Nutrient Profile Model for Sri Lanka
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

YAMU.LK PP- YAMU Range Ad Oct 15 FINAL.Pdf 1 10/15/15 2:55 PM
FREE The Sushi Bento at Naniyori MARCH/2016 WWW.YAMU.LK PP- YAMU Range Ad Oct 15 FINAL.pdf 1 10/15/15 2:55 PM C M Y CM MY CY CMY K PP- YAMU Range Ad Oct 15 FINAL.pdf 1 10/15/15 2:55 PM C M Y CM MY CY CMY K 4 [insert title here] - this is the actual title We’ve got some great stuff in this issue. We did our first EDITORIAL ever quiz, where you can gauge your competency as a Indi Samarajiva Colombar. If you feel inadequate after that, we’ve hooked Bhagya Goonewardhane you up with a guide to 24 hours in Colombo to impress Aisha Nazim Imaad Majeed your visiting friends! Shifani Reffai Kinita Shenoy We’ve also done lots of chill travels around the island, from Batti to Koggala Lake to Little Adam’s Peak. There’s ADVERTISING going to be plenty more coming up as we go exploring Dinesh Hirdaramani during the April holidays, so check the site yamu.lk for 779 776 445 / [email protected] more. CONTACT 11 454 4230 (9 AM - 5 PM) With the Ides of March around the corner, just remember [email protected] that any salad is a Caesar Salad if you stab it enough. PRINTED BY Imashi Printers ©2015 YAMU (Pvt) Ltd 14/15A Duplication Road, Col 4 kinita KIITO WE DO SUITS Damith E. Cooray CText ATI Head Cutter BSc (Hons) International Clothing Technology & Design Manchester Metropolitan University, UK Sole Distributor of Flagship Store KIITO Bespoke & Workshop # 19 , First Floor, Auditor General’s Department Building # 27, Rosmead Place Arcade Independance Square Colombo 07 Colombo 07 0112 690740 0112 675670 8 SCARLET ROOM 32, Alfred House Avenue, Colombo 03 | 11 4645333 BY BHAGYA their dishes with the exception Risotto Paella (Rs. -

Cultural Diary’ Brings You Details About Avurudu Celebrations and Sev- Celebration at the Governors Ter- Eral Other Fascinating Events Happening in the Country
>> Avurudu Ê Ruwanthi Abeyakoon As the sun moves from Meena Rashi to Mesha Rashi completing a cycle of a celebrations twelve-month period, the season of kiribath (milk rice), kevum and kokis begins. Experience a traditional Avurudu Today’s ‘Cultural Diary’ brings you details about Avurudu celebrations and sev- celebration at the Governors Ter- eral other fascinating events happening in the country. Take your pick of stage race, Mount Lavinia Hotel. You can plays, exhibitions, or dance performance and add colour to your routine life. You witness and take part in the old can make merry and enjoy the adventures or sit back, relax and enjoy a movie of April traditions and enjoy the dawn of your choice. Make a little space to kick into high gear amidst the busy work the New Year. Events that will take schedules to enjoy the exciting events happening at venues around the city. If >> Non-Aligned place are Lipa gini melaweema 11 April there is an event you would like others to know, drop an email to eventcalen- (Lighting of the hearth-fire place) [email protected] or call us on 011 2429652. Have a pleasant week. Boiling of milk in a newly earthen - an exhibition pot 15 Aahara anubhawaya Ganu denu with a difference Weda alleema Raban gaseema @ Barefoot Gallery Cultural show and dancing Artists Mariah Lookman and Shanaathanan envision Pancha keliya Non Aligned as a group show of works by Vaidehi Raja, Olindha keliya Thamotharampillai Shanaathanan, Muhanned Cader, Onchili warang Mariah Lookman, Lala Rukh and Ieuan Weinman. The exhibition will be held at Barefoot Gallery Colombo, 704, Galle Road Colombo 3 until April 17. -

Rs.600 Million
