Download 2012 Annual Report .PDF
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sunday.Sept.06.Overnight 261 Songs, 14.2 Hours, 1.62 GB
Page 1 of 8 ...sunday.Sept.06.Overnight 261 songs, 14.2 hours, 1.62 GB Name Time Album Artist 1 Go Now! 3:15 The Magnificent Moodies The Moody Blues 2 Waiting To Derail 3:55 Strangers Almanac Whiskeytown 3 Copperhead Road 4:34 Shut Up And Die Like An Aviator Steve Earle And The Dukes 4 Crazy To Love You 3:06 Old Ideas Leonard Cohen 5 Willow Bend-Julie 0:23 6 Donations 3 w/id Julie 0:24 KSZN Broadcast Clips Julie 7 Wheels Of Love 2:44 Anthology Emmylou Harris 8 California Sunset 2:57 Old Ways Neil Young 9 Soul of Man 4:30 Ready for Confetti Robert Earl Keen 10 Speaking In Tongues 4:34 Slant 6 Mind Greg Brown 11 Soap Making-Julie 0:23 12 Volunteer 1 w/ID- Tony 1:20 KSZN Broadcast Clips 13 Quittin' Time 3:55 State Of The Heart Mary Chapin Carpenter 14 Thank You 2:51 Bonnie Raitt Bonnie Raitt 15 Bootleg 3:02 Bayou Country (Limited Edition) Creedence Clearwater Revival 16 Man In Need 3:36 Shoot Out the Lights Richard & Linda Thompson 17 Semicolon Project-Frenaudo 0:44 18 Let Him Fly 3:08 Fly Dixie Chicks 19 A River for Him 5:07 Bluebird Emmylou Harris 20 Desperadoes Waiting For A Train 4:19 Other Voices, Too (A Trip Back To… Nanci Griffith 21 uw niles radio long w legal id 0:32 KSZN Broadcast Clips 22 Cold, Cold Heart 5:09 Timeless: Hank Williams Tribute Lucinda Williams 23 Why Do You Have to Torture Me? 2:37 Swingin' West Big Sandy & His Fly-Rite Boys 24 Madmax 3:32 Acoustic Swing David Grisman 25 Grand Canyon Trust-Terry 0:38 26 Volunteer 2 Julie 0:48 KSZN Broadcast Clips Julie 27 Happiness 3:55 So Long So Wrong Alison Krauss & Union Station -

The Twenty Greatest Music Concerts I've Ever Seen
THE TWENTY GREATEST MUSIC CONCERTS I'VE EVER SEEN Whew, I'm done. Let me remind everyone how this worked. I would go through my Ipod in that weird Ipod alphabetical order and when I would come upon an artist that I have seen live, I would replay that concert in my head. (BTW, since this segment started I no longer even have an ipod. All my music is on my laptop and phone now.) The number you see at the end of the concert description is the number of times I have seen that artist live. If it was multiple times, I would do my best to describe the one concert that I considered to be their best. If no number appears, it means I only saw that artist once. Mind you, I have seen many artists live that I do not have a song by on my Ipod. That artist is not represented here. So although the final number of concerts I have seen came to 828 concerts (wow, 828!), the number is actually higher. And there are "bar" bands and artists (like LeCompt and Sam Butera, for example) where I have seen them perform hundreds of sets, but I counted those as "one," although I have seen Lecompt in "concert" also. Any show you see with the four stars (****) means they came damn close to being one of the Top Twenty, but they fell just short. So here's the Twenty. Enjoy and thanks so much for all of your input. And don't sue me if I have a date wrong here and there. -

