Thesis Title: Characteristics of Scapulothoracic Kinematics in A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Elbow Checklist
Workbook Musculoskeletal Ultrasound September 26, 2013 Shoulder Checklist Long biceps tendon Patient position: Facing the examiner Shoulder in slight medial rotation; elbow in flexion and supination Plane/ region: Transverse (axial): from a) intraarticular portion to b) myotendinous junction (at level of the pectoralis major tendon). What you will see: Long head of the biceps tendon Supraspinatus tendon Transverse humeral ligament Subscapularis tendon Lesser tuberosity Greater tuberosity Short head of the biceps Long head of the biceps (musculotendinous junction) Humeral shaft Pectoralis major tendon Plane/ region: Logitudinal (sagittal): What you will see: Long head of biceps; fibrillar structure Lesser tuberosity Long head of the biceps tendon Notes: Subscapularis muscle and tendon Patient position: Facing the examiner Shoulder in lateral rotation; elbow in flexion/ supination Plane/ region: longitudinal (axial): full vertical width of tendon. What you will see: Subscapularis muscle, tendon, and insertion Supraspinatus tendon Coracoid process Deltoid Greater tuberosity Lesser tuberosity Notes: Do passive medial/ lateral rotation while examining Plane/ region: Transverse (sagittal): What you will see: Lesser tuberosity Fascicles of subscapularis tendon Supraspinatus tendon Patient position: Lateral to examiner Shoulder in extension and medial rotation Hand on ipsilateral buttock Plane/ region: Longitudinal (oblique sagittal) Identify the intra-articular portion of biceps LH in the transverse plane; then -

Structure of the Human Body
STRUCTURE OF THE HUMAN BODY Vertebral Levels 2011 - 2012 Landmarks and internal structures found at various vertebral levels. Vertebral Landmark Internal Significance Level • Bifurcation of common carotid artery. C3 Hyoid bone Superior border of thyroid C4 cartilage • Larynx ends; trachea begins • Pharynx ends; esophagus begins • Inferior thyroid A crosses posterior to carotid sheath. • Middle cervical sympathetic ganglion C6 Cricoid cartilage behind inf. thyroid a. • Inferior laryngeal nerve enters the larynx. • Vertebral a. enters the transverse. Foramen of C 6. • Thoracic duct reaches its greatest height C7 Vertebra prominens • Isthmus of thyroid gland Sternoclavicular joint (it is a • Highest point of apex of lung. T1 finger's breadth below the bismuth of the thyroid gland T1-2 Superior angle of the scapula T2 Jugular notch T3 Base of spine of scapula • Division between superior and inferior mediastinum • Ascending aorta ends T4 Sternal angle (of Louis) • Arch of aorta begins & ends. • Trachea ends; primary bronchi begin • Heart T5-9 Body of sternum T7 Inferior angle of scapula • Inferior vena cava passes through T8 diaphragm T9 Xiphisternal junction • Costal slips of diaphragm T9-L3 Costal margin • Esophagus through diaphragm T10 • Aorta through diaphragm • Thoracic duct through diaphragm T12 • Azygos V. through diaphragm • Pyloris of stomach immediately above and to the right of the midline. • Duodenojejunal flexure to the left of midline and immediately below it Tran pyloric plane: Found at the • Pancreas on a line with it L1 midpoint between the jugular • Origin of Superior Mesenteric artery notch and the pubic symphysis • Hilum of kidneys: left is above and right is below. • Celiac a. -

Parts of the Body 1) Head – Caput, Capitus 2) Skull- Cranium Cephalic- Toward the Skull Caudal- Toward the Tail Rostral- Toward the Nose 3) Collum (Pl