NO E-PAPER FROM RICE MILLS DECLARED APRIL 13 TO 15 The Daily News E-Paper will not be published from Monday, April 13 to Wednesday, April 15 in view of the Sinhala and Tamil New Year. Publication will resume from Thursday, April 16. The online edition of the Daily News will be updated as usual during this period at www.dailynews.lk. AN essenTIAL SERVICE RICE MILLS HAVE TO BE KEPT OPEN THREE MILLION MT OF PADDY HARVesTED STERN ACTION AGAINST PRICE GOUGING AMALI MALLAWARACHCHI to distribute in the entire country.A Services of all rice mills have been harvest of around three million metric Rs.600 million declared an essential service under the tons of paddy has been reaped by now COVID–19 quarantine process since and the quantity of rice that can be the provision of essential foods and rice produced is equivalent to 2/3 of that production, storage and distribution is amount. MAXIMUM RETAIL allocated for imperative to ensure food security, the Accordingly, all the relevant par- President’s Office said. ties have been told that increasing the Rice mill owners must produce rice rice prices or hampering the supply of in their respective areas using paddy rice pose a major impediment to the purchasing fish stocks in their possession. Under the effective implementation of quarantine PRICes FOR RICE instructions of the President, the Secre- activities. The Consumer Affairs Authority yesterday CHAMINDA PERERA tary to the President P. B. Jayasundara Accordingly, the President’s Secre- announced maximum retail prices (MRP) on rice in a letter had informed the Acting tary has instructed relevant parties to with effect from April 10, 2020. -
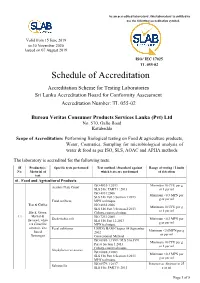
Schedule of Accreditation
As an accredited laboratory, this laboratory is entitled to use the following accreditation symbol. Valid from 15 June 2019 to 30 November 2020 Issued on 07 August 2019 ISO/ IEC 17025 TL 055-02 Schedule of Accreditation Accreditation Scheme for Testing Laboratories Sri Lanka Accreditation Board for Conformity Assessment Accreditation Number: TL 055-02 Bureau Veritas Consumer Products Services Lanka (Pvt) Ltd No. 570, Galle Road Katubedda Scope of Accreditation: Performing Biological testing on Food & agriculture products, Water, Cosmetics, Sampling for microbiological analysis of water & food as per ISO, SLS, AOAC and APHA methods The laboratory is accredited for the following tests. SI Product(s) / Specific tests performed Test method / Standard against Range of testing / Limits No. Material of which tests are performed of detection test 01. Food and Agricultural Products ISO 4833-1:2013 Minimum 10 CFU per g Aerobic Plate Count SLS 516: PART 1: 2013 or 1 per ml ISO 4831:2006 Minimum <0.3 MPN per SLS 516 Part 3 Section 1:2013 g or per ml Total coliform MPN technique Tea & Coffee ISO 4832:2006 Minimum 10 CFU per g SLS 516 Part 3 Section 2:2013 or 1 per ml Black, Green, Colony-count technique 1.1 Herbal & ISO 7251:2005 Escherichia coli Minimum <0.3 MPN per flavored, white SLS 516 Part 12:2013 g or per ml tea Camellia MPN technique sinensis, Tea Fecal coliforms USFDA BAM Chapter 04 September Minimum <3.0MPN per g based 2002 or per ml Beverages Conventional Method ISO 6888-1:1999 / SLS 516:1991 Minimum 10 CFU per g Part 6 Section 1:2013 or 1 per ml Colony-count technique Staphylococcus aureus ISO 6888-3:2003 Minimum <0.3 MPN per SLS 516 Part 6 Section 3:2013 g or per ml MPN technique ISO 6579-1:2017 Presence or Absence in 25 Salmonella SLS 516: PART 5: 2013 g or ml Page 1 of 8 SI Product(s) / Specific tests performed Test method / Standard against Range of testing / Limits No. -

14 Baski.Pdf
NEWS • HABER BBM DERGİSİ July-September • Temmuz - Eylül 2015 1 NEWS • HABER 2 July-September • Temmuz - Eylül 2015 BBM MAGAZINE NEWS • HABER BBM DERGİSİ July-September • Temmuz - Eylül 2015 3 EDITOR EDİTÖR The next IDMA is in 2018 Bir sonraki İDMA, 2018’de Dear Readers, Değerli okurlar, We, as Parantez Fair Organization, have managed to carry Parantez Fuarcılık olarak geride bıraktığımız 10 yıllık süreçte, İDMA IDMA Exhibition a step further in the last 10 years. As a fair orga- Fuarı’nı hep bir basamak yukarı taşımayı başardık. Bir fuar şirketi nization company, our biggest dream for IDMA was to carrying it olarak en büyük hayalimiz, bir gün İDMA’nın uluslararası alanda to an international fair level to be known and followed internation- tanınan ve takip edilen bir fuar düzeyine ulaşmasıydı. Nihayetinde