Lassa Fever in Nigeria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Linking Behavior, Co-Infection Patterns, and Viral Infection Risk with the Whole Gastrointestinal Helminth Community Structure in Mastomys Natalensis
ORIGINAL RESEARCH published: 17 August 2021 doi: 10.3389/fvets.2021.669058 Linking Behavior, Co-infection Patterns, and Viral Infection Risk With the Whole Gastrointestinal Helminth Community Structure in Mastomys natalensis Bram Vanden Broecke 1*, Lisse Bernaerts 1, Alexis Ribas 2, Vincent Sluydts 1, Ladslaus Mnyone 3, Erik Matthysen 1 and Herwig Leirs 1 1 Evolutionary Ecology Group, Department of Biology, University of Antwerp, Antwerp, Belgium, 2 Parasitology Section, Department of Biology, Healthcare and Environment, Faculty of Pharmacy and Food Science, IRBio (Research Institute of Biodiversity), University of Barcelona, Barcelona, Spain, 3 Pest Management Center, Sokoine University of Agriculture, Morogoro, Tanzania Edited by: Yadong Zheng, Infection probability, load, and community structure of helminths varies strongly between Lanzhou Institute of Veterinary and within animal populations. This can be ascribed to environmental stochasticity Research (CAAS), China or due to individual characteristics of the host such as their age or sex. Other, but Reviewed by: Mario Garrido, understudied, factors are the hosts’ behavior and co-infection patterns. In this study, we Ben-Gurion University of the used the multimammate mouse (Mastomys natalensis) as a model system to investigate Negev, Israel Si-Yang Huang, how the hosts’ sex, age, exploration behavior, and viral infection history affects their Yangzhou University, China infection risk, parasitic load, and community structure of gastrointestinal helminths. We Hannah Rose Vineer, hypothesized that the hosts’ exploration behavior would play a key role in the risk for University of Liverpool, United Kingdom infection by different gastrointestinal helminths, whereby highly explorative individuals *Correspondence: would have a higher infection risk leading to a wider diversity of helminths and a larger Bram Vanden Broecke load compared to less explorative individuals. -

Establishment of a Genetically Confirmed Breeding Colony of Mastomys Natalensis from Wild-Caught Founders from West Africa
viruses Article Establishment of a Genetically Confirmed Breeding Colony of Mastomys natalensis from Wild-Caught Founders from West Africa David Safronetz 1,*,†, Kyle Rosenke 1, Robert J. Fischer 2,‡, Rachel A. LaCasse 3, Dana P. Scott 3, Greg Saturday 3, Patrick W. Hanley 3, Ousmane Maiga 4, Nafomon Sogoba 4, Tom G. Schwan 2 and Heinz Feldmann 1,* 1 Laboratory of Virology, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, MT 59840, USA; [email protected] 2 Laboratory of Zoonotic Pathogens, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, MT 59840, USA; fi[email protected] (R.J.F.); [email protected] (T.G.S.) 3 Rocky Mountain Veterinary Branch, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, MT 59840, USA; [email protected] (R.A.L.); [email protected] (D.P.S.); [email protected] (G.S.); [email protected] (P.W.H.) 4 International Center for Excellence in Research (ICER-Mali), Faculty of Medicine and Odonto Stomatology, University of Sciences, Techniques and Technologies of Bamako (USTTB), Bamako, Mali; [email protected] (O.M.); [email protected] (N.S.) * Correspondence: [email protected] (D.S.); [email protected] (H.F.) † Current address: Zoonotic Diseases and Special Pathogens, Public Health Agency of Canada, Winnipeg, MB R3E 3R2, Canada. Citation: Safronetz, D.; Rosenke, K.; ‡ Current Address: Laboratory of Virology, Rocky Mountain Laboratories, National Institute of Allergy Fischer, R.J.; LaCasse, R.A.; Scott, D.P.; and Infectious Diseases, National Institutes of Health, Hamilton, MT 59840, USA. -

Mastomys Spp. – Multimammate Mouse