BIO 3330 Advanced Human Cadaver Anatomy Instructor: Dr. Jeff Simpson Department of Biology Metropolitan State College of Denver 1 PARTS OF THE BODY 1) HEAD – CAPUT, CAPITUS 2) SKULL- CRANIUM CEPHALIC- TOWARD THE SKULL CAUDAL- TOWARD THE TAIL ROSTRAL- TOWARD THE NOSE 3) COLLUM (PL. COLLI), CERVIX 4) TRUNK- THORAX, CHEST 5) ABDOMEN- AREA BETWEEN THE DIAPHRAGM AND THE HIP BONES 6) PELVIS- AREA BETWEEN OS COXAS EXTREMITIES -UPPER 1) SHOULDER GIRDLE - SCAPULA, CLAVICLE 2) BRACHIUM - ARM 3) ANTEBRACHIUM -FOREARM 4) CUBITAL FOSSA 6) METACARPALS 7) PHALANGES 2 Lower Extremities Pelvis Os Coxae (2) Inominant Bones Sacrum Coccyx Terms of Position and Direction Anatomical Position Body Erect, head, eyes and toes facing forward. Limbs at side, palms facing forward Anterior-ventral Posterior-dorsal Superficial Deep Internal/external Vertical & horizontal- refer to the body in the standing position Lateral/ medial Superior/inferior Ipsilateral Contralateral Planes of the Body Median-cuts the body into left and right halves Sagittal- parallel to median Frontal (Coronal)- divides the body into front and back halves 3 Horizontal(transverse)- cuts the body into upper and lower portions Positions of the Body Proximal Distal Limbs Radial Ulnar Tibial Fibular Foot Dorsum Plantar Hallicus HAND Dorsum- back of hand Palmar (volar)- palm side Pollicus Index finger Middle finger Ring finger Pinky finger TERMS OF MOVEMENT 1) FLEXION: DECREASE ANGLE BETWEEN TWO BONES OF A JOINT 2) EXTENSION: INCREASE ANGLE BETWEEN TWO BONES OF A JOINT 3) ADDUCTION: TOWARDS MIDLINE -
Shoulder Shoulder
SHOULDER SHOULDER ⦿ Connects arm to thorax ⦿ 3 joints ◼ Glenohumeral joint ◼ Acromioclavicular joint ◼ Sternoclavicular joint ⦿ https://www.youtube.com/watch?v=rRIz6oO A0Vs ⦿ Functional Areas ◼ scapulothoracic ◼ scapulohumeral SHOULDER MOVEMENTS ⦿ Global Shoulder ⦿ Arm (Shoulder Movement Joint) ◼ Elevation ◼ Flexion ◼ Depression ◼ Extension ◼ Abduction ◼ Abduction ◼ Adduction ◼ Adduction ◼ Medial Rotation ◼ Medial Rotation ◼ Lateral Rotation ◼ Lateral Rotation SHOULDER MOVEMENTS ⦿ Movement of shoulder can affect spine and rib cage ◼ Flexion of arm Extension of spine ◼ Extension of arm Flexion of spine ◼ Adduction of arm Ipsilateral sidebending of spine ◼ Abduction of arm Contralateral sidebending of spine ◼ Medial rotation of arm Rotation of spine ◼ Lateral rotation of arm Rotation of spine SHOULDER GIRDLE ⦿ Scapulae ⦿ Clavicles ⦿ Sternum ⦿ Provides mobile base for movement of arms CLAVICLE ⦿ Collarbone ⦿ Elongated S shaped bone ⦿ Articulates with Sternum through Manubrium ⦿ Articulates with Scapula through Acromion STERNOCLAVICULAR JOINT STERNOCLAVICULAR JOINT ⦿ Saddle Joint ◼ Between Manubrium and Clavicle ⦿ Movement ◼ Flexion - move forward ◼ Extension - move backward ◼ Elevation - move upward ◼ Depression - move downward ◼ Rotation ⦿ Usually movement happens with scapula Scapula Scapula ● Flat triangular bone ● 3 borders ○ Superior, Medial, Lateral ● 3 angles ○ Superior, Inferior, Lateral ● Processes and Spine ○ Acromion Process, Coracoid Process, Spine of Scapula ● Fossa ○ Supraspinous, Infraspinous, Subscapularis, Glenoid SCAPULA -

Shoulder Anatomy
ShoulderShoulder AnatomyAnatomy www.fisiokinesiterapia.biz ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy ClavicleClavicle – Sternal end – Acromion end ScapulaScapula Acromion – Surfaces end Sternal Costal end Dorsal – Borders – Angles ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy Scapula 1. spine 2. acromion 3. superior border 4. supraspinous fossa 5. infraspinous fossa 6. medial (vertebral) border 7. lateral (axillary) border 8. inferior angle 9. superior angle 10. glenoid fossa (lateral angle) 11. coracoid process 12. superior scapular notch 13 subscapular fossa 14. supraglenoid tubercle 15. infraglenoid tubercle ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy HumerousHumerous – head – anatomical neck – greater tubercle – lesser tubercle – greater tubercle – lesser tubercle – intertubercular sulcus (AKA bicipital groove) – deltoid tuberosity ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy HumerousHumerous – Surgical Neck – Angle of Inclination 130-150 degrees – Angle of Torsion 30 degrees posteriorly ShoulderShoulder ComplexComplex ArticulationsArticulations SternoclavicularSternoclavicular JointJoint – Sternal end of clavicle with manubrium/ 1st costal cartilage – 3 degree of freedom – Articular Disk – Ligaments Capsule Anterior/Posterior Sternoclavicular Ligament Interclavicular Ligament Costoclavicular Ligament ShoulderShoulder ComplexComplex ArticulationsArticulations AcromioclavicularAcromioclavicular JointJoint – 3 degrees of freedom – Articular Disk – Ligaments Superior/Inferior -

