VTE) Cindy Ward, DNP, RN-BC, CMSRN, ACNS-BC
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CDK4/6 Inhibitors in Breast Cancer Treatment: Potential Interactions with Drug, Gene and Pathophysiological Conditions
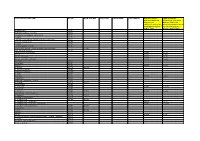
Review CDK4/6 Inhibitors in Breast Cancer Treatment: Potential Interactions with Drug, Gene and Pathophysiological Conditions Rossana Roncato 1,*,†, Jacopo Angelini 2,†, Arianna Pani 2,3,†, Erika Cecchin 1, Andrea Sartore-Bianchi 2,4, Salvatore Siena 2,4, Elena De Mattia 1, Francesco Scaglione 2,3,‡ and Giuseppe Toffoli 1,‡ 1 1 Experimental and Clinical Pharmacology Unit, Centro di Riferimento Oncologico (CRO), IRCCS, 33081 Aviano, Italy; [email protected] (E.C.); [email protected] (E.D.M.); [email protected] (G.T.) 2 Department of Oncology and Hemato-Oncology, Università degli Studi di Milano, 20122 Milan, Italy; [email protected] (J.A.); [email protected] (A.P.); [email protected] (A.S-B.); [email protected] (S.S.); [email protected] (F.S.) 3 Clinical Pharmacology Unit, ASST Grande Ospedale Metropolitano Niguarda, Piazza dell'Ospedale Maggiore 3, 20162 Milan, Italy 4 Department of Hematology and Oncology, Niguarda Cancer Center, Grande Ospedale Metropolitano Niguarda, 20162 Milan, Italy * Correspondence: [email protected]; Tel.:+390434659130 † These authors contributed equally. ‡ These authors share senior authorship. Int. J. Mol. Sci. 2020, 21, x; doi: www.mdpi.com/journal/ijms Int. J. Mol. Sci. 2020, 21, x 2 of 8 Table S1. Co-administered agents categorized according to their potential risk for Drug-Drug interaction (DDI) in combination with CDK4/6 inhibitors (CDKis). Colors suggest the risk of DDI with CDKis: green, low risk DDI; orange, moderate risk DDI; red, high risk DDI. ADME, absorption, distribution, metabolism, and excretion; GI, Gastrointestinal; TdP, Torsades de Pointes; NTI, narrow therapeutic index. * Cardiological toxicity should be considered especially for ribociclib due to the QT prolongation. -

GTH 2021 State of the Art—Cardiac Surgery: the Perioperative Management of Heparin-Induced Thrombocytopenia in Cardiac Surgery
Review Article 59 GTH 2021 State of the Art—Cardiac Surgery: The Perioperative Management of Heparin-Induced Thrombocytopenia in Cardiac Surgery Laura Ranta1 Emmanuelle Scala1 1 Department of Anesthesiology, Cardiothoracic and Vascular Address for correspondence Emmanuelle Scala, MD, Centre Anesthesia, Lausanne University Hospital (CHUV), Lausanne, Hospitalier Universitaire Vaudois, Rue du Bugnon 46, BH 05/300, 1011 Switzerland Lausanne, Suisse, Switzerland (e-mail: [email protected]). Hämostaseologie 2021;41:59–62. Abstract Heparin-induced thrombocytopenia (HIT) is a severe, immune-mediated, adverse drug Keywords reaction that paradoxically induces a prothrombotic state. Particularly in the setting of ► Heparin-induced cardiac surgery, where full anticoagulation is required during cardiopulmonary bypass, thrombocytopenia the management of HIT can be highly challenging, and requires a multidisciplinary ► cardiac surgery approach. In this short review, the different perioperative strategies to run cardiopul- ► state of the art monary bypass will be summarized. Introduction genicity of the antibodies and is diagnostic for HIT. The administration of heparin to a patient with circulating Heparin-induced thrombocytopenia (HIT) is a severe, im- pathogenic HITabs puts the patient at immediate risk of mune-mediated, adverse drug reaction that paradoxically severe thrombotic complications. induces a prothrombotic state.1,2 Particularly in the setting The time course of HIT can be divided into four distinct of cardiac surgery, where full anticoagulation is required phases.6 Acute HIT is characterized by thrombocytopenia during cardiopulmonary bypass (CPB), the management of and/or thrombosis, the presence of HITabs, and confirma- HIT can be highly challenging, and requires a multidisciplin- tion of their platelet activating capacity by a functional ary approach. -
List of Union Reference Dates A
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Ventavis, INN-Iloprost
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Ventavis 10 microgram/ml nebuliser solution Ventavis 20 microgram/ml nebuliser solution 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Ventavis 10 microgram/ml nebuliser solution 1 ml solution contains 10 microgram iloprost (as iloprost trometamol). Each ampoule with 1 ml solution contains 10 microgram iloprost. Each ampoule with 2 ml solution contains 20 microgram iloprost. Ventavis 20 microgram/ml nebuliser solution 1 ml solution contains 20 microgram iloprost (as iloprost trometamol). Each ampoule with 1 ml solution contains 20 microgram iloprost. Excipient with known effect • Ventavis 10 microgram/ml: Each ml contains 0.81 mg ethanol 96% (equivalent to 0.75 mg ethanol) • Ventavis 20 microgram/ml: Each ml contains 1.62 mg ethanol 96% (equivalent to 1.50 mg ethanol). For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Nebuliser solution. Ventavis 10 microgram/ml nebuliser solution Clear, colourless solution. Ventavis 20 microgram/ml nebuliser solution Clear, colourless to slightly yellowish solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Treatment of adult patients with primary pulmonary hypertension, classified as NYHA functional class III, to improve exercise capacity and symptoms. 4.2 Posology and method of administration Drug product Suitable inhalation device (nebuliser) to be used Ventavis 10 microgram/ml Breelib I-Neb AAD Venta-Neb Ventavis 20 microgram/ml Breelib I-Neb AAD Ventavis should only be initiated and monitored by a physician experienced in the treatment of pulmonary hypertension. 2 Posology Dose per inhalation session At initiation of Ventavis treatment the first inhaled dose should be 2.5 microgram iloprost as delivered at the mouthpiece of the nebuliser. -