Mastomys spp. – Multimammate Mouse Taxonomic status: Species Taxonomic notes: A good review of the systematics of Mastomys is provided by Granjon et al. (1997). Mastomys spp. are cryptic and difficult to distinguish morphologically but clearly separable by molecular and chromosomal markers (Britton-Davidian et al. 1995; Lecompte et al. 2005). For example, within the assessment region, M. coucha and M. natalensis can be distinguished only through chromosome number (in M. coucha 2n = 36; in M. natalensis 2n = 32) and molecular markers (Colangelo et al. 2013) but not on cranio-dental features, nor a multivariate analysis (Dippenaar et al. 1993). Mastomys coucha – Richard Yarnell Assessment Rationale Regional Red List status (2016) Both species are listed as Least Concern as they have a Mastomys coucha Least Concern wide distribution within the assessment region, where they likely occur in most protected areas, are abundant in Mastomys natalensis Least Concern human-transformed areas, including agricultural areas and areas affected by human disturbances, and because National Red List status (2004) there are no significant threats that could cause range- Mastomys coucha Least Concern wide decline. Additionally, these species are known as prolific breeders with population numbers likely to recover Mastomys natalensis Least Concern quickly after a decline. Because of their reproductive Reasons for change No change characteristics, population eruptions often occur under favourable conditions. Landowners and managers should Global Red List status (2016) pursue ecologically-based rodent management strategies Mastomys coucha Least Concern and biocontrol instead of rodenticides to regulate population explosions of this species. Mastomys natalensis Least Concern Regional population effects: For M. coucha, significant TOPS listing (NEMBA) (2007) None dispersal is unlikely because the bulk of the population CITES listing None occurs within the assessment region. -

TANZANIA One Health in Action (2009-2020) a One Health Approach to Strengthening National Health Security TANZANIA
TANZANIA One Health in action (2009-2020) A One Health approach to strengthening national health security TANZANIA Since 2009, UC Davis, the Sokoine is considered a hotspot for viral transmission, and delivered critical University of Agriculture (SUA), and spillover and spread due to land data and insights for strengthening government partners, have worked conversion, human population health security and refining national to advance One Health capacity and movement from neighboring surveillance plans. wildlife laboratory infrastructure in Uganda, Rwanda, and Burundi, and Tanzania. During PREDICT-1, our intensive livestock development. Our In addition, by putting stakeholder One Health team targeted high-risk team’s work has provided proof of engagement and community human-wildlife interfaces, collected concept for applying the One Health outreach at the forefront of our samples from wildlife, and tested approach in Tanzania, strengthened approach, we worked directly with them for viral threats. IIn the first five subnational and district-level One communities at all levels to identify years, 63 viruses were detected (12 Health platforms by training animal practical and actionable disease known viruses and 51 new viruses). and human health professionals on prevention and control strategies. the frontlines of zoonotic disease Building on these successes, our transmission, shed light on the team partnered with the Ifakara viruses and pathogens circulating Health Institute (IHI) to launch in animal and human populations intensive One Health -

Zimbabwe Zambia Malawi Species Checklist Africa Vegetation Map
ZIMBABWE ZAMBIA MALAWI SPECIES CHECKLIST AFRICA VEGETATION MAP BIOMES DeserT (Namib; Sahara; Danakil) Semi-deserT (Karoo; Sahel; Chalbi) Arid SAvannah (Kalahari; Masai Steppe; Ogaden) Grassland (Highveld; Abyssinian) SEYCHELLES Mediterranean SCruB / Fynbos East AFrican Coastal FOrest & SCruB DrY Woodland (including Mopane) Moist woodland (including Miombo) Tropical Rainforest (Congo Basin; upper Guinea) AFrO-Montane FOrest & Grassland (Drakensberg; Nyika; Albertine rift; Abyssinian Highlands) Granitic Indian Ocean IslandS (Seychelles) INTRODUCTION The idea of this booklet is to enable you, as a Wilderness guest, to keep a detailed record of the mammals, birds, reptiles