Prevention and Control of Mycoplasma Contamination in Cell Cultures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mycoplasma Agalactiae MEMBRANE PROTEOME
UNIVERSITÀ DEGLI STUDI DI SASSARI SCUOLA DI DOTTORATO IN SCIENZE BIOMOLECOLARI E BIOTECNOLOGICHE INDIRIZZO MICROBIOLOGIA MOLECOLARE E CLINICA XXIII Ciclo CHARACTERIZATION OF Mycoplasma agalactiae MEMBRANE PROTEOME Direttore: Prof. Bruno Masala Tutor: Dr. Alberto Alberti Tesi di dottorato della Dott.ssa Carla Cacciotto ANNO ACCADEMICO 2009-2010 TABLE OF CONTENTS 1. Abstract 2. Introduction 2.1 Mycoplasmas: taxonomy and main biological features 2.2 Metabolism 2.3 In vitro cultivation 2.4 Mycoplasma lipoproteins 2.5 Invasivity and pathogenicity 2.6 Diagnosis of mycoplasmosis 2.7 Mycoplasma agalactiae and Contagious Agalactia 3. Research objectives 4. Materials and methods 4.1 Media and buffers 4.2 Bacterial strains and culture conditions 4.3 Total DNA extraction and PCR 4.4 Total proteins extraction 4.5 Triton X-114 fractionation 4.6 SDS-PAGE 4.7 Western immunoblotting 4.8 2-D PAGE 4.9 2D DIGE 4.10 Spot picking and in situ tryptic digestion 4.11 GeLC-MS/MS 4.12 MALDI-MS 4.13 LC-MS/MS 4.14 Data analysis Dott.ssa Carla Cacciotto, Characterization of Mycoplasma agalactiae membrane proteome. Tesi di Dottorato in Scienze Biomolecolari e Biotecnologiche, Università degli Studi di Sassari. 5. Results 5.1 Species identification 5.2 Extraction of bacterial proteins and isolation of liposoluble proteins 5.3 2-D PAGE/MS of M. agalactiae PG2T liposoluble proteins 5.4 2D DIGE of liposoluble proteins among the type strain and two field isolates of M. agalactiae 5.5 GeLC-MS/MS of M. agalactiae PG2T liposoluble proteins 5.6 Data analysis and classification 6. Discussion 7. -

( 12 ) United States Patent
US009956282B2 (12 ) United States Patent ( 10 ) Patent No. : US 9 ,956 , 282 B2 Cook et al. (45 ) Date of Patent: May 1 , 2018 ( 54 ) BACTERIAL COMPOSITIONS AND (58 ) Field of Classification Search METHODS OF USE THEREOF FOR None TREATMENT OF IMMUNE SYSTEM See application file for complete search history . DISORDERS ( 56 ) References Cited (71 ) Applicant : Seres Therapeutics , Inc. , Cambridge , U . S . PATENT DOCUMENTS MA (US ) 3 ,009 , 864 A 11 / 1961 Gordon - Aldterton et al . 3 , 228 , 838 A 1 / 1966 Rinfret (72 ) Inventors : David N . Cook , Brooklyn , NY (US ) ; 3 ,608 ,030 A 11/ 1971 Grant David Arthur Berry , Brookline, MA 4 ,077 , 227 A 3 / 1978 Larson 4 ,205 , 132 A 5 / 1980 Sandine (US ) ; Geoffrey von Maltzahn , Boston , 4 ,655 , 047 A 4 / 1987 Temple MA (US ) ; Matthew R . Henn , 4 ,689 ,226 A 8 / 1987 Nurmi Somerville , MA (US ) ; Han Zhang , 4 ,839 , 281 A 6 / 1989 Gorbach et al. Oakton , VA (US ); Brian Goodman , 5 , 196 , 205 A 3 / 1993 Borody 5 , 425 , 951 A 6 / 1995 Goodrich Boston , MA (US ) 5 ,436 , 002 A 7 / 1995 Payne 5 ,443 , 826 A 8 / 1995 Borody ( 73 ) Assignee : Seres Therapeutics , Inc. , Cambridge , 5 ,599 ,795 A 2 / 1997 McCann 5 . 648 , 206 A 7 / 1997 Goodrich MA (US ) 5 , 951 , 977 A 9 / 1999 Nisbet et al. 5 , 965 , 128 A 10 / 1999 Doyle et al. ( * ) Notice : Subject to any disclaimer , the term of this 6 ,589 , 771 B1 7 /2003 Marshall patent is extended or adjusted under 35 6 , 645 , 530 B1 . 11 /2003 Borody U . -

A Phylogenetic Analysis of the Mycoplasmas: Basis for Their Lc Assification W
