Pharmacokinetics and Exposure-Response Relationship of Teprotumumab Frst 3 Months, Unless Determined to Be Medically Necessary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oregon Medicaid Pharmaceutical Services Prior Authorization Criteria
Oregon Medicaid Pharmaceutical Services Prior Authorization Criteria HEALTH SYSTEMS DIVISION Prior authorization (PA) criteria for fee-for-service prescriptions for Oregon Health Plan clients March 1, 2021 Contents Contents ................................................................................................................................................................ 2 Introduction........................................................................................................................................................... 7 About this guide ......................................................................................................................................... 7 How to use this guide ................................................................................................................................. 7 Administrative rules and supplemental information .................................................................................. 7 Update information............................................................................................................................................... 8 Effective March 1, 2021 ............................................................................................................................ 8 Substantive updates and new criteria ............................................................................................. 8 Clerical changes ............................................................................................................................ -

IGF System in Sarcomas: a Crucial Pathway with Many Unknowns to Exploit for Therapy
61 1 Journal of Molecular C Mancarella and Targeting IGF system in sarcoma 61:1 T45–T60 Endocrinology K Scotlandi THEMATIC REVIEW 40 YEARS OF IGF1 IGF system in sarcomas: a crucial pathway with many unknowns to exploit for therapy Caterina Mancarella and Katia Scotlandi Experimental Oncology Lab, CRS Development of Biomolecular Therapies, Orthopaedic Rizzoli Institute, Bologna, Italy Correspondence should be addressed to K Scotlandi: [email protected] This paper forms part of a special section on 40 Years of IGF1. The guest editors for this section were Derek LeRoith and Emily Gallagher. Abstract The insulin-like growth factor (IGF) system has gained substantial interest due to its Key Words involvement in regulating cell proliferation, differentiation and survival during anoikis f sarcomas and after conventional and targeted therapies. However, results from clinical trials have f IGF system been largely disappointing, with only a few but notable exceptions, such as trials targeting f targeted therapy sarcomas, especially Ewing sarcoma. This review highlights key studies focusing on IGF f clinical trials signaling in sarcomas, specifically studies underscoring the properties that make this system an attractive therapeutic target and identifies new relationships that may be exploited. This review discusses the potential roles of IGF2 mRNA-binding proteins (IGF2BPs), discoidin domain receptors (DDRs) and metalloproteinase pregnancy-associated plasma protein-A (PAPP-A) in regulating the IGF system. Deeper investigation of these novel regulators of the IGF system may help us to further elucidate the spatial and temporal control of the IGF Journal of Molecular axis, as understanding the control of this axis is essential for future clinical studies. -

Interim Report for the First Quarter of 2020
Genmab Announces Financial Results for the First Quarter of 2020 May 6, 2020; Copenhagen, Denmark; Interim Report for the First Quarter Ended March 31, 2020 Highlights DARZALEX® (daratumumab) net sales increased approximately 49% compared to the first quarter of 2019 to USD 937 million, resulting in royalty income of DKK 775 million DARZALEX approved in Europe in combination with bortezomib, thalidomide and dexamethasone for the treatment of adult patients with newly diagnosed multiple myeloma who are eligible for autologous stem cell transplant U.S. FDA approved TEPEZZA™ (teprotumumab-trbw), developed and commercialized by Horizon Therapeutics, for thyroid eye disease U.S. FDA accepted, with priority review, Novartis’ supplemental Biologics License Application for subcutaneous ofatumumab in relapsing multiple sclerosis Anthony Pagano appointed Chief Financial Officer Anthony Mancini appointed Chief Operating Officer “Despite the unprecedented challenges posed by the coronavirus (COVID-19) pandemic, we will continue to invest in our innovative proprietary products, technologies and capabilities and use our world-class expertise in antibody drug development to create truly differentiated products with the potential to help cancer patients. While Genmab is closely monitoring the developments in the rapidly evolving landscape, we are extremely fortunate to have a solid financial foundation and a fabulous and committed team to carry us through these uncertain times,” said Jan van de Winkel, Ph.D., Chief Executive Officer of Genmab. Financial Performance First Quarter of 2020 Revenue was DKK 892 million in the first quarter of 2020 compared to DKK 591 million in the first quarter of 2019. The increase of DKK 301 million, or 51%, was mainly driven by higher DARZALEX royalties. -