Voices in the Hall: Sam Bush (Part 1) Episode Transcript
VOICES IN THE HALL: SAM BUSH (PART 1) EPISODE TRANSCRIPT PETER COOPER Welcome to Voices in the Hall, presented by the Country Music Hall of Fame and Museum. I’m Peter Cooper. Today’s guest is a pioneer of New-grass music, Sam Bush. SAM BUSH When I first started playing, my dad had these fiddle albums. And I loved to listen to them. And then realized that one of the things I liked about them was the sound of the fiddle and the mandolin playing in unison together. And that’s when it occurred to me that I was trying on the mandolin to note it like a fiddle player notes. Then I discovered Bluegrass and the great players like Bill Monroe of course. You can specifically trace Bluegrass music to the origins. That it was started by Bill Monroe after he and his brother had a duet of mandolin and guitar for so many years, the Monroe Brothers. And then when he started his band, we're just fortunate that he was from the state of Kentucky, the Bluegrass State. And that's why they called them The Bluegrass Boys. And lo and behold we got Bluegrass music out of it. PETER COOPER It’s Voices in the Hall, with Sam Bush. “Callin’ Baton Rouge” – New Grass Revival (Best Of / Capitol) PETER COOPER “Callin’ Baton Rouge," by the New Grass Revival. That song was a prime influence on Garth Brooks, who later recorded it. Now, New Grass Revival’s founding member, Sam Bush, is a mandolin revolutionary whose virtuosity and broad- minded approach to music has changed a bunch of things for the better. -

'Standards Must Rise...' Is Feb
A gourmet's delight There will be an organic dinner this Friday, Jan. 30 at 6:30 p.m. in Cabin 4. All are invited. Bring food or pay $1. Change the world; eat a prune There will be a lecture today, Tuesday, entitled "World Revolu- tion through Dietary Change :The Practice and Philosophy of Natural Foods" at 4:30 in F-101. The possibility will be discussed of societal change through a change in our habits and attitudes toward food, and practical suggestions will be given on natural food selection and preparation. This is the first in a series of talks, discussions and cooking classes to be held in the future. What's up Josh? There will be a color film nigh Adventure on the College Campus", featuring Josh McDowell (author of the Christian Higher Ed. Chancellor speoks to Stockton students best-seller "Evidence that Demands a Verdict") in G-208 on Monday, Feb. 2 at 8 pm. The film is free. Defect now There is still time to sign up for the trip to Russia. The deadline 'Standards must rise...' is Feb. 3. The cost is now $699, and. it will take place from By Wayne Wippermann throughout the state . are being March 5-13. Contact Marcia Satin, ext. 380 for more information. Ralph Dungan, Chancellor of cut. r Higher Education, paid a very This procedure would make Permanent press VA regulations low-keyed visit to Stockton Col- the prospective student feel Due to a new wrinkle in the VA regulations and policies it has lege last Friday. -

