Blue Cross and BCN Utilization Management Medical Drug List
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Spinraza™ (Nusinersen)
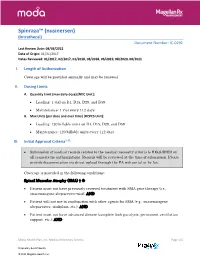
Spinraza™ (nusinersen) (Intrathecal) Document Number: IC-0291 Last Review Date: 08/03/2021 Date of Origin: 01/31/2017 Dates Reviewed: 01/2017, 02/2017, 01/2018, 08/2018, 06/2019, 08/2020, 08/2021 I. Length of Authorization Coverage will be provided annually and may be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: • Loading: 1 vial on D1, D15, D29, and D59 • Maintenance: 1 vial every 112 days B. Max Units (per dose and over time) [HCPCS Unit]: • Loading: 120 billable units on D1, D15, D29, and D59 • Maintenance: 120 billable units every 112 days III. Initial Approval Criteria1-12 • Submission of medical records related to the medical necessity criteria is REQUIRED on all requests for authorizations. Records will be reviewed at the time of submission. Please provide documentation via direct upload through the PA web portal or by fax. Coverage is provided in the following conditions: Spinal Muscular Atrophy (SMA) † Ф • Patient must not have previously received treatment with SMA gene therapy (i.e., onasemnogene abeparvovec-xioi); AND • Patient will not use in combination with other agents for SMA (e.g., onasemnogene abeparvovec, risdiplam, etc.); AND • Patient must not have advanced disease (complete limb paralysis, permanent ventilation support, etc.); AND Moda Health Plan, Inc. Medical Necessity Criteria Page 1/5 Proprietary & Confidential © 2021 Magellan Health, Inc. • Patient must have the following laboratory tests at baseline and prior to each administration*: platelet count, prothrombin time; activated -

Pertuzumab and Trastuzumab: the Rationale Way to Synergy
Anais da Academia Brasileira de Ciências (2016) 88(1 Suppl.): 565-577 (Annals of the Brazilian Academy of Sciences) Printed version ISSN 0001-3765 / Online version ISSN 1678-2690 http://dx.doi.org/10.1590/0001-3765201620150178 www.scielo.br/aabc Pertuzumab and trastuzumab: the rationale way to synergy SANDRINE RICHARD1, FRÉDÉRIC SELLE1, JEAN-PIERRE LOTZ1,2, AHMED KHALIL1, JOSEPH GLIGOROV1,2 and DANIELE G. SOARES1 1Medical Oncology Department, APREC (Alliance Pour la Recherche En Cancérologie), Tenon Hospital (Hôpitaux Universitaires de l’Est-Parisien, AP-HP), rue de la Chine, 75020 Paris, France 2Institut Universitaire de Cancérologie Université Pierre et Marie Curie (IUC-UPMC Univ Paris 06), Sorbonne Universités, 4 place Jussieu, 75005 Paris, France Manuscript received on March 13, 2015; accepted for publication on May 5, 2015 ABSTRACT It has now been 15 years since the HER2-targeted monoclonal antibody trastuzumab was introduced in clinical and revolutionized the treatment of HER2-positive breast cancer patients. Despite this achievement, most patients with HER2-positive metastatic breast cancer still show progression of their disease, highlighting the need for new therapies. The continuous interest in novel targeted agents led to the development of pertuzumab, the first in a new class of agents, the HER dimerization inhibitors. Pertuzumab is a novel recombinant humanized antibody directed against extracellular domain II of HER2 protein that is required for the heterodimerization of HER2 with other HER receptors, leading to the activation of downstream signalling pathways. Pertuzumab combined with trastuzumab plus docetaxel was approved for the first-line treatment of patients with HER2-positive metastatic breast cancer and is currently used as a standard of care in this indication. -

Minutes of the CHMP Meeting 14-17 September 2020
13 January 2021 EMA/CHMP/625456/2020 Corr.1 Human Medicines Division Committee for medicinal products for human use (CHMP) Minutes for the meeting on 14-17 September 2020 Chair: Harald Enzmann – Vice-Chair: Bruno Sepodes Disclaimers Some of the information contained in these minutes is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also vary during the course of the review. Additional details on some of these procedures will be published in the CHMP meeting highlights once the procedures are finalised and start of referrals will also be available. Of note, these minutes are a working document primarily designed for CHMP members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the minutes cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on- going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006). 1 Addition of the list of participants Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2020. -