Therapeutic Targeting of the IGF Axis
cells Review Therapeutic Targeting of the IGF Axis Eliot Osher and Valentine M. Macaulay * Department of Oncology, University of Oxford, Oxford, OX3 7DQ, UK * Correspondence: [email protected]; Tel.: +44-1865617337 Received: 8 July 2019; Accepted: 9 August 2019; Published: 14 August 2019 Abstract: The insulin like growth factor (IGF) axis plays a fundamental role in normal growth and development, and when deregulated makes an important contribution to disease. Here, we review the functions mediated by ligand-induced IGF axis activation, and discuss the evidence for the involvement of IGF signaling in the pathogenesis of cancer, endocrine disorders including acromegaly, diabetes and thyroid eye disease, skin diseases such as acne and psoriasis, and the frailty that accompanies aging. We discuss the use of IGF axis inhibitors, focusing on the different approaches that have been taken to develop effective and tolerable ways to block this important signaling pathway. We outline the advantages and disadvantages of each approach, and discuss progress in evaluating these agents, including factors that contributed to the failure of many of these novel therapeutics in early phase cancer trials. Finally, we summarize grounds for cautious optimism for ongoing and future studies of IGF blockade in cancer and non-malignant disorders including thyroid eye disease and aging. Keywords: IGF; type 1 IGF receptor; IGF-1R; cancer; acromegaly; ophthalmopathy; IGF inhibitor 1. Introduction Insulin like growth factors (IGFs) are small (~7.5 kDa) ligands that play a critical role in many biological processes including proliferation and protection from apoptosis and normal somatic growth and development [1]. IGFs are members of a ligand family that includes insulin, a dipeptide comprised of A and B chains linked via two disulfide bonds, with a third disulfide linkage within the A chain. -

Horizon Therapeutics Secures US FDA Approval For
Horizon Therapeutics Secures U.S. FDA Approval for Teprotumumab, for the Treatment of Thyroid Eye Disease (TED) Media Release Copenhagen, Denmark, January 23, 2020 • Third Genmab-created product approved by the U.S. FDA Genmab A/S (Nasdaq: GMAB) announced today that the U.S. Food and Drug Administration (U.S. FDA) has granted approval to Horizon Therapeutics (Nasdaq: HZNP) for the use of teprotumumab, under the trade name TEPEZZA™ (teprotumumab-trbw), for the treatment of Thyroid Eye Disease (TED). TEPEZZA, the first and only U.S. FDA-approved medicine for the treatment of TED, was developed by and is manufactured by Horizon, completing a long development program that began when Genmab created the molecule nearly two decades ago. Horizon submitted the Biologics License Application for teprotumumab, which received Priority Review, Orphan Drug, Fast Track and Breakthrough Therapy designations from the FDA. Teprotumumab was created by Genmab under a collaboration with Roche and development of the product is now being conducted by Horizon under a license from Roche. Under the terms of Genmab’s agreement with Roche, Genmab will receive mid- single digit royalties on sales of TEPEZZA. “We would like to congratulate Horizon on this exciting approval, and we are very pleased that patients in the United States living with thyroid eye disease, a vision-threatening autoimmune condition, will now have this important new treatment option,” said Jan van de Winkel, Ph.D., Chief Executive Officer of Genmab. “We also believe that this approval, the third for a Genmab-created product following Arzerra® and DARZALEX®, reflects our company’s proven track record in improving the lives of patients by creating breakthrough innovative antibody products.” For more information about TEPEZZA and TED, please see the press release issued by Horizon Therapeutics. -

CDER Breakthrough Therapy Designation Approvals Data As of December 31, 2020 Total of 190 Approvals
CDER Breakthrough Therapy Designation Approvals Data as of December 31, 2020 Total of 190 Approvals Submission Application Type and Proprietary Approval Use Number Number Name Established Name Applicant Date Treatment of patients with previously BLA 125486 ORIGINAL-1 GAZYVA OBINUTUZUMAB GENENTECH INC 01-Nov-2013 untreated chronic lymphocytic leukemia in combination with chlorambucil Treatment of patients with mantle cell NDA 205552 ORIGINAL-1 IMBRUVICA IBRUTINIB PHARMACYCLICS LLC 13-Nov-2013 lymphoma (MCL) Treatment of chronic hepatitis C NDA 204671 ORIGINAL-1 SOVALDI SOFOSBUVIR GILEAD SCIENCES INC 06-Dec-2013 infection Treatment of cystic fibrosis patients age VERTEX PHARMACEUTICALS NDA 203188 SUPPLEMENT-4 KALYDECO IVACAFTOR 21-Feb-2014 6 years and older who have mutations INC in the CFTR gene Treatment of previously untreated NOVARTIS patients with chronic lymphocytic BLA 125326 SUPPLEMENT-60 ARZERRA OFATUMUMAB PHARMACEUTICALS 17-Apr-2014 leukemia (CLL) for whom fludarabine- CORPORATION based therapy is considered inappropriate Treatment of patients with anaplastic NOVARTIS lymphoma kinase (ALK)-positive NDA 205755 ORIGINAL-1 ZYKADIA CERITINIB 29-Apr-2014 PHARMACEUTICALS CORP metastatic non-small cell lung cancer (NSCLC) who have progressed on or are intolerant to crizotinib Treatment of relapsed chronic lymphocytic leukemia (CLL), in combination with rituximab, in patients NDA 206545 ORIGINAL-1 ZYDELIG IDELALISIB GILEAD SCIENCES INC 23-Jul-2014 for whom rituximab alone would be considered appropriate therapy due to other co-morbidities -