GRAM PARSONS LYRICS Compiled by Robin Dunn & Chrissie Van Varik
GRAM PARSONS LYRICS Compiled by Robin Dunn & Chrissie van Varik. As performed in principal recordings (or demos) by or with Gram Parsons or, in the case of Gram Parsons compositions, performed by others. Gram often varied, adapted or altered the lyrics to non-Parsons compositions; those listed here are as sung by him. Gram’s birth name was Ingram Cecil Connor III. However, ‘Gram Parsons’ is used throughout this document. Following his father’s suicide, Gram’s mother Avis subsequently married Robert Parsons, whose surname Gram adopted. Born Ingram Cecil Connor III, 5th November 1946 - 19th September 1973 and credited as being the founder of modern ‘country-rock’, Gram Parsons was hugely influenced by The Everly Brothers and included a number of their songs in his live and recorded repertoire – most famously ‘Love Hurts’, a truly wonderful rendition with a young Emmylou Harris. He also recorded ‘Brand New Heartache’ and ‘Sleepless Nights’ – also the title of a posthumous album – and very early, in 1967, ‘When Will I Be Loved’. Many would attest that ‘country-rock’ kicked off with The Everly Brothers, and in the late sixties the album Roots was a key and acknowledged influence, but that is not to deny Parsons huge role in developing it. Gram Parsons is best known for his work within the country genre but he also mixed blues, folk, and rock to create what he called “Cosmic American Music”. While he was alive, Gram Parsons was a cult figure that never sold many records but influenced countless fellow musicians, from the Rolling Stones to The Byrds. -
1 Column Unindented
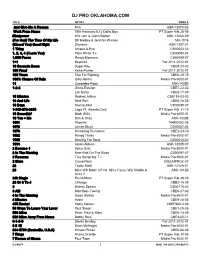
DJ PRO OKLAHOMA.COM TITLE ARTIST SONG # Just Give Me A Reason Pink ASK-1307A-08 Work From Home Fifth Harmony ft.Ty Dolla $ign PT Super Hits 28-06 #thatpower Will.i.am & Justin Bieber ASK-1306A-09 (I've Had) The Time Of My Life Bill Medley & Jennifer Warnes MH-1016 (Kissed You) Good Night Gloriana ASK-1207-01 1 Thing Amerie & Eve CB30053-02 1, 2, 3, 4 (I Love You) Plain White T's CB30094-04 1,000 Faces Randy Montana CB60459-07 1+1 Beyonce Fall 2011-2012-01 10 Seconds Down Sugar Ray CBE9-23-02 100 Proof Kellie Pickler Fall 2011-2012-01 100 Years Five For Fighting CBE6-29-15 100% Chance Of Rain Gary Morris Media Pro 6000-01 11 Cassadee Pope ASK-1403B 1-2-3 Gloria Estefan CBE7-23-03 Len Barry CBE9-11-09 15 Minutes Rodney Atkins CB5134-03-03 18 And Life Skid Row CBE6-26-05 18 Days Saving Abel CB30088-07 1-800-273-8255 Logic Ft. Alessia Cara PT Super Hits 31-10 19 Somethin' Mark Wills Media Pro 6000-01 19 You + Me Dan & Shay ASK-1402B 1901 Phoenix PHM1002-05 1973 James Blunt CB30067-04 1979 Smashing Pumpkins CBE3-24-10 1982 Randy Travis Media Pro 6000-01 1985 Bowling For Soup CB30048-02 1994 Jason Aldean ASK-1303B-07 2 Become 1 Spice Girls Media Pro 6000-01 2 In The Morning New Kids On The Block CB30097-07 2 Reasons Trey Songz ftg. T.I. Media Pro 6000-01 2 Stars Camp Rock DISCMPRCK-07 22 Taylor Swift ASK-1212A-01 23 Mike Will Made It Feat. -

Recorded Jazz in the 20Th Century
Recorded Jazz in the 20th Century: A (Haphazard and Woefully Incomplete) Consumer Guide by Tom Hull Copyright © 2016 Tom Hull - 2 Table of Contents Introduction................................................................................................................................................1 Individuals..................................................................................................................................................2 Groups....................................................................................................................................................121 Introduction - 1 Introduction write something here Work and Release Notes write some more here Acknowledgments Some of this is already written above: Robert Christgau, Chuck Eddy, Rob Harvilla, Michael Tatum. Add a blanket thanks to all of the many publicists and musicians who sent me CDs. End with Laura Tillem, of course. Individuals - 2 Individuals Ahmed Abdul-Malik Ahmed Abdul-Malik: Jazz Sahara (1958, OJC) Originally Sam Gill, an American but with roots in Sudan, he played bass with Monk but mostly plays oud on this date. Middle-eastern rhythm and tone, topped with the irrepressible Johnny Griffin on tenor sax. An interesting piece of hybrid music. [+] John Abercrombie John Abercrombie: Animato (1989, ECM -90) Mild mannered guitar record, with Vince Mendoza writing most of the pieces and playing synthesizer, while Jon Christensen adds some percussion. [+] John Abercrombie/Jarek Smietana: Speak Easy (1999, PAO) Smietana -