and amphibians that you observe during your travels. It also serves as a compact record of your African journey for future reference that hopefully sparks interest in other wildlife spheres when you return home or when travelling elsewhere on our fragile planet. Although always exciting to see, especially for the first-time Africa visitor, once you move beyond the cliché of the ‘Big Five’ you will soon realise that our wilderness areas offer much more than certain flagship animal species. Africa’s large mammals are certainly a big attraction that one never tires of, but it’s often the smaller mammals, diverse birdlife and incredible reptiles that draw one back again and again for another unparalleled visit. Seeing a breeding herd of elephant for instance will always be special but there is a certain thrill in seeing a Lichtenstein’s hartebeest, cheetah or a Lilian’s lovebird – to name but a few. As a globally discerning traveller, look beyond the obvious, and challenge yourself to learn as much about all wildlife aspects and the ecosystems through which you will travel on your safari. -
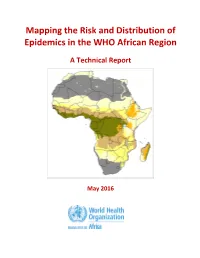
Mapping the Risk and Distribution of Epidemics in the WHO African Region
Mapping the Risk and Distribution of Epidemics in the WHO African Region A Technical Report May 2016 WHO/AFRO Library Cataloguing – in – Publication Data Mapping the Risk and Distribution of Epidemics in the WHO African Region: a technical report 1. Disease Outbreaks – statistics and numerical data 2. Epidemics – statistics and numerical data 3. Communicable Diseases – statistics and numerical data 4. Risk Assessment – supply and distribution – statistics and numerical data 5. Data collection – utilization 6. Africa I. Work Health Organization. Regional Office for Africa II. Title ISBN: 978-9290233084-4 (NLM Classification : WA 105) © WHO Regional Office for Africa, 2016 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. Copies of this publication may be obtained from the Library, WHO Regional Office for Africa, P.O. Box 6, Brazzaville, Republic of Congo (Tel: +47 241 39100; Fax: +47 241 39507; E-mail: [email protected]). Requests for permission to reproduce or translate this publication – whether for sale or for non-commercial distribution – should be sent to the same address. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Appendix a Flora Species Recorded
APPENDIX A FLORA SPECIES RECORDED Environmental Scoping Report Plant Species Identified During Field Survey (April 2017) Trees Shrubs Forbs Grasses Cyperoids Acacia sieberiana Gnidia kraussiana Achyranthes Andropogon Cyperus digitatus aspera eucomus Albizia antunesiana Blumea alata Amaranthus Andropogon Cyperus hybridus gayanus esculentus Brachystegia Eriosema ellipticum Bidens biternata Aristida junciformis Cyperus tenax spiciformis Burkea africana Eriosema Bidens pilosa Arundinella Kylinga erecta engleranum nepalensis Combretum molle Euclea crispa C. albida Brachiaria deflexa Pycreus aethiops Cussonia arborea Gnidia kraussiana Ceratotheca triloba Cynodon dactylon Typha latifolius Ekebergia Helichrysum Conyza albida Dactyloctenium benguelensis kraussii aegyptium Faurea speciosa Indigofera arrecta Conyza welwitschii Digitaria scalarum Julbemardia Lantana camara Datura stramonium Eleusine indica globiflora Kigellia africana Leptactina Euphorbia Eragrostis benguelensis cyparissoides capensis Ochna puhra Lippia javanica Haumaniastrum Eragrostis sericeum chapelieri Ozoroa insignis Lopholaena Helichrysum Eragrostis spp. coriifolia species Parinari Maytenus Kniphofia Hemarthria curatellifolia heterophylla linearifolia altissima Strychnos spinosa Maytenus Oldenlandia Heteropogon senegalensis corymbosa contortus Vangueria infausta Pavetta Oldenlandia Hyparrhenia schumanniana herbacea filipendula Senna Rhynchosia Polygonum Hyperthelia didymobotrya resinosa senegalense dissoluta Ranunculus Melinis repens multifidus Senecio strictifolius Monocymbium -

Lassa International Conference (LIC) 15 – 19 Jan 2019 Abuja, Nigeria