Clinical Trial Protocol: BPS-314D-MR-PAH-302
Clinical Trial Protocol: BPS-314d-MR-PAH-302 Study Title: A multicenter, double-blind, randomized, placebo-controlled, Phase 3 study to assess the efficacy and safety of oral BPS-314d-MR added-on to treprostinil, inhaled (Tyvaso®) in subjects with pulmonary arterial hypertension Study Number: BPS-314d- MR-PAH-302 Study Phase: 3 Product Name: Beraprost Sodium 314d Modified Release IND Number: 111,729 Indication: Treatment of Pulmonary Arterial Hypertension Investigators: Multicenter Sponsor: Lung Biotechnology Inc. Sponsor Contact: Medical Monitor: Date Original Protocol: 16 April 2013 Amendment 1: 17 December 2013 Amendment 2 15 October 2014 GCP Statement: This study will be conducted in compliance with the protocol, Good Clinical Practice (GCP) and applicable regulatory requirements. Confidentiality Statement The concepts and information contained herein are confidential and proprietary and shall not be disclosed in whole or part without the express written consent of Lung Biotechnology Inc. © 2014 Lung Biotechnology Inc. Beraprost Sodium 314d Modified Release Lung Biotechnology Inc. Clinical Trial Protocol: BPS-314-d-MR-PAH 302 15 October 2014 LIST OF CONTACTS Study Sponsor: Lung Biotechnology Inc. 1040 Spring Street Silver Spring, Maryland 20910 United States Phone: 301-608-9292 Fax: 301-589-0855 Sponsor Contact: Medical Monitor: SAE Reporting: CONFIDENTIAL Page 2 of 75 Beraprost Sodium 314d Modified Release Lung Biotechnology Inc. Clinical Trial Protocol: BPS-314-d-MR-PAH 302 15 October 2014 SYNOPSIS Sponsor: Lung Biotechnology Inc. -

Evaluation of Low-Dose Aspirin for Primary Prevention of Ischemic
Kim et al. Diabetology & Metabolic Syndrome (2015) 7:8 DIABETOLOGY & DOI 10.1186/s13098-015-0002-y METABOLIC SYNDROME RESEARCH Open Access Evaluation of low-dose aspirin for primary prevention of ischemic stroke among patients with diabetes: a retrospective cohort study Ye-Jee Kim1†, Nam-Kyong Choi2,3†, Mi-Sook Kim4, Joongyub Lee2, Yoosoo Chang5, Jong-Mi Seong1, Sun-Young Jung1, Ju-Young Shin1, Ji-Eun Park6,7 and Byung-Joo Park1,4,6* Abstract Background: Low-dose aspirin is recommended to reduce the risk of cardiovascular disease. However, the questions with regard to primary prevention have been raised among patients with diabetes. We evaluated low-dose aspirin use for preventing ischemic stroke in patients with diabetes using a national health insurance database. Methods: Using data from the Korean Health Insurance Review and Assessment Service database from January 1, 2005, through December 31, 2009, a population-based retrospective cohort study was conducted with incident patients with diabetes aged 40 to 99 years old with the initial use of low-dose aspirin during the index period from January 1, 2006 to December 31, 2007. We matched each low-dose aspirin user to one non-user using a propensity score. The Cox proportional hazards model was used to compare the risk of hospitalization for ischemic stroke in users and nonusers of low-dose aspirin until December 31, 2009. Results: Out of 261,065 incident patients with diabetes, 15,849 (6.2%) were low-dose aspirin users. Compared to non-users, the adjusted hazard ratio (95% confidence interval) of low-dose aspirin users for hospitalization due to ischemic stroke was 1.73 (95% CI; 1.41-2.12). -