What You No. .John Hartford, with Benny Martin, David Briggs, Sam Bush, Et Al
NJ,)~ Knows- What You no. .John Hartford, with Benny Martin, David Briggs, Sam Bush, et al. 12 selections, vocal and instrumental, stereo. Flying Fish 028, 3320 Halstad St., Chicago, Ill. 60657, 1976. Reviewed by Bob Blackman About the best thing that can be said for Nobody Knows What You Do is that it's a slight improvement over John Hartford's previous record, Mark Twang (reviewed in Folklore Forum 10 Gpring)1977; 10:l). This is due not to Hartford but entirely to the welcome addition of some fine sidemen (absent on the earlier release). Their hot picking compensates for the further deterioration of Hartford's songwriting. Hartford's sense of humor, always his strongest point, has become plain silly. Lyrics like "The Golden Globe Award" (singing the praises of his girl's "golden globes") and "Granny Won'tcha Smoke Some Marijuana" are at a high school level of self-conscious sniggering. "The False Hearted Tenor Waltz" expresses his desire to sing that high lonesome bluegrass tenor, and would be one of the record's more successful cuts if Hartford's "comic" falsetto weren't so grating. The title song is so completely pointless that it's hard to understand why anyone would bother to write it, let alone record it. The one serious song is "In Tall Buildings," another in a long line of "Oh, life in the city is such a drag" compositions that are churned out by every songwriter in the business. The lyrics here are as trite as most such songs, but at least it's nice to hear one track sung "straight." Most of the other so-called songs are just words thrown together between long instrumental breaks. -

NJDARM: Collection Guide
NJDARM: Collection Guide - NEW JERSEY STATE ARCHIVES COLLECTION GUIDE Record Group: Col. Henry Hartford (1937-1919) Series: Papers, 1861-1929 Accession #: 1993.046 Series #: PHART001 Guide Date: 2/1994 (JK) Volume: 1 c.f. [1 box, 1 volume, and 12 oversized folders] Content Note | Contents Biographical Note Born 8 February 1837 in Coleraine, County Londonderry, Ireland, Henry Hartford was the eldest child of William and Martha (Leslie) Hartford. He attended private schools in Ireland, and at the age of 18 decided to follow his brother William to the United States. After Henry's arrival in New York City in 1855, the Hartford brothers were employed as clerks in a grocery store. By the 1860s, their widowed mother and twin sisters Elizabeth and Susan joined them. At the outbreak of the Civil War, both Henry and William Hartford joined the Union forces--Henry enlisting in Company K of the First Regiment, New Jersey Militia, for three-months' service. In July 1861, the First Militia was reorganized as the 8th New Jersey Volunteer Regiment. Hartford became first sergeant of Company F on 31 August 1861, and was promoted to second lieutenant on 10 December the following year. On 3 October 1863, he was promoted to first lieutenant and transferred to Company E. Hartford was made captain of Company C on 11 June 1864, and in December of the same year he rose to the rank of major and was made regimental commander of the 8th New Jersey, replacing Col. John Ramsey. After distinguishing himself in battle at Petersburg, Virginia, he was made brevet lieutenant colonel on 2 April 1865, and later lieutenant colonel. -

Jazz Collection: Alison Krauss – Die Stimme Des Bluegrass Dienstag, 13
Jazz Collection: Alison Krauss – die Stimme des Bluegrass Dienstag, 13. Juli 2021, 21.00 – 22.00 Uhr, SRF 2 Kultur Samstag, 17. Juli 2021, 17.06 – 18.30 Uhr, SRF 2 Kultur (mit Bonustracks) Mit 27 erhaltenen Grammys ist Alison Krauss eine der prominentesten Musikerinnen der USA. Ihre herausragende Popularität geht weit über ihre angestammte Szene der akustischen Roots Music, des Bluegrass hinaus. Einiges davon hat mit ihrer unvergleichlichen Stimme und ihren instrumentalen Fähigkeiten als Fiddlerin zu tun, aber auch mit ihrem Willen, stets über die Grenzen hinauszuschauen. Zu ihrem 50. Geburtstag spricht Eric Facon mit der Schweizer Country-Sängerin und - Mandolinistin Jessie Hardegger von Jessie & the Gents. Gast: Jessie Hardegger Redaktion und Moderation: Eric Facon Interpret*in Titel Komponist*in Album / Label Alison Krauss Everytime You Say Goodbye John Pennell Now That I’ve Found You / New Rounder & Union Station Records (1995) Alison Krauss When God Dips His Pen of Ralph Hill The Cox Family – Everybody’s Reaching Out & Cox Family Love in My Heart for Someone / New Rounder Records (1993) Alison Krauss When You Say Nothing at All Don Schlitz Now That I’ve Found You / New Rounder & Union Station Records (1995) Alison Krauss Oh, Atlanta Mick Ralphs Now That I’ve Found You / New Rounder Records (1995) Alison Krauss Down to the River to Pray Traditional Soundtrack zu «O Brother Where Art Thou» / Universal (2000) Alison Krauss Cluck Old Hen Traditional Alison Krauss & Union Station Live / New & Union Station Rounders Records (2002) Brad Paisley Whiskey Lullaby Bill Anderson Brad Paisley: Mud on the Tires / Arista & Alison Krauss Nashville (2003) Robert Plant Gone Gone Gone Phil Everly Robert Plant & Alison Krauss: Raising Sand / & Alison Krauss Decca Records (2007) Alison Krauss It’s Goodbye And So Long Raymond Couture Windy City / Capitol Records (2017) Alison Krauss Gentle on My Mind John Hartford Windy City / Capitol Records (2017) Bonustracks (nur am Samstag) Interpret*in Titel Komponist*in Album / Label Alison Krauss I’ll Fly Away Albert E. -