Color Enhancement Strategies for 3D Printing of X-Ray Computed Tomography Bone Data for Advanced Anatomy Teaching Models
applied sciences Technical Note Color Enhancement Strategies for 3D Printing of X-ray Computed Tomography Bone Data for Advanced Anatomy Teaching Models Megumi Inoue 1,2, Tristan Freel 2, Anthony Van Avermaete 2 and W. Matthew Leevy 1,2,3,* 1 Department of Biological Sciences, 100 Galvin Life Science Center, University of Notre Dame, Notre Dame, IN 46556, USA; [email protected] 2 IDEA Center Innovation Lab, 1400 E Angela Blvd, South Bend, IN 46617, USA; [email protected] (T.F.); [email protected] (A.V.A.) 3 Harper Cancer Research Institute, University of Notre Dame, Notre Dame, IN 46556, USA * Correspondence: [email protected]; Tel.: +57-4631-1683 Received: 22 January 2020; Accepted: 17 February 2020; Published: 25 February 2020 Abstract: Three-dimensional (3D) printed anatomical models are valuable visual aids that are widely used in clinical and academic settings to teach complex anatomy. Procedures for converting human biomedical image datasets, like X-ray computed tomography (CT), to prinTable 3D files were explored, allowing easy reproduction of highly accurate models; however, these largely remain monochrome. While multi-color 3D printing is available in two accessible modalities (binder-jetting and poly-jet/multi-jet systems), studies embracing the viability of these technologies in the production of anatomical teaching models are relatively sparse, especially for sub-structures within a segmentation of homogeneous tissue density. Here, we outline a strategy to manually highlight anatomical subregions of a given structure and multi-color 3D print the resultant models in a cost-effective manner. Readily available high-resolution 3D reconstructed models are accessible to the public in online libraries. -

UL-Muscles of Back
The back Curvatures • Primary – Concave Anteriorly (Thoracic,Sacral) • Secondry – Convex Anteriorly (Cervical , Lumbar) Back - landmarks Landmarks Scapula – 2nd to 7th rib Acromion – top of shoulder Crest of spine – from acromion medially, downwards Medial border and inf. angle of scapula - palpable Iliac Crest – curved bony ridge below the waist ASIS – Ant. end of iliac crest PSIS – Shallow dimple above buttock approx. 5 cm from median plane Sacrum – Lies between two dimples of PSIS Coccyx – Between buttocks in median plane Spine of C-7 – at root of neck External Occipital protrubance – In Median Plane Superior Nuchal Lines – On either side T3 spine at level of spine of scapula T7 spine at level of inferior angle of scapula L4 – highest point of iliac crest S2 - At PSIS Shoulder Girdle Bones – Scapula -- Clavicle Joints – Sterno-clavicular Acromio-clavicular Muscles of the Back Three groups: • Superficial - muscles that act on the upper limb • Intermediate - muscles of thorax • Deep - muscles of vertebral column Muscles of the Back Muscles of the Back 5 pairs of muscles in the superficial layer • Trapezius • Latissimus dorsi Under Cover of Trepezius • Rhomboid major • Rhomboid minor • Levator scapulae Trapezius Origin • Medial 2/3 of superior nuchal line • Ligamentum Nuche • 7th cervical spine • All thoracic vertebral spines (T1 – T12) Insertion Upper or occipital fibres –post. Border of lat. 1/3 of clavicle Middle fibres – Medial border of Acromion -- Upper lip of crest of spine Lower fibres – Deltoid Tubercle N. Supply Proprioceptive – conveyed by ventral rami of C3 and C4 Motor Fibres – Spinal part of Accessory Nerve Main Action Elevate Scapula – Upper Fibres with Levator Scapulae Retract Scapula – Middle Fibres with Rhomboids Forward Rotation of Scapula – Upper and Lower Fibres with Serratus Ant. -

Origins, Insertions and Prime Mover Actions of Muscles in Figure 6.8
