Bloom's Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Variant Requirements for DNA Repair Proteins in Cancer Cell Lines That Use
Variant requirements for DNA repair proteins in cancer cell lines that use alternative lengthening of telomere mechanisms of elongation DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Alaina Rae Martinez Biomedical Sciences Graduate Program The Ohio State University 2016 Dissertation Committee: Dr. Jeffrey D. Parvin, Advisor Dr. Joanna Groden Dr. Amanda E. Toland Dr. Kay F. Huebner Copyright by Alaina Rae Martinez 2016 Abstract The human genome relies on DNA repair proteins and the telomere to maintain genome stability. Genome instability is recognized as a hallmark of cancer, as is limitless replicative capacity. Cancer cells require telomere maintenance to enable this uncontrolled growth. Most often telomerase is activated, although a subset of human cancers depend on recombination-based mechanisms known as Alternative Lengthening of Telomeres (ALT). ALT depends invariably on recombination and its associated DNA repair proteins to extend telomeres. This study tested the hypothesis that the requirement for those requisite recombination proteins include other types of DNA repair proteins. These functions were tested in ALT cell lines using C-circle abundance as a marker of ALT. The requirement for homologous recombination proteins and other DNA repair proteins varied between ALT cell lines compared. Several proteins essential for homologous recombination were dispensable for C-circle production in some ALT cell lines, while proteins grouped into excision DNA repair processes were required for C- circle production. The MSH2 mismatch repair protein was required for telomere recombination by intertelomeric exchange. In sum, our study suggests that ALT proceeds by multiple mechanisms that differ between human cancer cell lines and that some of these depend on DNA repair proteins not associated with homologous recombination pathways. -

Structure and Function of the Human Recq DNA Helicases
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2005 Structure and function of the human RecQ DNA helicases Garcia, P L Posted at the Zurich Open Repository and Archive, University of Zurich ZORA URL: https://doi.org/10.5167/uzh-34420 Dissertation Published Version Originally published at: Garcia, P L. Structure and function of the human RecQ DNA helicases. 2005, University of Zurich, Faculty of Science. Structure and Function of the Human RecQ DNA Helicases Dissertation zur Erlangung der naturwissenschaftlichen Doktorw¨urde (Dr. sc. nat.) vorgelegt der Mathematisch-naturwissenschaftlichen Fakultat¨ der Universitat¨ Z ¨urich von Patrick L. Garcia aus Unterseen BE Promotionskomitee Prof. Dr. Josef Jiricny (Vorsitz) Prof. Dr. Ulrich H ¨ubscher Dr. Pavel Janscak (Leitung der Dissertation) Z ¨urich, 2005 For my parents ii Summary The RecQ DNA helicases are highly conserved from bacteria to man and are required for the maintenance of genomic stability. All unicellular organisms contain a single RecQ helicase, whereas the number of RecQ homologues in higher organisms can vary. Mu- tations in the genes encoding three of the five human members of the RecQ family give rise to autosomal recessive disorders called Bloom syndrome, Werner syndrome and Rothmund-Thomson syndrome. These diseases manifest commonly with genomic in- stability and a high predisposition to cancer. However, the genetic alterations vary as well as the types of tumours in these syndromes. Furthermore, distinct clinical features are observed, like short stature and immunodeficiency in Bloom syndrome patients or premature ageing in Werner Syndrome patients. Also, the biochemical features of the human RecQ-like DNA helicases are diverse, pointing to different roles in the mainte- nance of genomic stability. -

