coconut harvesting and de- husking. Machine Average climbing speed of the skilled operator in manual practice 3 307 has been found 0.4 m/s while average capacity of de-husker has been observed 309 nuts per hour at the speed of 27rpm. -

Department of Sociology University of Dhaka Dhaka University Institutional Repository
THE NATURE AND EXTENT OF HOMICIDE IN BANGLADESH: A CONTENT ANALYSIS ON REPORTS OF MURDER IN DAILY NEWSPAPERS T. M. Abdullah-Al-Fuad June 2016 Department of Sociology University of Dhaka Dhaka University Institutional Repository THE NATURE AND EXTENT OF HOMICIDE IN BANGLADESH: A CONTENT ANALYSIS ON REPORTS OF MURDER IN DAILY NEWSPAPERS T. M. Abdullah-Al-Fuad Reg no. 111 Session: 2011-2012 Submitted in partial fulfillment of the requirements of the degree of Master of Philosophy June 2016 Department of Sociology University of Dhaka Dhaka University Institutional Repository DEDICATION To my parents and sister Dhaka University Institutional Repository Abstract As homicide is one of the most comparable and accurate indicators for measuring violence, the aim of this study is to improve understanding of criminal violence by providing a wealth of information about where homicide occurs and what is the current nature and trend, what are the socio-demographic characteristics of homicide offender and its victim, about who is most at risk, why they are at risk, what are the relationship between victim and offender and exactly how their lives are taken from them. Additionally, homicide patterns over time shed light on regional differences, especially when looking at long-term trends. The connection between violence, security and development, within the broader context of the rule of law, is an important factor to be considered. Since its impact goes beyond the loss of human life and can create a climate of fear and uncertainty, intentional homicide (and violent crime) is a threat to the population. Homicide data can therefore play an important role in monitoring security and justice. -

Lesson Learning Report: Economic Empowerment of Jumiya People
February 2015 Lesson Learning Report: Economic Empowerment of Jumiya people through Medicinal Plant Cultivation Table of Contents Maps ............................................................................................................................................................. 4 List of Acronyms ............................................................................................................................................ 5 Executive Summary ....................................................................................................................................... 6 Findings ..................................................................................................................................................... 6 Lessons Learned ........................................................................................................................................ 8 Recommendations for National Government .......................................................................................... 8 Section 1 Background, Purpose and Methodology ....................................................................................... 9 1.1. Background ........................................................................................................................................ 9 1.2. Purpose .............................................................................................................................................. 9 1.3. Methodology ..................................................................................................................................... -

Weekly Situation Report 8
Weekly Situation Report # 8 Date of issue: 30 December 2017 Period covered: 23 December – 30 December Location: Bangladesh Emergency type: Rohingya Refugee Crisis 867 550 149 962 children aged under 7 655 500 165 927 children 1.2 million total Rohingya years vaccinated with pentavalent, new arrivals since under 15 years were people targeted for in Bangladesh pneumococcal, and bivalent oral vaccinated with Td 25 Aug 2017 humanitarian assistance polio vaccines. vaccine. KEY HIGHLIGHTS A total of 2934 cases suspected of diphtheria, of whom 27 died, have been reported from 8 November – 30 December 2017. The District Core Committee for Diphtheria Outbreak, chaired by the Civil Surgeon of Cox’s Bazar, has been formalized with WHO and partners to contain the spread of diphtheria through effective treatment, vaccination, and contact tracing activities. Around 50% of Rohingya children are malnourished and anemic. The acute malnutrition rate in children under 5 years is 25%. WHO, as co-lead of the health sector, is working to strengthen linkages with WASH, nutrition, and child protection to address issues of acute malnutrition and anemia. Approximately 67% of pregnant women have no or very limited access to gynecological and obstetrical pregnancy related complications. Arrangements to obtain 24/7 facility access for maternal health and critical care services are underway in coordination with the Refugee Relief and Repatriation Commissioner (RRRC), Directorate General of Health Services (DGHS), and WHO led Strategic Advisory Group (SAG). SITUATION OVERVIEW Since 25 August 2017, an estimated 655 500 Rohingya have crossed the border into Cox’s Bazar, joining approximately 300 000 others who had fled in earlier waves of displacement. -