Insulin-Like Growth Factor Pathway and the Thyroid
REVIEW published: 04 June 2021 doi: 10.3389/fendo.2021.653627 Insulin-Like Growth Factor Pathway and the Thyroid Terry J. Smith* Department of Ophthalmology and Visual Sciences, Kellogg Eye Center, Division of Metabolism, Endocrinology, and Diabetes, Department of Internal Medicine, University of Michigan Medical School, Ann Arbor, MI, United States The insulin-like growth factor (IGF) pathway comprises two activating ligands (IGF-I and IGF-II), two cell-surface receptors (IGF-IR and IGF-IIR), six IGF binding proteins (IGFBP) and nine IGFBP related proteins. IGF-I and the IGF-IR share substantial structural and functional similarities to those of insulin and its receptor. IGF-I plays important regulatory roles in the development, growth, and function of many human tissues. Its pathway intersects with those mediating the actions of many cytokines, growth factors and hormones. Among these, IGFs impact the thyroid and the hormones that it generates. Further, thyroid hormones and thyrotropin (TSH) can influence the biological effects of growth hormone and IGF-I on target tissues. The consequences of this two-way interplay can be far-reaching on many metabolic and immunologic processes. Specifically, IGF-I supports normal function, volume and hormone synthesis of the thyroid gland. Some of these effects are mediated through enhancement of sensitivity to the actions of TSH while Edited by: others may be independent of pituitary function. IGF-I also participates in pathological Jeff M. P. Holly, conditions of the thyroid, including benign enlargement and tumorigenesis, such as those University of Bristol, United Kingdom ’ Reviewed by: occurring in acromegaly. With regard to Graves disease (GD) and the periocular process Leonard Girnita, frequently associated with it, namely thyroid-associated ophthalmopathy (TAO), IGF-IR Karolinska Institutet (KI), Sweden has been found overexpressed in orbital connective tissues, T and B cells in GD and TAO. -

FDA Briefing Document Dermatologic and Ophthalmic Drugs Advisory
FDA Briefing Document Dermatologic and Ophthalmic Drugs Advisory Committee Meeting December 13, 2019 The committee will discuss biologics license application (BLA) 761143, teprotumumab solution for intravenous use, submitted by Horizon Pharma Ireland, Ltd., proposed for the treatment of active Thyroid Eye Disease (TED). FDA Advisory Committee Briefing Material for BLA 761143 (b) (4) (teprotumumab- (b) (4) The attached package contains background information prepared by the Food and Drug Administration (FDA) for the panel members of the advisory committee. The FDA background package often contains assessments and/or conclusions and recommendations written by individual FDA reviewers. Such conclusions and recommendations do not necessarily represent the final position of the individual reviewers, nor do they necessarily represent the final position of the Review Division or Office. We have brought the biologics license application (BLA) 761143, teprotumumab solution for intravenous use, submitted by Horizon Pharma Ireland, Ltd. and proposed for the treatment of active Thyroid Eye Disease (TED) to this Advisory Committee in order to gain the Committee’s insights and opinions, and the background package may not include all issues relevant to the final regulatory recommendation and instead is intended to focus on issues identified by the Agency for discussion by the advisory committee. The FDA will not issue a final determination on the issues at hand until input from the advisory committee process has been considered and all reviews have been finalized. The final determination may be affected by issues not discussed at the advisory committee meeting. 2 FDA Advisory Committee Briefing Material for BLA 761143 (b) (4) (teprotumumab- (b) (4) Table of Contents 1. -
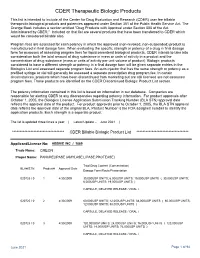
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

Medical Drug Benefit Clinical Criteria Updates
Medicaid Managed Care Provider Bulletin April 2021 Medical drug benefit Clinical Criteria updates On August 16, 2019, November 15, 2019, December 18, 2019, February 21, 2020, March 26, 2020, May 15, 2020, June 18, 2020, August 21, 2020, September 24, 2020, and November 20, 2020, the Pharmacy and Therapeutics (P&T) Committee approved the following Clinical Criteria applicable to the medical drug benefit for Healthy Blue. These policies were developed, revised or reviewed to support clinical coding edits. Visit Clinical Criteria to search for specific policies. If you have questions or would like additional information, use this email. Please see the explanation/definition for each category of Clinical Criteria below: • New: newly published criteria • Revised: addition or removal of medical necessity requirements, new document number • Updates marked with an asterisk (*): criteria may be perceived as more restrictive Please note: The Clinical Criteria listed below applies only to the medical drug benefits contained within the member’s medical policy. This does not apply to pharmacy services. Effective date Document number Clinical Criteria title New or revised 06/07/2021 ING-CC-0154* Givlaari (givosiran) New 06/07/2021 ING-CC-0155* Ethyol (amifostine) New 06/07/2021 ING-CC-0156* Reblozyl (luspatercept) New 06/07/2021 ING-CC-0157* Padcev (enfortumab vedotin) New 06/07/2021 ING-CC-0158* Enhertu (fam-trastuzumab deruxtecan-nxki) New 06/07/2021 ING-CC-0159* Scenesse (afamelanotide) New 06/07/2021 ING-CC-0161* Sarclisa (isatuximab-irfc) New -