The Bloom Syndrome Protein Limits the Lethality Associated with RAD51 Deficiency
Published OnlineFirst March 9, 2010; DOI: 10.1158/1541-7786.MCR-09-0534 Molecular DNA Damage and Cellular Stress Responses Cancer Research The Bloom Syndrome Protein Limits the Lethality Associated with RAD51 Deficiency Kenza Lahkim Bennani-Belhaj1,2, Sébastien Rouzeau1,2, Géraldine Buhagiar-Labarchède1,2, Pauline Chabosseau1,2, Rosine Onclercq-Delic1,2, Emilie Bayart1, Fabrice Cordelières3,4, Jérôme Couturier5,6, and Mounira Amor-Guéret1,2 Abstract Little is known about the functional interaction between the Bloom's syndrome protein (BLM) and the re- combinase RAD51 within cells. Using RNA interference technology, we provide the first demonstration that RAD51 acts upstream from BLM to prevent anaphase bridge formation. RAD51 downregulation was associated with an increase in the frequency of BLM-positive anaphase bridges, but not of BLM-associated ultrafine bridges. Time-lapse live microscopy analysis of anaphase bridge cells revealed that BLM promoted cell survival in the absence of Rad51. Our results directly implicate BLM in limiting the lethality associated with RAD51 deficiency through the processing of anaphase bridges resulting from the RAD51 defect. These findings provide insight into the molecular basis of some cancers possibly associated with variants of the RAD51 gene family. Mol Cancer Res; 8(3); 385–94. ©2010 AACR. Introduction cently, SUMOylation of BLM has been shown to regulate its association with RAD51 and its function in HR-medi- Bloom's syndrome displays one of the strongest known ated repair of damaged replication forks (13). In several correlations between chromosomal instability and a high models, it has been proposed that BLM restarts replication risk of cancer at an early age. -

Scaffolding Protein SPIDR/KIAA0146 Connects the Bloom Syndrome Helicase with Homologous Recombination Repair
Scaffolding protein SPIDR/KIAA0146 connects the Bloom syndrome helicase with homologous recombination repair Li Wan1, Jinhua Han1, Ting Liu1, Shunli Dong, Feng Xie, Hongxia Chen, and Jun Huang2 Life Sciences Institute, Zhejiang University, Hangzhou, Zhejiang 310058, China Edited by James E. Cleaver, University of California, San Francisco, CA, and approved February 26, 2013 (received for review December 1, 2012) The Bloom syndrome gene product, BLM, is a member of the highly of the SDSA pathway (6, 7). The ability of BLM to yield non- conserved RecQ family. An emerging concept is the BLM helicase crossover products is thought to play a critical role in the avoidance collaborates with the homologous recombination (HR) machinery to of chromosomal rearrangements during the homolog-directed re- help avoid undesirable HR events and to achieve a high degree of pair of chromosomal lesions. As a result, cells defective for BLM fidelity during the HR reaction. However, exactly how such coordina- exhibit elevated rates of sister chromatid exchange (SCE) (19–21). tion occurs in vivo is poorly understood. Here, we identified a protein Upon the occurrence of DNA damage, BLM is able to form termed SPIDR (scaffolding protein involved in DNA repair) as the link discrete foci, where it colocalizes with other DNA repair proteins between BLM and the HR machinery. SPIDR independently interacts (22, 23). However, mechanistically how BLM is recruited to sites with BLM and RAD51 and promotes the formation of a BLM/RAD51- of DNA damage and how it collaborates with other proteins to containing complex of biological importance. Consistent with its role mediate recombination repair remain largely unexplored. -

Haplotype Patterns in Cancer-Related Genes with Long-Range Linkage Disequilibrium: No Evidence of Association with Breast Cancer Or Positive Selection
European Journal of Human Genetics (2008) 16, 252–260 & 2008 Nature Publishing Group All rights reserved 1018-4813/08 $30.00 www.nature.com/ejhg ARTICLE Haplotype patterns in cancer-related genes with long-range linkage disequilibrium: no evidence of association with breast cancer or positive selection Gloria Ribas*,1, Roger L Milne2, Anna Gonzalez-Neira2 and Javier Benı´tez1,2 1Human Genetics Group, Human Cancer Genetics Programme, Spanish National Cancer Centre (CNIO), Madrid, Spain; 2National Genotyping Centre (CeGen), Human Cancer Genetics Programme, Spanish National Cancer Centre (CNIO), Madrid, Spain The average length of linkage disequilibrium (LD) blocks in European populations is about 22 kb. In this study, we have selected 20 genes with LD blocks larger than 60 kb (with a median length of 88 kb) from a total of 121 cancer-related genes. We observed limited haplotype diversity, with an average of three haplotypes per gene accounting for more than 90% of the diversity, two of these being a Yin–Yang pair in 95% of the LD blocks. The mean frequency of the most common haplotype in the Spanish population was just below 50%, similar to those for the HapMap CEU and African samples, but lower than the 60% observed in Asian samples. Genes involved in the regulation of nucleobases and nucleic acid metabolism were overrepresented among these 20 genes with long LD blocks (eight genes ATM, BRCA1, BRCA2, ERCC6, MLH1, MSH3, RAD54B and XRCC4) relative to the other 101 cancer-related genes studied (P ¼ 1.23 Â 10À6). The ancestral haplotype was observed at a frequency greater than 3 in 67% of the genes either in the Spanish or one of the HapMap sampled populations. -