ORIGINS, INSERTIONS AND PRIME MOVER ACTIONS OF MUSCLES IN FIGURE 6.8 Muscle Origin Insertion Actions Adductor Longus Anterior surface of pubis Adducts thigh Adductor Magnus Ischial and pubic rami and ischial tuberosity Medial half of linea aspera Adducts thigh on the femur Biceps Brachii Long head – upper margin of glenoid fossa; Radial (bicipital) tuberosity Flexes and supinates forearm short head – coracoid process of scapula of radius Biceps Femoris Long head – ischial tuberosity; short head – Lateral aspect of head of Flexes knee; long head extends thigh linea aspera of femur fibula and lateral condyle of tibia Brachialis Anterior surface of lower ½ of humerus Anterior surface of Flexes forearm coranoid process of ulna Brachioradialis Upper 2/3rd of lateral supracondylar ridge of Base of styloids process of Flexes forearm humerus humerus Deltoid - Anterior Anterior border of outer 1/3rd of clavicle } Flexes and horizontally flexes humerus } - Medial Acromion process and lateral end of clavicle }Deltoid tuberosity of Abducts and horizontally flexes humerus }humerus (lateral aspect of - Posterior Lower margin of spine of scapula }humerus near midpoint) Extends and horizontally extends } humerus Extensor Digitorum Lateral epicondyle of humerus Distal phalanges of fingers Extends fingers at metacarpophalangeal 2-5 and interphalangeal joints Extensor Digitorum Lateral condyle of tibia and upper ¾ of Second and third phalanges Dorsiflexes and everts foot and extends Longus anterior surface of fibula of four lesser toes toes Extensor Carpi -
The Shoulder Breakdown (PDF)
The Shoulder Breakdown Understand and Apply Scapular Mechanics in Yoga Asana Keri Bergeron, MSPT, ERYT Shoulder Joint(s) • Four joints in one • Scapulothoracic: where scapula moves on ribcage • Glenohumeral joint: where humerus meets scapula (green here) • Acromioclavicular joint: where acromion meets collar bone • Sternoclavicular joint: where collar bone meets sternum • Glenohumeral joint is primary mover • Ball and socket joint • Primary movements: Flex/Ext, IR/ER, ABD/ADD • Designed for stability or mobility? Why? Scapula Anterior View Left Scapula Posterior View Right Scapula Shoulder Motions Defined • Flexion: raise arm forward and up overhead • The general rule is that flexion decreases the angle at a joint • Bending your elbow is the clearest example • Extension: reach or pull arms back behind the plane of your body • The general rule for extension is to increase the angle at a joint • Straightening the elbow from a bent position • Abduction: movement away from the midline of the body • Adduction: movement in towards the midline of the body • External rotation: rotation away from the center • Internal rotation: rotation towards the midline • Keep in mind: there are four joints that are working together to make these motions occur! Scapular Motions Defined • Protraction: spread shoulder blades away from the spine. • Also called abduction • Retraction: draw shoulder blades together towards the spine • Also called retraction • Lateral rotation: rotation away from the midline • Medial rotation: rotation towards the midline • Elevation: draw shoulder blades up towards ears • Depression: draw shoulder blades down toward waist • Keep in mind that these motions most often occur in combination with each other Glenoid Labrum • The labrum of the shoulder is a flexible cartilage ring that makes the socket, the glenoid, a little deeper and in turn, the shoulder slightly more stable. -
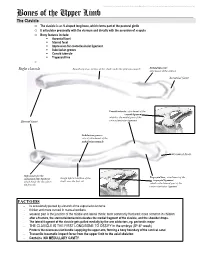
Bones of the Upper Limb
This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. Bones of the Upper Limb The Clavicle o The clavicle is an S-shaped long bone, which forms part of the pectoral girdle o It articulates proximally with the sternum and distally with the acromion of scapula o Bony features include: . Acromial facet . Sternal facet . Impression for costoclavicular ligament . Subclavian groove . Conoid tubercle . Trapezoid line o Right clavicle Smooth superior surface of the shaft, under the platysma muscle Deltoid tubercle: attachment of the deltoid Acromial facet Conoid tubercle, attachment of the conoid ligament which is the medial part of the Sternal facet coracoclavicular ligament Subclavian groove: site of attachment of the subclavius muscle Acromial facet Impression for the Trapezoid line, attachment of the costoclavicular ligament Rough inferior surface