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by DigitalCommons@University of Nebraska University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Public Health Resources Public Health Resources 9-1989 A Phylogenetic Analysis of the Mycoplasmas: Basis for Their lC assification W. G. Weisburg University of Illinois J. G. Tully National Institute of Allergy and Infectious Diseases D. L. Rose National Institute of Allergy and Infectious Diseases J. P. Petzel Iowa State University H. Oyaizu University of Illinois See next page for additional authors Follow this and additional works at: https://digitalcommons.unl.edu/publichealthresources Weisburg, W. G.; Tully, J. G.; Rose, D. L.; Petzel, J. P.; Oyaizu, H.; Yang, D.; Mandelco, L.; Sechrest, J.; Lawrence, T. G.; Van Etten, James L.; Maniloff, J.; and Woese, C. R., "A Phylogenetic Analysis of the Mycoplasmas: Basis for Their lC assification" (1989). Public Health Resources. 310. https://digitalcommons.unl.edu/publichealthresources/310 This Article is brought to you for free and open access by the Public Health Resources at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Public Health Resources by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Authors W. G. Weisburg, J. G. Tully, D. L. Rose, J. P. Petzel, H. Oyaizu, D. Yang, L. Mandelco, J. Sechrest, T. G. Lawrence, James L. Van Etten, J. Maniloff, and C. R. Woese This article is available at DigitalCommons@University of Nebraska - Lincoln: https://digitalcommons.unl.edu/ publichealthresources/310 JOURNAL OF BACTERIOLOGY, Dec. 1989, p. 6455-6467 Vol. 171, No. -

Invivogen Insight Newsletter: Mycoplasma
November/December 2005 An Insightful Look At InvivoGen’s Innovative Products Mycoplasma contamination remains a significant problem to Mycoplasma: The Insidious Invader of Cell Cultures the culture of mammalian cells. Mycoplasmas are the smallest and simplest and enzymatic procedures. However, none of these self-replicating organisms. Due to their seriously methods is 100% reliable. Direct growth methods are The detection of mycoplasma degraded genome they cannot perform many relatively sensitive to most species but the overall contamination is an important metabolic functions, such as cell wall production or procedure is lengthy (3 weeks), costly and less synthesis of nucleotides and amino acids. sensitive to noncultivable species. The PCR method, part of mycoplasma control and Mycoplasmas are strictly parasites. They parasitize a although rather fast and inexpensive, is limited by its should be an established wide range of organisms including humans, animals, sensitivity and the risk of positive and false negative method in every cell culture insects, and plants. results. Mycoplasma and Acholeplasma are Mollicutes, that InvivoGen has developed a new mycoplasma detection laboratory. InvivoGen is pleased comprise together more than 100 recognized species. method that promises to resolve these issues. This to introduce PlasmoTest™, a Among them, about 20 species have been described as method is based on the detection of mycoplasmas by contaminants of eukaryotic cell cultures. However engineered cells that express Toll-like receptor 2, a Mycoplasma detection kit based 5 species (Mycoplasma (M.) arginini, M. fermentans, pathogen recognition receptor that detects mycoplasmas. on a brand new technology. M. orale, M. hyorhinis and Acholeplasma laidlawii) PlasmoTest™, InvivoGen’s new mycoplasma detection are isolated in 90-95% of contaminated cell cultures1. -

Table S1. Proportional Abundance, and Absolute Abundance of Penile Bacteria from the 266 Men Included in the HIV Seroconversion Cohort