Acetylation of BLM Protein Regulates Its Function in Response to DNA Damage Cite This: RSC Adv.,2017,7,55301 Yankun Wang and Jianyuan Luo *
RSC Advances View Article Online PAPER View Journal | View Issue Acetylation of BLM protein regulates its function in response to DNA damage Cite this: RSC Adv.,2017,7,55301 Yankun Wang and Jianyuan Luo * Bloom syndrome is an autosomal recessive disease with phenotypes of cancer predisposition and premature aging caused by mutations of the blm gene. BLM belongs to the RecQ DNA helicase family and functions in maintaining genomic stability. In this study, we found that several lysine residues of BLM were acetylated in cells. The dynamic acetylation levels of BLM were regulated by CBP/p300 and SIRT1. Received 15th June 2017 We further identified that five lysines, K476, K863, K1010, K1329, and K1411, are the major acetylation Accepted 29th November 2017 sites. Treating cells with different DNA damage agents found that acetylation of BLM was different in DOI: 10.1039/c7ra06666j response to etoposide and hydroxyurea, suggesting that BLM acetylation may have multiple functions in rsc.li/rsc-advances DNA repair. Creative Commons Attribution-NonCommercial 3.0 Unported Licence. Introduction recombination and makes DNA back to integrated condition.14 On the other hand, BLM interacts with 53BP1 and completes Bloom syndrome protein (BLM), coded by the blm gene, is the repair in the NHEJ pathway.11 It has been found that BLM is a 1417 amino acid protein. Mutations or deletions of the blm sensitive to multiple stress factors, including hydroxyurea (HU), gene lead to Bloom Syndrome (BS).1 It is an inherited etoposide and ionizing radiation (IR) which all -

Hyper Telomere Recombination Accelerates Replicative Senescence and May Promote Premature Aging
Hyper telomere recombination accelerates replicative senescence and may promote premature aging R. Tanner Hagelstroma,b, Krastan B. Blagoevc,d, Laura J. Niedernhofere, Edwin H. Goodwinf, and Susan M. Baileya,1 aDepartment of Environmental and Radiological Health Sciences, Colorado State University, Fort Collins, CO 80523-1618; bPharmaceutical Genomics Division, Translational Genomics Research Institute, Phoenix, AZ 85004; cNational Science Foundation, Arlington, VA 22230; dDepartment of Physics Cavendish Laboratory, Cambridge University, Cambridge CB3 0HE, United Kingdom; eDepartment of Microbiology and Molecular Genetics, University of Pittsburgh, School of Medicine and Cancer Institute, Pittsburgh, PA 15261; and fKromaTiD Inc., Fort Collins, CO 80524 Edited* by José N. Onuchic, University of California San Diego, La Jolla, CA, and approved August 3, 2010 (received for review May 7, 2010) Werner syndrome and Bloom syndrome result from defects in the cell-cycle arrest known as senescence (12). Most human tissues lack RecQ helicases Werner (WRN) and Bloom (BLM), respectively, and sufficient telomerase activity to maintain telomere length through- display premature aging phenotypes. Similarly, XFE progeroid out life, limiting cell division potential. The majority of cancers syndrome results from defects in the ERCC1-XPF DNA repair endo- circumvent this tumor-suppressor mechanism by reactivating telo- nuclease. To gain insight into the origin of cellular senescence and merase (13), thus removing telomere shortening as a barrier to human aging, we analyzed the dependence of sister chromatid continuous proliferation. In some situations, a recombination- exchange (SCE) frequencies on location [i.e., genomic (G-SCE) vs. telo- based mechanism known as “alternative lengthening of telomeres” meric (T-SCE) DNA] in primary human fibroblasts deficient in WRN, (ALT) maintains telomere length in the absence of telomerase (14). -