ally. I believe that we managed this eventually. I think IDMA 2013 de bunu başardığımıza inanıyorum. Özellikle İDMA 2013’ün bu an- was a serious breaking point in that sense. IDMA 2015 has also lamda ciddi bir kırılma noktası olduğunu düşünüyorum, İDMA 2015 proved this one more time in spite of general improper conditions ise dünya genelindeki olumsuz tabloya rağmen bunu bir kez daha in the world. onaylayan fuar oldu. Of course, the success gained so far was not a coinci- Elbette bugüne kadar ki başarı, kesinlikle bir tesadüf değildi… Bu dence… This success was a gaining obtained by a vision of başarı, belli bir alanda uzmanlaşma vizyonumuzun, yani bir fuar şirketi specializing in a specific area, in other words, leaving all the olarak diğer tüm sektörle olan çalışmalarımızı geride bırakıp sadece other businesses behind and focusing on only one industry. -

The Gujarati Lyrics of Kavi Dayarambhal
The Gujarati Lyrics of Kavi Dayarambhal Rachel Madeline Jackson Dwyer School of Oriental and African Studies Thesis presented to the University of London for the degree PhD July 1995 /f h. \ ProQuest Number: 10673087 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 10673087 Published by ProQuest LLC(2017). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 ABSTRACT Kavi Dayarambhal or Dayaram (1777-1852), considered to be one of the three greatest poets of Gujarati, brought to an end not only the age of the great bhakta- poets, but also the age of Gujarati medieval literature. After Dayaram, a new age of Gujarati literature and language began, influenced by Western education and thinking. The three chapters of Part I of the thesis look at the ways of approaching North Indian devotional literature which have informed all subsequent readings of Dayaram in the hundred and fifty years since his death. Chapter 1 is concerned with the treatment by Indologists of the Krsnaite literature in Braj Bhasa, which forms a significant part of Dayaram's literary antecedents. -

Sweetening the Deal Tapping Into a Sweet Sri Lankan Secret by Vidya Balachander
Navigate | LOCAL FLAVOUR Sweetening the Deal Tapping inTo a sweeT sri Lankan secreT BY VIDYA BALACHANDER considered Sri Lanka’s answer to maple The fishtail palm’s syrup. It tastes flowery, like single inflorescence is flora honey, yet not as cloying, and tapped for its sugary sap which with an undertone of warm spice like makes a sticky that of mulled wine. The secret of its treacle as well as unique flavour rests in the fact that it is solid jaggery; A produced from the sap collected from jar of fresh kithul treacle (bottom). its flowers. Like other palm products from the subcontinent, the supply of kithul treacle hinges on the dexterity of skilled tappers, who climb trees that can grow over 20 feet high. Armed with traditional wisdom about when the trees bloom (only once in their life) and form sap, tappers make a cut at the base of the stalk bearing clusters of flowers. A pot is tied to the tree to collect the precious sap, which is then thickened and purified over a wood fire before being bottled. Like the Bengali winter favourite nolen gur, a toffee-like liquid jaggery extracted from the wild date palm, Sri Lankan kithul is also a much- loved local delicacy. A complex and flavourful substitute for sugar, kithul is a quintessential part of Sri Lankan sweets such as pani walalu, a squiggly, jalebi- like sweet made of urad dal and rice which is dunked in treacle, and konda kevum, a spongy, deep-fried cake like the South Indian appe or paniyaram, flavoured with treacle instead of sugar. -
Intangible Cultural Heritage Safeguarding Efforts in Sri Lanka