Pharmacokinetics and Exposure-Response Relationship of Teprotumumab Frst 3 Months, Unless Determined to Be Medically Necessary
Clinical Pharmacokinetics https://doi.org/10.1007/s40262-021-01003-3 ORIGINAL RESEARCH ARTICLE Pharmacokinetics and Exposure‑Response Relationship of Teprotumumab, an Insulin‑Like Growth Factor‑1 Receptor‑Blocking Antibody, in Thyroid Eye Disease Yan Xin1 · Fengyan Xu2 · Yuying Gao2 · Nivedita Bhatt1 · Jason Chamberlain1 · Saba Sile1 · Suzy Hammel1 · Robert J. Holt1 · Srini Ramanathan1 Accepted: 10 February 2021 © The Author(s) 2021 Abstract Background and Objective Thyroid eye disease (TED) is characterized by infammation/expansion of orbital tissues, prop- tosis, and diplopia. Teprotumumab is the frst US Food and Drug Administration-approved therapy for TED, administered as an initial intravenous infusion of 10 mg/kg followed by 20 mg/kg every 3 weeks for an additional seven infusions. The objec- tive of this article is to discuss the pharmacokinetics and exposure-response profle for teprotumumab in patients with TED. Methods A population pharmacokinetic analysis was performed to characterize pharmacokinetics and select dosing in patients with TED. Exposure-response was evaluated for efcacy (proptosis response, clinical activity score categorical response, and diplopia response) and safety (hyperglycemia, muscle spasms, and hearing impairment) parameters. Results Teprotumumab pharmacokinetics was linear in patients with TED, with low systemic clearance (0.334 L/day), low volume of distribution (3.9 and 4.2 L for the central and peripheral compartment, respectively), and a long elimination half- life (19.9 days). The approved dosing regimen provided > 20 µg/mL for > 90% insulin-like growth factor 1 receptor saturation throughout the dosing interval. Model-predicted mean (± standard deviation) steady-state area under the concentration-time curve, peak, and trough concentrations in patients with TED were 131 (± 30.9) mg∙h/mL, 643 (± 130) µg/mL, and 157 (± 50.6) µg/mL, respectively. -

2017 ANNUAL REPORT | Translating SCIENCE • Transforming LIVES OUR COMMITMENT Make Every Day Count at PTC, Patients Are at the Center of Everything We Do
20 YEARS OF COMMITMENT 2017 ANNUAL REPORT | Translating SCIENCE • Transforming LIVES OUR COMMITMENT Make every day count At PTC, patients are at the center of everything we do. We have the opportunity to support patients and families living with rare disorders through their journey. We know that every day matters and we are committed to making a difference. OUR SCIENCE Our scientists are finding new ways to regulate biology to control disease We have several scientific research platforms focused on modulating protein expression within the cell that we believe have the potential to address many rare genetic disorders. OUR PEOPLE Care for each other, our community, and for the needs of our patients At PTC, we are looking at drug discovery and development in a whole new light, bringing new technologies and approaches to developing medicines for patients living with rare disorders and cancer. We strive every day to be better than we were the day before. At PTC Therapeutics, it is our mission to provide access to best-in-class treatments for patients who have an unmet need. We are a science-led, global biopharmaceutical company focused on the discovery, development and commercialization of clinically-differentiated medicines that provide benefits to patients with rare disorders. Founded 20 years ago, PTC Therapeutics has successfully launched two rare disorder products and has a global commercial footprint. This success is the foundation that drives investment in a robust pipeline of transformative medicines and our mission to provide access to best-in-class treatments for patients who have an unmet medical need. As we celebrate our 20th year of bringing innovative therapies to patients affected by rare disorders, we reflect on our unwavering commitment to our patients, our science and our employees. -

Predictive QSAR Tools to Aid in Early Process Development of Monoclonal Antibodies
Predictive QSAR tools to aid in early process development of monoclonal antibodies John Micael Andreas Karlberg Published work submitted to Newcastle University for the degree of Doctor of Philosophy in the School of Engineering November 2019 Abstract Monoclonal antibodies (mAbs) have become one of the fastest growing markets for diagnostic and therapeutic treatments over the last 30 years with a global sales revenue around $89 billion reported in 2017. A popular framework widely used in pharmaceutical industries for designing manufacturing processes for mAbs is Quality by Design (QbD) due to providing a structured and systematic approach in investigation and screening process parameters that might influence the product quality. However, due to the large number of product quality attributes (CQAs) and process parameters that exist in an mAb process platform, extensive investigation is needed to characterise their impact on the product quality which makes the process development costly and time consuming. There is thus an urgent need for methods and tools that can be used for early risk-based selection of critical product properties and process factors to reduce the number of potential factors that have to be investigated, thereby aiding in speeding up the process development and reduce costs. In this study, a framework for predictive model development based on Quantitative Structure- Activity Relationship (QSAR) modelling was developed to link structural features and properties of mAbs to Hydrophobic Interaction Chromatography (HIC) retention times and expressed mAb yield from HEK cells. Model development was based on a structured approach for incremental model refinement and evaluation that aided in increasing model performance until becoming acceptable in accordance to the OECD guidelines for QSAR models. -