Great Instrumental
I grew up during the heyday of pop instrumental music in the 1950s and the 1960s (there were 30 instrumental hits in the Top 40 in 1961), and I would listen to the radio faithfully for the 30 seconds before the hourly news when they would play instrumentals (however the first 45’s I bought were vocals: Bimbo by Jim Reeves in 1954, The Ballad of Davy Crockett with the flip side Farewell by Fess Parker in 1955, and Sixteen Tons by Tennessee Ernie Ford in 1956). I also listened to my Dad’s 78s, and my favorite song of those was Raymond Scott’s Powerhouse from 1937 (which was often heard in Warner Bros. cartoons). and to records that my friends had, and that their parents had - artists such as: (This is not meant to be a complete or definitive list of the music of these artists, or a definitive list of instrumental artists – rather it is just a list of many of the instrumental songs I heard and loved when I was growing up - therefore this list just goes up to the early 1970s): Floyd Cramer (Last Date and On the Rebound and Let’s Go and Hot Pepper and Flip Flop & Bob and The First Hurt and Fancy Pants and Shrum and All Keyed Up and San Antonio Rose and [These Are] The Young Years and What’d I Say and Java and How High the Moon), The Ventures (Walk Don't Run and Walk Don’t Run ‘64 and Perfidia and Ram-Bunk-Shush and Diamond Head and The Cruel Sea and Hawaii Five-O and Oh Pretty Woman and Go and Pedal Pusher and Tall Cool One and Slaughter on Tenth Avenue), Booker T. -

For Folksong in America
Project for Folksong In America Cheryl Hudson May 2.5, 1973 Fo 134 8:1600°. u '3.,:<.: ! .· '· When this project started, .the plan was to interview several people, in their early twenties or so, ·who played guitar and sang. A primary reason was to find out if one could generalize about them as a group, to see if they had gone through similar "stages" of doing things musically as they had progressed, well, maybe not progressed, .but at least stages they had . gone . through since they learned _to ·play. The original intentions had been to interview people ranging from amateur to· rather professional, but this pr9ved to be slight- ly over-ambitious. People were not as easy to get ,and interview as I had anticipated, and being excited about the project, I had undere~tlmated the amount of work involved. Perhap~ 1t is · just. as well, for' it ended up that there was enough material to work wt.th, but not· so much as at throughly overwhelm me. I interviewed four people, and then also ui:~ed . m;}[se.lf and my experiences·, as well as the knowledge I have of other people who were not interviewed. George Murphy was the first person I talked with. He is neither an excellent guitar player, nor does he have the stereotype "good" voice, but he has, at many . times, played around at coffeehouses and more nightclub type places for money. Cathy Johnson was · the ne~t person interviewed. She was the least proficient, musically. She plays mainly b8:sic chords and does not sing well (does no.t hit notes right on pitch, or hold J t~em there).