Table S1. Proportional abundance, and absolute abundance of penile bacteria from the 266 men included in the HIV Seroconversion Cohort. All men were uncircumcised. Proportional Abundance Absolute Abundance (16S copies/swab) Genus Median Q#1 Q#3 Median Q#1 Q#3 Prevotella 0.155 0.059 0.279 2.78E+07 9.78E+05 3.14E+08 Peptoniphilus 0.077 0.038 0.119 1.52E+07 1.66E+06 8.69E+07 Peptoniphilaceae<0.97*† 0.049 0.013 0.125 7.81E+06 2.97E+05 1.39E+08 Porphyromonas 0.032 0.010 0.067 4.47E+06 2.36E+05 9.88E+07 Finegoldia 0.029 0.005 0.104 3.37E+06 7.02E+05 2.07E+07 Corynebacterium 0.027 0.004 0.119 2.74E+06 7.12E+05 1.19E+07 Anaerococcus 0.025 0.008 0.061 4.38E+06 7.03E+05 2.10E+07 Dialister 0.018 0.002 0.045 1.76E+06 7.01E+04 3.40E+07 Lactobacillus 0.002 0.001 0.004 2.46E+05 3.33E+04 2.33E+06 Gardnerella 0.001 0.000 0.003 5.72E+04 9.27E+03 8.40E+05 Ezakiella 0.004 0.001 0.016 3.59E+05 2.59E+04 1.11E+07 Clostridiales incertae sedis XIII<0.97*† 0.003 0.000 0.010 3.80E+05 1.32E+04 1.10E+07 Mobiluncus 0.001 0.000 0.011 2.24E+05 1.18E+04 6.54E+06 Firmicutes<0.97*‡ 0.005 0.001 0.016 4.55E+05 1.76E+04 1.55E+07 Murdochiella 0.004 0.001 0.015 6.34E+05 2.70E+04 1.10E+07 Campylobacter 0.004 0.000 0.013 4.19E+05 1.69E+04 1.25E+07 Negativicoccus 0.003 0.000 0.018 3.83E+05 2.54E+04 6.11E+06 Saccharofermentans<0.97* 0.001 0.000 0.009 9.49E+04 7.09E+03 5.02E+06 Peptostreptococcus 0.004 0.000 0.027 2.13E+05 1.69E+04 1.38E+07 Proteobacteria<0.97*‡ 0.001 0.000 0.010 9.69E+04 7.26E+03 3.90E+06 Porphyromonas<0.97* 0.001 0.000 0.005 1.08E+05 4.03E+03 3.46E+06 Staphylococcus -

Microbiology Catalogue Contents
Microbiology catalogue Contents 3 About ATCC 4 About the ATCC / LGC Standards partnership 5 Quality control strains 7 Pharmaceutical applications 12 Food microbiology 20 Food microbiology, Genomic DNA 21 Water microbiology 24 Catalogue listing 38 Nucleic Acids prepared from ATCC Genuine Cultures® 39 Fully sequenced microbes 45 Microbial technical resource 61 Instructions for rehydrating freeze-dried cultures 63 ATCC MTA All care has been taken in the compilation of the information contained in this catalogue. However, any applications for products are suggestions only, and LGC Standards makes no express or implied representations or warranties regarding the accuracy, content, completeness, or reliability of the information or any suggestions provided, and specifically disclaims any and all implied warranties with respect to the same, including without limitation any warranties of merchantability, fitness or suitability for particular purpose. About ATCC Mission ATCC is a global nonprofit bioresource centre and ATCC is an independent, private, nonprofit research organisation that provides biological biological resource centre (BRC) and research products, technical services and educational organisation. programmes to private industry, government and academic organisations. The mission of As a biological resource centre, ATCC ATCC is to acquire, authenticate, preserve, authenticates microorganisms and cell lines and develop and distribute biological materials, manages logistics of long-term preservation information, technology, intellectual -

Mycoplasma Spermatophilum, a New Species Isolated from Human Spermatozoa and Cervix AURIOL C