Where Do Novel Drugs of 2016 Fit In?
FORMULARY JEOPARDY: WHERE DO NOVEL DRUGS OF 2016 FIT IN? Maabo Kludze, PharmD, MBA, CDE, BCPS, Associate Director Elizabeth A. Shlom, PharmD, BCPS, SVP & Director Clinical Pharmacy Program Acurity, Inc. Privileged and Confidential August 15, 2017 Privileged and Confidential Program Objectives By the end of the presentation, the pharmacist or pharmacy technician participant will be able to: ◆ Identify orphan drugs and first-in-class medications approved by the FDA in 2016. ◆ Describe the role of new agents approved for use in oncology patients. ◆ Identify and discuss the role of novel monoclonal antibodies. ◆ Discuss at least two new medications that address public health concerns. Neither Dr. Kludze nor Dr. Shlom have any conflicts of interest in regards to this presentation. Privileged and Confidential 2016 NDA Approvals (NMEs/BLAs) ◆ Nuplazid (primavanserin) P ◆ Adlyxin (lixisenatide) ◆ Ocaliva (obeticholic acid) P, O ◆ Anthim (obitoxaximab) O ◆ Rubraca (rucaparib camsylate) P, O ◆ Axumin (fluciclovive F18) P ◆ Spinraza (nusinersen sodium) P, O ◆ Briviact (brivaracetam) ◆ Taltz (ixekizumab) ◆ Cinqair (reslizumab) ◆ Tecentriq (atezolizumab) P ◆ Defitelio (defibrotide sodium) P, O ◆ Venclexta (venetoclax) P, O ◆ Epclusa (sofosburvir and velpatasvir) P ◆ Xiidra (lifitigrast) P ◆ Eucrisa (crisaborole) ◆ Zepatier (elbasvir and grazoprevir) P ◆ Exondys 51 (eteplirsen) P, O ◆ Zinbyrta (daclizumab) ◆ Lartruvo (olaratumab) P, O ◆ Zinplava (bezlotoxumab) P ◆ NETSTPOT (gallium Ga 68 dotatate) P, O O = Orphan; P = Priority Review; Red = BLA Privileged and Confidential History of FDA Approvals Privileged and Confidential Orphan Drugs ◆FDA Office of Orphan Products Development • Orphan Drug Act (1983) – drugs and biologics . “intended for safe and effective treatment, diagnosis or prevention of rare diseases/disorders that affect fewer than 200,000 people in the U.S. -

New Brunswick Drug Plans Formulary
New Brunswick Drug Plans Formulary August 2019 Administered by Medavie Blue Cross on Behalf of the Government of New Brunswick TABLE OF CONTENTS Page Introduction.............................................................................................................................................I New Brunswick Drug Plans....................................................................................................................II Exclusions............................................................................................................................................IV Legend..................................................................................................................................................V Anatomical Therapeutic Chemical (ATC) Classification of Drugs A Alimentary Tract and Metabolism 1 B Blood and Blood Forming Organs 23 C Cardiovascular System 31 D Dermatologicals 81 G Genito Urinary System and Sex Hormones 89 H Systemic Hormonal Preparations excluding Sex Hormones 100 J Antiinfectives for Systemic Use 107 L Antineoplastic and Immunomodulating Agents 129 M Musculo-Skeletal System 147 N Nervous System 156 P Antiparasitic Products, Insecticides and Repellants 223 R Respiratory System 225 S Sensory Organs 234 V Various 240 Appendices I-A Abbreviations of Dosage forms.....................................................................A - 1 I-B Abbreviations of Routes................................................................................A - 4 I-C Abbreviations of Units...................................................................................A -