Field Survey Report Intangible Cultural Heritage Safeguarding Efforts in the Asia-Pacific 2011 International Information and Networking Centre for Intangible Cultural Heritage in the Asia-Pacific Region under the auspices of UNESCO In collaboration with National Library and Documentation Services Board, Sri Lanka Preface The International Information and Networking Centre for Intangible Cultural Heritage in the Asia-Pacific Region proposed by the Korean government was finally approved as a category 2 centre under the auspices of UNESCO at the 35th session of the UNESCO General Conference last October. Over the course of the next year, the Centre and the Korean government prepared for the establishment of the UNESCO category 2 centre which is intended to become a hub for the safeguarding of intangible cultural heritage in Asia and the Pacific region. As a well intentioned objective for the future activities of this centre, ICHCAP initiated the 2009 Field Survey Project of the Intangible Cultural Heritage Safeguarding Efforts in the Asia-Pacific Region. In 2011 ICHCAP worked in collaboration with institutions from seven countries which include: Cook Islands, Kyrgyzstan, Lao People’s Democratic Republic, Marshall Islands, Pakistan, Sri Lanka, and Tonga to carry out the field surveys. The purpose of the field survey project was to obtain a grasp on the current situation of ICH safeguarding, along with specific details on each country’s efforts in inventory making and relevant policies, laws, organisations, etc. The centre will continue this project over the next several years to cover all of the countries within the Asia-Pacific region. The centre will serve Asia-Pacific Member States as an information and networking centre for the safeguarding of ICH. -
“Focus on Our Core Strength
ISSN 1833-1831 Tel: 08 8672 5920 http://cooberpedyregionaltimes.wordpress.com Thursday 4 June 2015 “FOCUS ON OUR CORE STRENGTH - OPAL AND TOURISM” SAYS MAYOR The 2015 Far North SA Economic Forum took place in the Conference Room of Desert Cave Hotel on Tuesday 26th May. Mayor Stephen Staines opened the event with an authoritative speech that drew attention to the continuing importance of the opal industry for Coober Pedy. He talked about Far North SA and the State of South Australia “riding the wave of optimism” that large scale mineral mining had brought to the region but now, Coober Pedy had to “get back to basics and focus on our fundamental strengths, opal and tourism.” The Mayor spoke of the opal industry’s strengths such as: - In 1985, opal was adopted as the Gemstone Emblem of South Australia; - In 1995, opal took the mantle as the National Gemstone of Australia; - Australia continues to supply a staggering 95 per cent of the world’s natural gem quality opals; - The highest quality precious opal ranks with diamonds, emeralds, rubies and sapphires as the world’s top five most valuable gemstones; - The state's three major opal fields - Coober Pedy, Mintabie, and Andamooka – are all located in Far North South Australia – and the opal from these fields continues to supply an estimated 80% of total world production. Yanni and Christo Pantelis gave a presentation on the transformation of the former Ampol Roadhouse, now Shell His speech implied that, despite our advantages over other opal producing countries, Australia does not capitalise on “Opal mining is an intriguing part of the mining sector Once again, the local businesses at the event were by far our strengths very well. -

ENGLISH Grade 4
ENGLISH Grade 4 Educational Publications Department First Print - 2018 Second Print - 2019 All Rights Reserved ISBN 978-955-25-0057-2 Published by Educational Publications Department Printed by Sanvin (Pvt) Ltd. No. 35/3, Keragala Road, Halummahara, Delgoda. ii The National Anthem of Sri Lanka Sri Lanka Matha Apa Sri Lanka Namo Namo Namo Namo Matha Sundara siri barinee, surendi athi sobamana Lanka Dhanya dhanaya neka mal palaturu piri jaya bhoomiya ramya Apa hata sepa siri setha sadana jeewanaye matha Piliganu mena apa bhakthi pooja Namo Namo Matha Apa Sri Lanka Namo Namo Namo Namo Matha Oba we apa vidya Obamaya apa sathya Oba we apa shakthi Apa hada thula bhakthi Oba apa aloke Apage anuprane Oba apa jeevana we Apa mukthiya oba we Nava jeevana demine, nithina apa pubudukaran matha Gnana veerya vadawamina regena yanu mana jaya bhoomi kara Eka mavakage daru kela bevina Yamu yamu vee nopama Prema vada sema bheda durerada Namo, Namo Matha Apa Sri Lanka Namo Namo Namo Namo Matha iii wms fjuq tl ujlf. orefjda tl ksjfiys fjfikd tl mdge;s tl reêrh fõ wm lh ;=< ÿjkd tneúks wms fjuq fidhqre fidhqßfhda tl f,i tys jefvkd cSj;a jk wm fuu ksjfia fid|sk isáh hq;= fõ ieug u fuka lreKd .