INTERNATIONALJOURNAL OF SYSTEMATICBACTERIOLOGY, Apr. 1991, p. 229-233 Vol. 41, No. 2 0020-7713/91/020229-05$02.oo/o Copyright 0 1991, International Union of Microbiological Societies Mycoplasma spermatophilum, a New Species Isolated from Human Spermatozoa and Cervix AURIOL C. HILL Medical Research Council Toxicology Unit, Woodmansterne Road, Carshalton, Surrey SM5 4EF, United Kingdom A mycoplasma isolated from human spermatozoa and a human cervix was shown to be serologically distinct from 98 previously recognized MycopEasma and AchoZepZasma spp. Six mycoplasma colonies were cloned and examined in detail for morphology, growth, and biochemical characteristics; five of these were from sperm samples and one was from a cervix. These strains were closely related and had the following properties: guanine-plus-cytosine content of 32 mol%, requirement for sterol, and anaerobic growth. Glucose was not metabolized, and arginine and urea were not hydrolyzed. Strain AH159 (= NCTC 11720) is the type strain of a new species, Mycoplasma spermatophilum. Twelve named Mycoplasma and Acholeplasma species colony isolated from each patient was cloned to produce a have been isolated from the respiratory or genital tracts of pure culture; this was done by initially filtering a broth humans (6). Mycoplasma buccale, Mycoplasma faucium, culture through a 220-nm-pore-size membrane filter, cultur- Mycoplasma lipophilum , Mycoplasma orale, Mycoplasma ing the filtrate on solid medium, transferring a single result- pneumoniae, and Mycoplasma salivarium are found almost ing colony to another agar plate, and inoculating the subse- exclusively in respiratory tracts. Mycoplasma fermentans quent growth into broth. This whole procedure was repeated has been found infrequently in urogenital tracts, while My- an additional four times; thus, the organisms were filter coplasma primatum, a species commonly present in nonhu- cloned five times (29). -

United States Patent (19) 11 Patent Number: 5,824,479 Smida Et Al
O USOO5824479A United States Patent (19) 11 Patent Number: 5,824,479 Smida et al. 45) Date of Patent: Oct. 20, 1998 54 INTER-LINE-PCR Chemical Abstract, vol. 120, 1994, p. 326. Abstract No. 20:976646, 75 Inventors: Jan Smida, Freising; Stefan Leibhard, Chemical Abstract, vol. 118, 1993, p. 562, Abstract No. Oberschleissheim; Ludwig Hieber, 118:56972r. Kirchheim; F. Eckardt-Schupp, Frothingham et al. A PCR-Based Method of Identifying Pfaffenhofen, all of Germany Species-Specific Repeated DNAs, BioTechniques, vol. 13. No. 2, 1992, pp. 210, 212. 213. 73) Assignee: Forschungszentrum fur, Umwelt und Furano et al., Amplification of the Ancient Murine Lx Family Gesundheit GmbH. Oberschleissheim, of Long Interspersed Repeated DNA Occurred During the Germany Murine Radiation, J. Mol. Evol., vol. 38 (1994), pp. 18-27. Pascale et al. The Evolution of Long Interspersed Repeated (21) Appl. No.: 646,809 DNA (L1, LINE 1) as Revealed by the Analysis of an Ancient Rodent Ll DNA Family, J. Mol. Evol. (1993), vol. 36 ppi (22 Filed: May 21, 1996 9-20. 30 Foreign Application Priority Data Gong et al., COMMUNICATION Identification of Region Specific Cosmid Clones by Hybrodization with Pooled May 22, 1995 DEI Germany ........................ 19518769.5 Alu-LINE Polymerase Chain Reaction Products of Yeast (51) int. Cl. ................... C12Q 1/68; C12P 19/34; Artificial Chromosone Clones, Methods in Mol. and Cell. CO7H 21/04 Biol. (1994), 4:269-272. (52) U.S. Cl. ........................... 435/6; 536/24.3: 536/22.1; Laten and Morris. SIRE-1, a long interspersed repetitive 435/91.2 DNA element from soybean with weak sequence similarity to (58) Field of Search ................................. -

Rapid, Sensitive PCR-Based Detection of Mycoplasmas In