Emergency Assistance Project – Improvement of (1) Rotna Palong up Office-Coat Bazar- Valukhiya Bazar Rd (Valukia Sea Beach Rd)
Initial Environmental Examination Project No. 52174-001 March 2020 G0582-BAN: Emergency Assistance Project BANGLADESH: Emergency Assistance Project – Improvement of (1) Rotna Palong UP office-Coat Bazar- Valukhiya Bazar Rd (Valukia Sea beach rd). By BC at Ch. 00-4300m (ID: - 422943001) & (2) Rotna Palong UP office-Chakbaita Bazar via Goyalmara rd (Yousuf Ali Ratna Palong kariabonia Road) by BC at Ch. 00-4435m (ID: - 422943004) Under Ukhiya Upazila, Dist.: Cox’s Bazar Package: EAP/LGED/W4D This Initial Environmental Examination is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. Emergency Assistance Project ADB Project 52174-001 | Grant 0582-BAN | TA 9546 BAN Initial Environmental Examination Package BANGLADESH: Emergency Assistance Project – Improvement of (1) Rotna Palong UP office- Coat Bazar-Valukhiya Bazar Rd (Valukia Sea beach rd). By BC at Ch. 00-4300m (ID: - 422943001) & (2) Rotna Palong UP office-Chakbaita Bazar via Goyalmara rd (Yousuf Ali Ratna Palong kariabonia Road) by BC at Ch. 00-4435m (ID: - 422943004) Under Ukhiya Upazila, Dist.: Cox’s Bazar Implementing Agency Local Government Engineering Department (LGED) Ministry of Local Government, Rural Development and Cooperatives (MLGRDC) EAP/LGED/W4D March 2020 BAN: EMERGENCY ASSISTANCE PROJECT Output 04: Access road Improved March 2020 The environmental impact assessment report is a document of the borrower. -

Report on AK Taj Group Masrur M. A. Hoque.Pdf (983.4Kb)
Internship Report on AK TAJ GROUP Prepared for, MD. Tamzidul Islam Assistant Professor BRAC BusinessSchool BRAC University Prepared By, Masrur M. A. Hoque ID # 12164092 Submission Date – 15/12/2015 LETTER OF TRANSMITTAL December 15, 2015 MD. Tamzidul Islam Assistant Professor BRAC BusinessSchool BRAC University Subject: Internship Report. Dear Sir, I would like to thank you for supervising and helping me throughout the semester. With due respect I am submitting a copy of intern report foryourappreciation. I have given my best effort to prepare the report with relevant information that I have collected from an onsite production department which is belongs to a group of company and from other sources during my accomplishthe course. I have the immense pleasure to have the opportunity to study on the marketing practices of AK TAJ Group. There is no doubt that the knowledge I have gathered during the study will help me in real life. For your kind consideration I would like to mention that there might be some errors and mistakes due to limitations of my knowledge. I expect that you will forgive me considering that I am still learner and in the process of learning. Thanking for your time and reviews. Yours faithfully Masrur M. A. Hoque ID-12164092 BRAC Business School BRAC University Acknowledgement The successful completion of this internship might not be possible in time without the help some person whose suggestion and inspiration made it happen. First of all I want to thank my Course Instructor MD. Tamzidul Islam for guiding me during the course. Without his help this report would not have been accomplished. -

List of Upazilas of Bangladesh
List Of Upazilas of Bangladesh : Division District Upazila Rajshahi Division Joypurhat District Akkelpur Upazila Rajshahi Division Joypurhat District Joypurhat Sadar Upazila Rajshahi Division Joypurhat District Kalai Upazila Rajshahi Division Joypurhat District Khetlal Upazila Rajshahi Division Joypurhat District Panchbibi Upazila Rajshahi Division Bogra District Adamdighi Upazila Rajshahi Division Bogra District Bogra Sadar Upazila Rajshahi Division Bogra District Dhunat Upazila Rajshahi Division Bogra District Dhupchanchia Upazila Rajshahi Division Bogra District Gabtali Upazila Rajshahi Division Bogra District Kahaloo Upazila Rajshahi Division Bogra District Nandigram Upazila Rajshahi Division Bogra District Sariakandi Upazila Rajshahi Division Bogra District Shajahanpur Upazila Rajshahi Division Bogra District Sherpur Upazila Rajshahi Division Bogra District Shibganj Upazila Rajshahi Division Bogra District Sonatola Upazila Rajshahi Division Naogaon District Atrai Upazila Rajshahi Division Naogaon District Badalgachhi Upazila Rajshahi Division Naogaon District Manda Upazila Rajshahi Division Naogaon District Dhamoirhat Upazila Rajshahi Division Naogaon District Mohadevpur Upazila Rajshahi Division Naogaon District Naogaon Sadar Upazila Rajshahi Division Naogaon District Niamatpur Upazila Rajshahi Division Naogaon District Patnitala Upazila Rajshahi Division Naogaon District Porsha Upazila Rajshahi Division Naogaon District Raninagar Upazila Rajshahi Division Naogaon District Sapahar Upazila Rajshahi Division Natore District Bagatipara -