Meeting brief: Lassa International Conference (LIC) 15 – 19 Jan 2019 Abuja, Nigeria Background (from LIC website): 50 years since the detection of Lassa fever in Nigeria, outbreaks have been recorded yearly in parts of the country. In 2018, Nigeria experienced the largest reported outbreak of Lassa Fever with 21 of 36 States in the country affected. The 50th year of discovery of the Lassa fever is an opportunity for the scientific community to reflect on what is known, describe gaps that exist and prioritize the research agenda for the future. Contents 1 Plenary session, Day 1 ..................................................................................................................................................................4 1.1. Nigeria’s 2018 Lassa fever outbreak and lessons for the future ............................................................................................................. 4 1.2. The Irrua Specialist Teaching Hospital (ISTH)’s role in the fight against Lassa fever in Nigeria ............................................................... 4 1.3. How a North-South relationship has improved our understanding of Lassa fever globally .................................................................... 4 1.4. CEPI’s role in the opportunity and responsibility for clinical trials in Africa ............................................................................................ 5 2 Parallel sessions, Day 1:................................................................................................................................................................5 -

Lassa Virus Circulation in Small Mammal Populations in Bo District, Sierra Leone
biology Article Lassa Virus Circulation in Small Mammal Populations in Bo District, Sierra Leone Umaru Bangura 1,2,* , Jacob Buanie 1, Joyce Lamin 1, Christopher Davis 3,Gédéon Ngiala Bongo 2, Michael Dawson 1, Rashid Ansumana 1, Dianah Sondufu 1, Emma C. Thomson 3, Foday Sahr 4 and Elisabeth Fichet-Calvet 2,* 1 Mercy Hospital Research Laboratory, Bo, Sierra Leone; [email protected] (J.B.); [email protected] (J.L.); [email protected] (M.D.); [email protected] (R.A.); [email protected] (D.S.) 2 Department of Virology, Bernhard Nocht Institute for Tropical Medicine, 20359 Hamburg, Germany; [email protected] 3 Centre for Virus Research, University of Glasgow, Glasgow G61 1QH, UK; [email protected] (C.D.); [email protected] (E.C.T.) 4 College of Medicine and Allied Health Sciences, University of Sierra Leone, Freetown PMB 595, Sierra Leone; [email protected] * Correspondence: [email protected] (U.B.); fi[email protected] (E.F.-C.) Simple Summary: Lassa fever is a viral hemorrhagic fever caused by the Lassa virus (LASV). It is a deadly rodent-borne zoonosis with outbreaks occurring mostly in Sierra Leone, Guinea, Liberia, and Nigeria, in West Africa. In Sierra Leone, surveillance activities of LASV focus mainly on the Kenema area in the eastern region, known to be the epicentre. Little is known about the presence of the virus in the Bo area, where Mastomys natalensis and Rattus rattus share habitats with humans. Our study investigated the circulation and phylogeny of new LASV strains and virus seroprevalence in rodent populations of villages in Bo district. -

Rodent Control to Fight Lassa Fever: Evaluation and Lessons Learned from a 4-Year Study in Upper Guinea
RESEARCH ARTICLE Rodent control to fight Lassa fever: Evaluation and lessons learned from a 4-year study in Upper Guinea 1 2 2 2 Almudena Mari SaezID *, Mory Cherif Haidara , Amara Camara , Fode Kourouma , MickaeÈl Sage3, N'Faly Magassouba2, Elisabeth Fichet-Calvet4 1 Global Health and Biosecurity Unit, Robert Koch Institute, Berlin, Germany, 2 Projet des fièvres HeÂmorragiques en GuineÂe, Laboratoire de Virologie, Conakry, Guinea, 3 CD Eau Environnement, Maizières, France and Faune Environment Expertise, Besancon, France, 4 Department of Virology, Bernhard Nocht a1111111111 Institute for Tropical Medicine, Hamburg, Germany a1111111111 a1111111111 * [email protected] a1111111111 a1111111111 Abstract Lassa fever is a viral haemorrhagic fever caused by an arenavirus. The disease is endemic in West African countries, including