APPLIED AND ENVIRONMENTAL MICROBIOLOGY, Mar. 1994, p. 953-959 Vol. 60, No. 3 0099-2240/94/$04.00 +0 Copyright © 1994, American Society for Microbiology Rapid, Sensitive PCR-Based Detection of Mycoplasmas in Simulated Samples of Animal Sera OLIVIER DUSSURGET AND DAISY ROULLAND-DUSSOIX* Laboratoire des Mycoplasnes, Institut Pasteur, 75724 Paris Cedex 15, Franice Received 2 August 1993/Accepted 17 December 1993 A fast and simple method to detect mycoplasmal contamination in simulated samples of animal sera by using a PCR was developed. The following five mycoplasma species that are major cell culture contaminants belonging to the class Mollicutes were investigated: Mycoplasma arginini, Acholeplasma laidlawii, Mycoplasma hyorhinis, Mycoplasma orale, and Mycoplasma fermentans. After a concentration step involving seeded sera, genus-specific primers were used to amplify a 717-bp DNA fragment within the 16S rRNA gene of mycoplasmas. In a second step, the universal PCR was followed by amplification of variable regions of the 16S rRNA gene by using species-specific primers, which allowed identification of contaminant mycoplasmas. With this method, 10 fg of purified DNA and 1 to 10 color-changing units of mycoplasmas could be detected. Since the sensitivity of the assay was increased 10-fold when the amplification products were hybridized with an internal mycoplasma-specific 32P-labelled oligonucleotide probe, a detection limit of 1 to 10 genome copies per PCR sample was obtained. This highly sensitive, specific, and simple assay may be a useful alternative to methods currently used to detect mycoplasmas in animal sera. Mycoplasmas (the trivial name for microorganisms belong- Like most cell cultures infected by mycoplasmas, serum infec- ing to the class Molliclutes) are the smallest self-replicating tions are rarely detected by visual inspection or light micros- bacteria. -

D DFA Chlamydiae Culture Confirmation Kit and Three Currently Marketed Culture Green Fluorescent Inclusions Are Observed in the Infected Cells
using iodine, Giemsa, or fluorescein-conjugated monoclonal antibodies. The use of iodine and Giemsa has been shown to be less sensitive than the use of fluorescein- conjugated monoclonal antibodies.1 III. PRINCIPLE OF THE PROCEDURE 3 The Diagnostic Hybrids, Inc. D3 DFA Chlamydiae Culture Confirmation Kit uses a blend of two specific murine MAbs that are directly labeled with fluorescein isothiocyanate D DFA (FITC) for the qualitative detection of Chlamydiae in inoculated cell cultures. Cell culture isolation of Chlamydiae utilizes either McCoy cells, a mouse fibroblast cell line, or Buffalo Green Monkey Kidney (BGMK) cells in shell vial or multi-well plate Chlamydiae Culture formats. The cells are overlaid with a Chlamydia isolation medium containing cycloheximide to enhance Chlamydial growth prior to inoculation of the clinical specimen. The inoculated cells are centrifuged for 60 minutes and incubated at 35° to 37°C for 48 to 72 hours. The cells are fixed in acetone and the Chlamydiae DFA Confirmation Kit Reagent is added to the cells to stain any Chlamydiae specific antigens that may be present following culture. After incubating for 15 to 30 minutes at 35° to 37°C, the stained cells are washed with the supplied Phosphate Buffered Saline (PBS). A drop of REF: 01-040000 the supplied Mounting Fluid is added to the multi-wells or to a clean microscope slide for mounting a coverslip. The cells are examined at 100 to 400X magnification using a For in vitro Diagnostic Use microscope equipped with the correct filter combination for fluorescein. Chlamydiae Please contact Diagnostic HYBRIDS Technical Services USA Toll-free: (866) 344-3477 infected cells will have bright, apple-green fluorescent inclusions while non-infected for technical assistance regarding this procedure. -