Can Synthetic Lethality Approach Be Used with DNA Repair Genes for Primary and Secondary MDS?
Medical Oncology (2019) 36:99 https://doi.org/10.1007/s12032-019-1324-7 ORIGINAL PAPER Can synthetic lethality approach be used with DNA repair genes for primary and secondary MDS? Howard Lopes Ribeiro Junior1,2 · Roberta Taiane Germano de Oliveira1,2 · Daniela de Paula Borges1,2 · Marília Braga Costa1,2 · Izabelle Rocha Farias1,2 · Antônio Wesley Araújo dos Santos1,2 · Silvia Maria Meira Magalhães1,2 · Ronald Feitosa Pinheiro1,2,3 Received: 5 August 2019 / Accepted: 15 October 2019 / Published online: 30 October 2019 © Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Cancer-specifc defects in DNA repair pathways create the opportunity to employ synthetic lethality approach. Recently, GEMA (gene expression and mutation analysis) approach detected insufcient expression of BRCA or NHEJ (non-homol- ogous end joining) to predict PARP inhibitors response. We evaluated a possible role of DNA repair pathways using gene expression of single-strand break (XPA, XPC, XPG/ERCC5, CSA/ERCC8, and CSB/ERCC6) and double-strand break (ATM, BRCA1, BRCA2, RAD51, XRCC5, XRCC6, LIG4) in 92 patients with myelodysplastic syndrome (73 de novo, 9 therapy- related (t-MDS). Therapy-related MDS (t-MDS) demonstrated a signifcant downregulation of axis BRCA1-BRCA2-RAD51 comparing to normal controls (p = 0.048, p = 0.001, p = 0.001). XRCC6 showed signifcantly low expression in de novo MDS comparing to controls (p = 0.039) and for patients who presented chromosomal abnormalities (p = 0.047). Downregula- tion of LIG4 was consistently associated with poor prognostic markers in de novo MDS (hemoglobin < 8 g/dL (p = 0.040), neutrophils < 800/mm3 (p < 0.001), patients with excess of blasts (p = 0.001), very high (p = 0.002)/high IPSS-R (p = 0.043) and AML transformation (p < 0.001). -
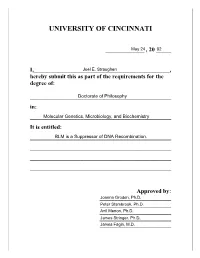
University of Cincinnati
UNIVERSITY OF CINCINNATI _____________ , 20 _____ I,______________________________________________, hereby submit this as part of the requirements for the degree of: ________________________________________________ in: ________________________________________________ It is entitled: ________________________________________________ ________________________________________________ ________________________________________________ ________________________________________________ Approved by: ________________________ ________________________ ________________________ ________________________ ________________________ BLM is a Suppressor of DNA Recombination A dissertation submitted to the Division of Research and Advanced Studies Of the University of Cincinnati In partial fulfillment of the Requirements for the degree of Doctorate of Philosophy (Ph.D.) In the Department of Molecular Genetics, Microbiology, and Biochemistry Of the College of Arts and Sciences 2002 by Joel E. Straughen B.S., The Ohio State University, 1985 M.D., University of Cincinnati, 2002 Committee Chair: Joanna Groden, Ph.D. i ABSTRACT Bloom’s syndrome (BS) is a rare, recessive chromosome breakage disorder characterized by small stature, sun sensitivity, facial erythema, immunodeficiency, female subfertility, male infertility, and a predisposition to a variety of cancers. When this body of work was started, the gene for Bloom’s syndrome (BLM)hadyettobe identified. This work presents characterization of the genomic region at BLM and the identification of BLM. With the cloning -

Somatic Mutations in Early Onset Luminal Breast Cancer
www.oncotarget.com Oncotarget, 2018, Vol. 9, (No. 32), pp: 22460-22479 Research Paper Somatic mutations in early onset luminal breast cancer Giselly Encinas1,*, Veronica Y. Sabelnykova2,*, Eduardo Carneiro de Lyra3, Maria Lucia Hirata Katayama1, Simone Maistro1, Pedro Wilson Mompean de Vasconcellos Valle1, Gláucia Fernanda de Lima Pereira1, Lívia Munhoz Rodrigues1, Pedro Adolpho de Menezes Pacheco Serio1, Ana Carolina Ribeiro Chaves de Gouvêa1, Felipe Correa Geyer1, Ricardo Alves Basso3, Fátima Solange Pasini1, Maria del Pilar Esteves Diz1, Maria Mitzi Brentani1, João Carlos Guedes Sampaio Góes3, Roger Chammas1, Paul C. Boutros2,4,5 and Maria Aparecida Azevedo Koike Folgueira1 1Instituto do Cancer do Estado de Sao Paulo, Departamento de Radiologia e Oncologia, Faculdade de Medicina FMUSP, Universidade de Sao Paulo, Sao Paulo, SP, Brazil 2Ontario Institute for Cancer Research, Toronto, Canada 3Instituto Brasileiro de Controle do Câncer, São Paulo, Brazil 4Department of Medical Biophysics, University of Toronto, Toronto, Canada 5Department of Pharmacology and Toxicology, University of Toronto, Toronto, Canada *These authors have contributed equally to this work Correspondence to: Maria Aparecida Azevedo Koike Folgueira, email: [email protected] Keywords: breast cancer; young patients; somatic mutation; germline mutation; luminal subtype Received: September 26, 2017 Accepted: March 06, 2018 Published: April 27, 2018 Copyright: Encinas et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License 3.0 (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. ABSTRACT Breast cancer arising in very young patients may be biologically distinct; however, these tumors have been less well studied. -