How Do We Treat Life-Threatening Anemia in a Jehovah's Witness
HOW DO I...? How do we treat life-threatening anemia in a Jehovah’s Witness patient? Joseph A. Posluszny Jr and Lena M. Napolitano he management of Jehovah’s Witness (JW) The refusal of allogeneic human blood and blood prod- patients with anemia and bleeding presents a ucts by Jehovah’s Witness (JW) patients complicates clinical dilemma as they do not accept alloge- the treatment of life-threatening anemia. For JW neic human blood or blood product transfu- patients, when hemoglobin (Hb) levels decrease Tsions.1,2 With increased understanding of the JW patient beyond traditional transfusion thresholds (<7 g/dL), beliefs and blood product limitations, the medical com- alternative methods to allogeneic blood transfusion can munity can better prepare for optimal treatment of severe be utilized to augment erythropoiesis and restore life-threatening anemia in JW patients. endogenous Hb levels. The use of erythropoietin- Lower hemoglobin (Hb) is associated with increased stimulating agents and intravenous iron has been mortality risk in JW patients. In a study of 300 patients shown to restore red blood cell and Hb levels in JW who refused blood transfusion, for every 1 g/dL decrease patients, although these effects may be significantly in Hb below 8 g/dL, the odds of death increased 2.5-fold delayed. When JW patients have evidence of life- (Fig. 1).3 A more recent single-center update of JW threatening anemia (Hb <5 g/dL), oxygen-carrying patients (n = 293) who declined blood transfusion capacity can be supplemented with the administration reported an overall mortality rate of 8.2%, with a twofold of Hb-based oxygen carriers (HBOCs). -

Intravenous Iron Replacement Therapy (Feraheme®, Injectafer®, & Monoferric®)
UnitedHealthcare® Commercial Medical Benefit Drug Policy Intravenous Iron Replacement Therapy (Feraheme®, Injectafer®, & Monoferric®) Policy Number: 2021D0088F Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Community Plan Policy Coverage Rationale ....................................................................... 1 • Intravenous Iron Replacement Therapy (Feraheme®, Definitions ...................................................................................... 3 Injectafer®, & Monoferric®) Applicable Codes .......................................................................... 3 Background.................................................................................... 4 Benefit Considerations .................................................................. 4 Clinical Evidence ........................................................................... 5 U.S. Food and Drug Administration ............................................. 7 Centers for Medicare and Medicaid Services ............................. 8 References ..................................................................................... 8 Policy History/Revision Information ............................................. 9 Instructions for Use ....................................................................... 9 Coverage Rationale See Benefit Considerations This policy refers to the following intravenous iron replacements: Feraheme® (ferumoxytol) Injectafer® (ferric carboxymaltose) Monoferric® (ferric derisomaltose)* The following -

Oregon Medicaid Pharmaceutical Services Prior Authorization Criteria
Oregon Medicaid Pharmaceutical Services Prior Authorization Criteria HEALTH SYSTEMS DIVISION Prior authorization (PA) criteria for fee-for-service prescriptions for Oregon Health Plan clients March 1, 2021 Contents Contents ................................................................................................................................................................ 2 Introduction........................................................................................................................................................... 7 About this guide ......................................................................................................................................... 7 How to use this guide ................................................................................................................................. 7 Administrative rules and supplemental information .................................................................................. 7 Update information............................................................................................................................................... 8 Effective March 1, 2021 ............................................................................................................................ 8 Substantive updates and new criteria ............................................................................................. 8 Clerical changes ............................................................................................................................ -

Refreshing the Biologic Pipeline 2020
news feature Credit: Science Lab / Alamy Stock Photo Refreshing the biologic pipeline 2020 In the absence of face-to-face meetings, FDA and industry implemented regulatory workarounds to maintain drug and biologics approvals. These could be here to stay. John Hodgson OVID-19 might have been expected since 1996) — a small miracle in itself “COVID-19 confronted us with the need to severely impair drug approvals (Fig. 1 and Table 1). to better triage sponsors’ questions,” says Cin 2020. In the event, however, To the usual crop of rare disease and Peter Marks, the director of the Center for industry and regulators delivered a small genetic-niche cancer treatments, 2020 Biologics Evaluation and Research (CBER) miracle. They found workarounds and also added a chimeric antigen receptor at the FDA. “That was perhaps the single surrogate methods of engagement. Starting (CAR)-T cell therapy with a cleaner biggest takeaway from the pandemic related in January 2020, when the outbreak veered manufacturing process and the first to product applications.” Marks says that it westward, the number of face-to face approved blockbuster indication for a became very apparent with some COVID- meetings declined rapidly; by March, small-interfering RNA (siRNA) — the 19-related files that resolving a single they were replaced by Webex and Teams. European Medicines Agency’s (EMA) issue can help a sponsor enormously and (Secure Zoom meeting are to be added registration of the RNA interference accelerate the development cycle. Before this year.) And remarkably, by 31 December, (RNAi) therapy Leqvio (inclisiran) for COVID-19, it was conceivable that a small the US Food and Drug Administration cardiovascular disease.