of the trapezoid ligament which binds the clavicle to shaft, over the first rib which is the lateral part of the the first rib coracoclavicular ligament FACTOIDS - Its occasionally pierced by a branch of the supraclavicular nerve - thicker and more curved in manual workers - weakest part is the junction of the middle and lateral thirds: most commonly fractured; more common in children - after a fracture, the sternocleidomastoid elevates the medial fragment of the clavicle, and the shoulder drops. - The lateral fragment of the clavicle gets pulled medially by the arm adductors, eg. pectoralis major - THE CLAVICLE IS THE FIRST LONG BONE TO OSSIFY in the embryo (5th-6th week) - Protects the neurovascular bundle supplying the upper arm, forming a bony boundary of the cervical canal - Transmits traumatic impact force from the upper limb to the axial skeleton - Contains NO MEDULLARY CAVITY - This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. -

Upper Extremity Muscle Table
Robert Frysztak, PhD. Structure of the Human Body Loyola University Chicago Stritch School of Medicine UPPER EXTREMITY MUSCLE TABLE PROXIMAL ATTACHMENT DISTAL ATTACHMENT MUSCLE INNERVATION MAIN ACTIONS BLOOD SUPPLY MUSCLE GROUP (ORIGIN) (INSERTION) Flexor carpi radialis Medial epicondyle of humerus Base of 2nd metacarpal Median nerve Flexes and abducts hand at wrist Radial artery Anterior forearm Humeral head: medial epicondyle of Pisiform bone, hook of hamate, base Flexor carpi ulnaris humerus Ulnar head: olecranon and Ulnar nerve Flexes and adducts hand at wrist Posterior ulnar recurrent artery Anterior forearm of 5th metacarpal posterior border of ulna Medial and anterior surface of Flexes distal phalanges of medial four Palmar base of distal phalanges of Medial part: ulnar nerve Lateral Anterior interosseous artery, Flexor digitorum profundus proximal 3/4 of ulna and digits, assists with flexion of hand at Anterior forearm medial four digits part: median nerve muscular branches of ulnar artery interosseous membrane wrist Humero‐ulnar head: medial epicondyle of humerus and coronoid Flexes middle and proximal Bodies of middle phalanges of medial Flexor digitorum superficialis process of ulna Median nerve phalanges of medial four digits, flexes Ulnar and radial arteries Anterior forearm four digits Radial head: superior half of anterior hand at wrist radius Anterior surface of radius and Palmar base of distal phalanx of Flexor pollicis longus Median nerve (anterior interosseous) Flexes phalanges of thumb Anterior interosseous artery -

The Shoulder
LWBK325-C06-239-291.qxd 5/1/09 6:18 PM Page 239 SECTION I: OVERVIEWSECTION OF III: THEORY THE UPPER AND EXTREMITIES TECHNIQUE 6 The Shoulder ain in the shoulder and shoulder girdle is common in the general population, with a prevalence of 15% to 25% in the 40- to 50-year-old age group.1 With increasing life expectancy and the aging population remaining active into advancing years, age- related degeneration is a significant factor in rotator cuf Pinjuries.2 Disorders of the shoulder region account for 30% to 40% of indus- trial complaints and have increased sixfold in the past decade.1 Although injuries to the shoulder girdle account for only 5% to 10% of sports injuries, they represent a much higher percentage of physician visits, proba- bly because they are perceived as being serious or disabling by the athlete.3 In many shoulder disorders, it is the soft tissue, such as the tendons and joint capsule, that is the source of the pain. The shoulder region may also be painful from a referral from the cervical and the thoracic spines and from visceral diseases, such as gallbladder and cardiac problems.4 239 LWBK325-C06-239-291.qxd 5/1/09 3:51 PM Page 240 240 Chapter 6: The Shoulder | Anatomy, Function, and Dysfunction of the Shoulder Complex Anatomy, Function, and Dysfunction of the Shoulder Complex spine and the thoracic spine influence mobility o GENERAL OVERVIEW the arm. The upper thoracic vertebrae must be able to extend, rotate, and side-bend to accomplish full 1 ■ The bones of the shoulder complex includes the elevation of the arm.