Effect of Prostanoids on Human Platelet Function: an Overview
International Journal of Molecular Sciences Review Effect of Prostanoids on Human Platelet Function: An Overview Steffen Braune, Jan-Heiner Küpper and Friedrich Jung * Institute of Biotechnology, Molecular Cell Biology, Brandenburg University of Technology, 01968 Senftenberg, Germany; steff[email protected] (S.B.); [email protected] (J.-H.K.) * Correspondence: [email protected] Received: 23 October 2020; Accepted: 23 November 2020; Published: 27 November 2020 Abstract: Prostanoids are bioactive lipid mediators and take part in many physiological and pathophysiological processes in practically every organ, tissue and cell, including the vascular, renal, gastrointestinal and reproductive systems. In this review, we focus on their influence on platelets, which are key elements in thrombosis and hemostasis. The function of platelets is influenced by mediators in the blood and the vascular wall. Activated platelets aggregate and release bioactive substances, thereby activating further neighbored platelets, which finally can lead to the formation of thrombi. Prostanoids regulate the function of blood platelets by both activating or inhibiting and so are involved in hemostasis. Each prostanoid has a unique activity profile and, thus, a specific profile of action. This article reviews the effects of the following prostanoids: prostaglandin-D2 (PGD2), prostaglandin-E1, -E2 and E3 (PGE1, PGE2, PGE3), prostaglandin F2α (PGF2α), prostacyclin (PGI2) and thromboxane-A2 (TXA2) on platelet activation and aggregation via their respective receptors. Keywords: prostacyclin; thromboxane; prostaglandin; platelets 1. Introduction Hemostasis is a complex process that requires the interplay of multiple physiological pathways. Cellular and molecular mechanisms interact to stop bleedings of injured blood vessels or to seal denuded sub-endothelium with localized clot formation (Figure1). -

Treprostinil for Pulmonary Hypertension
REVIEW Treprostinil for pulmonary hypertension Nika Skoro-Sajer1 Abstract: Treprostinil is a stable, long-acting prostacyclin analogue which can be admin- Irene Lang1 istered as a continuous subcutaneous infusion using a portable miniature delivery system. Robert Naeije2 Subcutaneous treprostinil has been shown in a large multicenter randomized controlled trial to improve exercise capacity, clinical state, functional class, pulmonary hemodynamics, and 1Division of Cardiology, Department of Internal Medicione II, Vienna quality of life in patients with pulmonary arterial hypertension, an uncommon disease of poor General Hospital, Medical University prognosis. Side effects include facial fl ush, headache, jaw pain, abdominal cramping, and diar- 2 of Vienna, Austria; Department rhea, all typical of prostacyclin, and manageable by symptom-directed dose adjustments, and of Cardiology, Erasme University Hospital, Brussels, Belgium infusion site pain which may make further treatment impossible in 7%–10% of the patients. Long-term survival in pulmonary arterial hypertension patients treated with subcutaneous treprostinil is similar to that reported with intravenous epoprostenol. There are uncontrolled data suggesting effi cacy of subcutaneous treprostinil in chronic thromboembolic pulmonary hypertension. Treprostinil can also be administered intravenously, although increased doses, up to 2–3 times those given subcutaneously, appear to be needed to obtain the same effi cacy. Preliminary results of a randomized controlled trial of inhaled treprostinil -
Modifications to the Harmonized Tariff Schedule of the United States To
U.S. International Trade Commission COMMISSIONERS Shara L. Aranoff, Chairman Daniel R. Pearson, Vice Chairman Deanna Tanner Okun Charlotte R. Lane Irving A. Williamson Dean A. Pinkert Address all communications to Secretary to the Commission United States International Trade Commission Washington, DC 20436 U.S. International Trade Commission Washington, DC 20436 www.usitc.gov Modifications to the Harmonized Tariff Schedule of the United States to Implement the Dominican Republic- Central America-United States Free Trade Agreement With Respect to Costa Rica Publication 4038 December 2008 (This page is intentionally blank) Pursuant to the letter of request from the United States Trade Representative of December 18, 2008, set forth in the Appendix hereto, and pursuant to section 1207(a) of the Omnibus Trade and Competitiveness Act, the Commission is publishing the following modifications to the Harmonized Tariff Schedule of the United States (HTS) to implement the Dominican Republic- Central America-United States Free Trade Agreement, as approved in the Dominican Republic-Central America- United States Free Trade Agreement Implementation Act, with respect to Costa Rica. (This page is intentionally blank) Annex I Effective with respect to goods that are entered, or withdrawn from warehouse for consumption, on or after January 1, 2009, the Harmonized Tariff Schedule of the United States (HTS) is modified as provided herein, with bracketed matter included to assist in the understanding of proclaimed modifications. The following supersedes matter now in the HTS. (1). General note 4 is modified as follows: (a). by deleting from subdivision (a) the following country from the enumeration of independent beneficiary developing countries: Costa Rica (b). -