Guinea. The rodents Mastomys natalensis and Mast- OPEN ACCESS omys erythroleucus have been identified as Lassa virus reservoirs in Guinea. In the Citation: Mari Saez A, Cherif Haidara M, Camara A, Kourouma F, Sage M, Magassouba N'Faly, et al. absence of a vaccine, rodent control and human behavioural changes are the only options (2018) Rodent control to fight Lassa fever: to prevent Lassa fever in highly endemic areas. We performed a 4 year intervention based Evaluation and lessons learned from a 4-year study on chemical rodent control, utilizing anticoagulant rodenticides in 3 villages and evaluating in Upper Guinea. PLoS Negl Trop Dis 12(11): the rodent abundance before and after treatment. Three additional villages were investi- e0006829. https://doi.org/10.1371/journal. pntd.0006829 gated as controls. Analyses to assess the effectiveness of the intervention, bait consump- tion and rodent dynamics were performed. -

Appendix a Letter from Environmental Affairs
APPENDIX A LETTER FROM ENVIRONMENTAL AFFAIRS DEPARTMENT Environmental Scoping Report APPENDIX B FLORA SPECIES RECORDED Environmental Scoping Report Plant Species Identified During Field Survey (April 2017) Trees Shrubs Forbs Grasses Cyperoids Acacia sieberiana Gnidia kraussiana Achyranthes Andropogon Cyperus digitatus aspera eucomus Albizia antunesiana Blumea alata Amaranthus Andropogon Cyperus hybridus gayanus esculentus Brachystegia Eriosema ellipticum Bidens biternata Aristida junciformis Cyperus tenax spiciformis Burkea africana Eriosema Bidens pilosa Arundinella Kylinga erecta engleranum nepalensis Combretum molle Euclea crispa C. albida Brachiaria deflexa Pycreus aethiops Cussonia arborea Gnidia kraussiana Ceratotheca triloba Cynodon dactylon Typha latifolius Ekebergia Helichrysum Conyza albida Dactyloctenium benguelensis kraussii aegyptium Faurea speciosa Indigofera arrecta Conyza welwitschii Digitaria scalarum Julbemardia Lantana camara Datura stramonium Eleusine indica globiflora Kigellia africana Leptactina Euphorbia Eragrostis benguelensis cyparissoides capensis Ochna puhra Lippia javanica Haumaniastrum Eragrostis sericeum chapelieri Ozoroa insignis Lopholaena Helichrysum Eragrostis spp. coriifolia species Parinari Maytenus Kniphofia Hemarthria curatellifolia heterophylla linearifolia altissima Strychnos spinosa Maytenus Oldenlandia Heteropogon senegalensis corymbosa contortus Vangueria infausta Pavetta Oldenlandia Hyparrhenia schumanniana herbacea filipendula Senna Rhynchosia Polygonum Hyperthelia didymobotrya resinosa senegalense -
Three Arenaviruses in Three Subspecific Natal Multimammate Mouse Taxa in Tanzania: Same Host Specificity, but Different Spatial Genetic Structure?
Three arenaviruses in three subspecific natal multimammate mouse taxa in Tanzania: Same host specificity, but different spatial genetic structure? Item Type Article; text Authors Cuypers, L.N.; Baird, S.J.E.; Hánová, A.; Locus, T.; Katakweba, A.S.; Gryseels, S.; Bryja, J.; Leirs, H.; de, Bellocq, J.G. Citation Cuypers, L. N., Baird, S. J., Hánová, A., Locus, T., Katakweba, A. S., Gryseels, S., ... & Goüy de Bellocq, J. (2020). Three arenaviruses in three subspecific natal multimammate mouse taxa in Tanzania: same host specificity, but different spatial genetic structure?. Virus evolution, 6(2), veaa039. DOI 10.1093/ve/veaa039 Publisher Oxford University Press Journal Virus Evolution Rights Copyright © The Author(s) 2020. Published by Oxford University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/). Download date 02/10/2021 20:38:59 Item License https://creativecommons.org/licenses/by-nc/4.0/ Version Final published version Link to Item http://hdl.handle.net/10150/659641 Virus Evolution, 2020, 6(2): veaa039 doi: 10.1093/ve/veaa039 Research Article Three arenaviruses in three subspecific natal Downloaded from https://academic.oup.com/ve/article/6/2/veaa039/5840739 by University of Arizona user on 21 May 2021 multimammate mouse taxa in Tanzania: same host specificity, but different spatial genetic structure? Laura N. Cuypers,1,*,† Stuart J. E. Baird,2 Alexandra Ha´nova´,2,3 Tatjana Locus,1 Abdul S. Katakweba,4 Sophie