Messenger RNA Levels of XPAC and ERCC1 in Ovarian Cancer Tissue Correlate with Response to Platinum-Based Chemotherapy
Messenger RNA levels of XPAC and ERCC1 in ovarian cancer tissue correlate with response to platinum-based chemotherapy. M Dabholkar, … , J J Yu, E Reed J Clin Invest. 1994;94(2):703-708. https://doi.org/10.1172/JCI117388. Research Article Nucleotide excision repair is a DNA repair pathway that is highly conserved in nature, with analogous repair systems described in Escherichia coli, yeast, and mammalian cells. The rate-limiting step, DNA damage recognition and excision, is effected by the protein products of the genes ERCC1 and XPAC. We therefore assessed mRNA levels of ERCC1 and XPAC in malignant ovarian cancer tissues from 28 patients that were harvested before the administration of platinum- based chemotherapy. Cancer tissues from patients whose tumors were clinically resistant to therapy (n = 13) showed greater levels of total ERCC1 mRNA (P = 0.059), full length transcript of ERCC1 mRNA (P = 0.026), and XPAC mRNA (P = 0.011), as compared with tumor tissues from those individuals clinically sensitive to therapy (n = 15). In 19 of these tissues, the percentage of alternative splicing of ERCC1 mRNA was assessed. ERCC1 splicing was highly variable, with no difference observed between responders and nonresponders. The alternatively spliced species constituted 2-58% of the total ERCC1 mRNA in responders (median = 18%) and 4-71% in nonresponders (median = 13%). These data suggest greater activity of the DNA excision repair genes ERCC1 and XPAC in ovarian cancer tissues of patients clinically resistant to platinum compounds. These data also -

DNA Repair Pathway Profiling and Microsatellite Instability in Colorectal Cancer Jinshengyu,1, 6 Mary A
Human Cancer Biology DNA Repair Pathway Profiling and Microsatellite Instability in Colorectal Cancer JinshengYu,1, 6 Mary A. Mallon,2 Wanghai Zhang,1, 6 Robert R. Freimuth,1,4 Sharon Marsh,1, 6 Mark A.Watson,4,6 PaulJ. Goodfellow,2,3,6 andHowardL.McLeod1,3,5,6 Abstract Background: The ability to maintain DNA integrity is a critical cellular function. DNA repair is conducted by distinct pathways of genes, many of which are thought to be altered in colorectal cancer. However, there has been little characterization of these pathways in colorectal cancer. Method: By using the TaqMan real-time quantitative PCR, RNA expression profiling of 20 DNA repair pathway genes was done in matched tumor and normal tissues from 52 patients with Dukes’C colorectal cancer. Results: The relative mRNA expression level across the 20 DNA repair pathway genes varied considerably, and the individual variability was also quite large, with an 85.4 median fold change in the tumor tissue genes and a 127.2 median fold change in the normal tissue genes. Tumor- normal differential expression was found in 13 of 20 DNA repair pathway genes (only XPA had a lower RNA level in the tumor samples; the other 12 genes had significantly higher tumor levels, all P < 0.01). Coordinated expression of ERCC6, HMG1, MSH2,andPOLB (RS z 0.60) was observed in the tumor tissues (all P < 0.001). Apoptosis index was not correlated with expression of the 20 DNA repair pathway genes. MLH1 and XRCC1 RNA expression was correlated with microsatellite instability status (P = 0.045 and 0.020, respectively).