=fKkS fj<S iu.s oñkS rka ñKs uq;= fkdj th uh iem;d lsis l, fkdu Èrkd - wdkkao iurfldaka - xU jha; kf;fs; ehkhNthk; xd;Nw ehk; thOk; ,y;yk; ed;Nw clypy; XLk; xd;Nw ek; FUjp epwk; mjdhy; rNfhjuH ehkhNthk; xd;wha; thOk; tsUk; ehk; ed;wha; ,t; ,y;ypdpNy eyNk tho;jy; Ntz;Lkd;Nwh ahtUk; md;G fUizAld; xw;Wik rpwf;f tho;e;jpLjy; nghd;Dk; kzpAk; Kj;Jky;y. -
Traditional Food & Beverages of Sri Lanka
Traditional Food & Beverages of Sri Lanka ll living beings live by food. The staple food of the Sri Lankan Prof. A. Nimal F. Perera ("Sabbesaththa aharatthika") is rice. Rice is obtained from the AIn. other words, food is paddy plant. Paddy was also known A. Nimhani K. Perera as "salee* in the past. Paddy essential for our existence. Wayamba University of included two broad categories; "Maa Moreover, the great sages of ancient Sri Lanka, Kutiyapitiya times [Hrishis) have declared that wee" and "EI wee". Various our disposition and qualities evidence points out that there had depend on the food that we take. been more than 1500 traditional Prof. E.R. Kalyani Perera Further, there are three categories paddy varieties. The rice prepared University of Peradeniya, of persons according to their food from these different paddy varieties Peradentya. preferences; the righteous and was diverse in taste, aroma and gentle " Sathvikas" prefer soft and their nutritional values. In addition delicious food, rough, nonchalant to rice, other grains containing sweetmeats, fish and meat. Curries and indulgent "Rajasikas" prefer carbohydrates, such as millet, ("maalu") were complementary for acidic, hot and spiced food, and the paspahun scrobicultatum ("amtf), com, lazy, less enthusiastic and less maize, barley, and eleusine coraoana the rice and hence it was known as intelligent "Thamasikas", savor ("kurakkan') were also used widely. "boJhmaaht (rice and curries). In the unclean and stale food. Green gram, cow pea, long beans, consumption of rice and curries, masurg, lentil, koJJu, and gingili were drinking of water ["bath pert) was Food and beverages and their essential capsular ["shimbf) grains also essential. -

Avurudu at the Galadari
2 Tuesday 12th April, 2011 henever there is a local ly get into this prestigious beauty contest, people contest! Wkeep popping the ques- Being a professional tion, "Where have all our beau- dancer, she was selected to ties gone?" The probable answer perform at a cultural show, would be 'abroad.' called Asia Explore, held in LA There are quite a few good last August (2010). lookers from Sri Lanka, now Just after her performance, domiciled in other parts of the she was approached backstage world. And some of them do by the organizers of Miss & Ms he Galle Face Hotel (estab- give their land of birth a big Asia USA. lished in 1864) has been boost by participating in inter- "The very next day, I received Tawarded one of the four national beauty pageants. an official invitation to attend Morina Dass is from Sri the Pageant Interview. And I Pacific Asia Travel Association Lanka, now residing in passed!' Grand Awards in the Heritage California. She works at the This annual event is the pre- Category for 2011. Bank of America, Los Angeles, miere cultural pageant in the An international panel of judges as a bankruptcy specialist. States, open to Asian women picked the winners from among 122 Right now, she is in the spot- living in that part of the world. light as she has been selected as This year, over 45 contestants entries from 102 organizations Ms Sri Lanka for Miss & Ms will be representing the majori- worldwide. Asia USA 2011. ty of the countries in the Asian The Galle Face Hotel was one of "I'm really excited and I'm continent.