Trastuzumab (Anti-Idiotype) Alexa Fluor® 750-Conjugated Antibody
Anti- Trastuzumab (Anti-Idiotype) Alexa Fluor® 750-conjugated Antibody Recombinant Monoclonal Rabbit IgG Clone # 2261E Catalog Number: FAB95471S 100 µg DESCRIPTION Specificity Detects Trastuzumab in Western blots and direct ELISAs. In direct ELISAs, no crossreactivity with Cetuximab, Ibritumomab, Rituximab, Adalimumab, Tositumomab, Brentuximab, Gemtuzumab, Solanezumab, Teprotumumab, and Aducanumab is observed. Source Recombinant Monoclonal Rabbit IgG Clone # 2261E Purification Protein A or G purified from cell culture supernatant Immunogen Fulllength Trastuzumab Conjugate Alexa Fluor 750 Excitation Wavelength: 749 nm Emission Wavelength: 775 nm Formulation Supplied 0.2 mg/mL in a saline solution containing BSA and Sodium Azide See Certificate of Analysis for details. *Contains <0.1% Sodium Azide, which is not hazardous at this concentration according to GHS classifications. Refer to the Safety Data Sheet (SDS) for additional information and handling instructions. APPLICATIONS Please Note: Optimal dilutions should be determined by each laboratory for each application. General Protocols are available in the Technical Information section on our website. Recommended Sample Concentration Flow Cytometry 0.251 µg/106 cells MCF7 Human Cell Line stained with Trastuzumab (AntiErbB2/Her2) PREPARATION AND STORAGE Shipping The product is shipped with polar packs. Upon receipt, store it immediately at the temperature recommended below. Stability & Storage Protect from light. Do not freeze. l 12 months from date of receipt, 2 to 8 °C as supplied. BACKGROUND The antiTrastuzumab antibody is an antiIdiotype antibody raised against and selected for the antigenic determinants of the variable region of Trastuzumab. The antibody has been tested against a broad range of other biosimilars to ensure specificity. -

Journal of Managed Care & Specialty Pharmacy®
J MC P ■ Journal of Mana of Journal JOURNAL OF g ANAGED ed Care & Specialty Pharmac M CARE & SPECIALTY PHARMACY® y ■ October 2020 Supplement ■ Volume 26 ■ Number 10-a ■ October 2020 ■ Supplemen t ■ Vol. 26, No. 10-a Making the Way for Innovation 2020 VIRTUAL • WEEK OF OCT. 19 Poster Abstracts Journal of Managed Care & Specialty Pharmacy® Previously published as JMCP, the Journal of Managed Care Pharmacy® A Peer-Reviewed Journal of the AMCP ■ www.jmcp.org ■ www.amcp.org AMCP Abstracts Program The AMCP NEXUS 2020 VIRTUAL will be held online the week of October 19, 2020. The AMCP abstracts program provides a forum through which authors can share their insights and outcomes of advanced managed care practice. For NEXUS 2020 VIRTUAL, abstract posters are scheduled to be presented Wednesday, October 21, from 1:00 pm EDT to 2:30 pm EDT. At that time, poster presenters will be available for live chats and will also share additional information about their research at https://plan.core-apps.com/ ■ Publisher amcp2020. Professional abstracts that have been reviewed are published in the Journal of Managed Susan A. Cantrell, RPh, CAE Care & Specialty Pharmacy’s (JMCP) Poster Abstracts supplement. Chief Executive Officer Academy of Managed Care Pharmacy Abstract Review Process ■ Editor-in-Chief Sixty-seven reviewers and 4 JMCP editorial reviewers were involved in the abstract review process Laura E. Happe, PharmD, MPH for AMCP NEXUS 2020 VIRTUAL. Each abstract (with author name and affiliation blinded) was 727.488.2700 reviewed and scored using a 1-5 scale with the following 5 criteria (15 rating scores per abstract), [email protected] which are used by JMCP to evaluate manuscripts for publication: ■ Assistant Editors • Relevance • Originality • Quality • Bias • Clarity Donald G.