Annex to Chapter 3. Results Framework for the 4Th HPBSP 2016
Annex to Chapter 3. Results Framework for the 4th HPBSP 2016-2021 Means of Result Indicator verification & Baseline & source Target 2021 timing Goal GI 1. Under-5 Mortality Rate (U5MR) BDHS, every 3 years 46, BDHS 2014 37 All citizens of GI 2. Neonatal Mortality Rate (NNMR) BDHS, every 3 years 28, BDHS 2014 21 Bangladesh enjoy health and well-being GI 3. Maternal Mortality Ratio (MMR) BMMS; MPDR 176, WHO 2015(http:// 105 www.who.int/ reproductivehealth/ publications/monitoring/ maternal-mortality-2015/ en/ GI 4. Total Fertility Rate (TFR) BDHS, every 3 years 2.3, BDHS 2014 1.7 GI 5. Prevalence of stunting among under- BDHS, every 3 years; 36.1%, BDHS 2014 25% 5children UESD, every non-DHS years GI 6. Prevalence of diabetes and hypertension BDHS, every 3 years; Dia: 11.2%; Hyp: 31.9%, Dia: 10%; Hyp: among adult women (Estimated as elevated blood NCD-RF, every 2 years BDHS 2011 30% sugar and blood pressure among women and men aged 35 years or older) GI 7. Percentage of public facilities with key BHFS, every 2 years FP: 38.2; ANC 7.8%; CH FP: 70%; ANC service readiness as per approved Essential 6.7%, BHFS 2014 50%; CH 50% Service Package (Defined as facilities (excluding CCs) having: a. for FP: guidelines, trained staff, BP machine, OCP, and condom; b. for ANC: Health Bulletin 2019 Health guidelines, trained staff, BP machine, hemoglobin, and urine protein testing capacity, Fe/folic acid tablets; c. for CH: IMCI guideline and trained staff, child scale, thermometer, growth chart, ORS, zinc, Amoxicillin, Paracetamol, Anthelmintic) Program -

Impact of Rohingya Settlement on the Landcovers at Ukhiya Upazila in Cox' S Bazar, Bangladesh
Jagannath University Journal of Life and Earth Sciences, 5(1):13-28, 2019 ISSN 2414-1402 IMPACT OF ROHINGYA SETTLEMENT ON THE LANDCOVERS AT UKHIYA UPAZILA IN COX' S BAZAR, BANGLADESH Mohammad Abdul Quader* Abstract The Ukhiya Upazila is an environmentally critical area where more than seven hundred thousand Rohingya refugees have temporarily settled since August 2017. The site is facing numerous land cover changes due to anthropogenic pressures exerted by the Rohingya resettlement program. The research measures the delineation of land cover in study area due to the 2017 forced migration of Rohingya refugees from Myanmar. In this research, the GIS-post processing classification approach is performed on Landsat images for five time periods (1980, 1990, 1999, 2010, and 2020) to identify the land cover change in the study area. From 1980 to 2020, more than 14.34 sq. km. of agricultural land increases, and 42.93 sq. km. of greenery was reduced due to anthropogenic activities. Furthermore, four classification approaches (GIS post-processing, OBIA, supervised, and unsupervised) was used to identify precise land cover classification method where GIS post-processing method seemed to be a suitable approach for land cover classification. The Kappa aspect shows that the post-processing GIS method can minimize most errors in the classifying procedure. The research will help the policymakers to identify the changes made on the land covers. The identified changes will be the key to determine the financial and ecological losses to claim compensation in the future. Keywords: Rohingya migration, Land cover, GIS-post processing, OBIA Introduction The function of anthropological action on the earth's surface is defined by land use, and visible land use characteristics on the world's body are determined by the land cover (Weihand White, 2008; Zhang et al.