Statistical Analysis Plan – Part 1
NCT03251482 Janssen Research & Development Statistical Analysis Plan – Part 1 A Randomized, Double-blind, Double-dummy, Multicenter, Adaptive Design, Dose Escalation (Part 1) and Dose-Response (Part 2) Study to Evaluate the Safety and Efficacy of Intravenous JNJ-64179375 Versus Oral Apixaban in Subjects Undergoing Elective Total Knee Replacement Surgery Protocol 64179375THR2001; Phase 2 JNJ-64179375 Status: Approved Date: 18 October 2017 Prepared by: Janssen Research & Development, LLC Document No.: EDMS-ERI-148215770 Compliance: The study described in this report was performed according to the principles of Good Clinical Practice (GCP). Confidentiality Statement The information in this document contains trade secrets and commercial information that are privileged or confidential and may not be disclosed unless such disclosure is required by applicable law or regulations. In any event, persons to whom the information is disclosed must be informed that the information is privileged or confidential and may not be further disclosed by them. These restrictions on disclosure will apply equally to all future information supplied to you that is indicated as privileged or confidential. 1 Approved, Date: 18 October 2017 JNJ-64179375 NCT03251482 Statistical Analysis Plan - Part 1 64179375THR2001 TABLE OF CONTENTS TABLE OF CONTENTS ............................................................................................................................... 2 LIST OF IN-TEXT TABLES AND FIGURES ............................................................................................... -

Antiplatelet Effects of Prostacyclin Analogues: Which One to Choose in Case of Thrombosis Or Bleeding? Sylwester P
INTERVENTIONAL CARDIOLOGY Cardiology Journal 20XX, Vol. XX, No. X, XXX–XXX DOI: 10.5603/CJ.a2020.0164 Copyright © 20XX Via Medica REVIEW ARTICLE ISSN 1897–5593 eISSN 1898–018X Antiplatelet effects of prostacyclin analogues: Which one to choose in case of thrombosis or bleeding? Sylwester P. Rogula1*, Hubert M. Mutwil1*, Aleksandra Gąsecka1, Marcin Kurzyna2, Krzysztof J. Filipiak1 11st Chair and Department of Cardiology, Medical University of Warsaw, Poland 2Department of Pulmonary Circulation, Thromboembolic Diseases and Cardiology, Center of Postgraduate Education Medical, European Health Center Otwock, Poland Abstract Prostacyclin and analogues are successfully used in the treatment of pulmonary arterial hypertension (PAH) due to their vasodilatory effect on pulmonary arteries. Besides vasodilatory effect, prostacyclin analogues inhibit platelets, but their antiplatelet effect is not thoroughly established. The antiplatelet effect of prostacyclin analogues may be beneficial in case of increased risk of thromboembolic events, or undesirable in case of increased risk of bleeding. Since prostacyclin and analogues differ regarding their potency and form of administration, they might also inhibit platelets to a different extent. This review summarizes the recent evidence on the antiplatelet effects of prostacyclin and analogue in the treatment of PAH, this is important to consider when choosing the optimal treatment regimen in tailoring to an individual patients’ needs. (Cardiol J 20XX; XX, X: xx–xx) Key words: prostacyclin analogues, pulmonary arterial hypertension, platelets, antiplatelet effect, thrombosis, bleeding Introduction tiproliferative effects [4]. The main indication for PGI2 and analogues is advanced pulmonary arterial Since 1935 when prostaglandin was isolated hypertension (PAH) and peripheral vascular disor- for the first time [1], many scientists have focused ders [5].