Detection of a Novel Intracellular Microbiome Hosted in Arbuscular Mycorrhizal Fungi
The ISME Journal (2014) 8, 257–270 & 2014 International Society for Microbial Ecology All rights reserved 1751-7362/14 www.nature.com/ismej ORIGINAL ARTICLE Detection of a novel intracellular microbiome hosted in arbuscular mycorrhizal fungi Alessandro Desiro` 1, Alessandra Salvioli1, Eddy L Ngonkeu2, Stephen J Mondo3, Sara Epis4, Antonella Faccio5, Andres Kaech6, Teresa E Pawlowska3 and Paola Bonfante1 1Department of Life Sciences and Systems Biology, University of Torino, Torino, Italy; 2Institute of Agronomic Research for Development (IRAD), Yaounde´, Cameroon; 3Department of Plant Pathology and Plant Microbe-Biology, Cornell University, Ithaca, NY, USA; 4Department of Veterinary Science and Public Health, University of Milano, Milano, Italy; 5Institute of Plant Protection, UOS Torino, CNR, Torino, Italy and 6Center for Microscopy and Image Analysis, University of Zurich, Zurich, Switzerland Arbuscular mycorrhizal fungi (AMF) are important members of the plant microbiome. They are obligate biotrophs that colonize the roots of most land plants and enhance host nutrient acquisition. Many AMF themselves harbor endobacteria in their hyphae and spores. Two types of endobacteria are known in Glomeromycota: rod-shaped Gram-negative Candidatus Glomeribacter gigasporarum, CaGg, limited in distribution to members of the Gigasporaceae family, and coccoid Mollicutes-related endobacteria, Mre, widely distributed across different lineages of AMF. The goal of the present study is to investigate the patterns of distribution and coexistence of the two endosymbionts, CaGg and Mre, in spore samples of several strains of Gigaspora margarita. Based on previous observations, we hypothesized that some AMF could host populations of both endobacteria. To test this hypothesis, we performed an extensive investigation of both endosymbionts in G. -
Advances in PCR Based Detection of Mycoplasmas Contaminating Cell Cultures
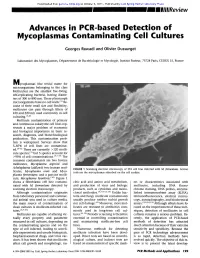
Downloaded from genome.cshlp.org on October 6, 2021 - Published by Cold Spring Harbor Laboratory Press Advances in PCR based Detection of Mycoplasmas Contaminating Cell Cultures Georges Rawadi and Olivier Dussurget Laboratoire des Mycoplasmes, D~partement de Bact&iologie et Mycologie, Institut Pasteur, 75724 Paris, CEDEX 15, France M ycoplasmas (the trivial name for microorganisms belonging to the class Mollicutes) are the smallest free-living, self-replicating bacteria, having diame- ters of 300 to 800 nm. These pleomorph microorganisms have no cell walls. (1~ Be- cause of their small size and flexibility, mollicutes can pass through filters of 450 and 220 nm used commonly in cell culturing. ~,2) Mollicute contamination of primary and continuous eukaryotic cell lines rep- resents a major problem of economic and biological importance in basic re- search, diagnosis, and biotechnological production. This contamination prob- lem is widespread. Surveys show that 5-87% of cell lines are contaminat- ed. (3-6~ There are currently ~120 molli- cute species, (~ but 5 species account for ~>95% of cell contaminations. (3'7-9~ The common contaminants are two bovine mollicutes, Mycoplasma arginini and Acholeplasma laidlawii; two human mol- FIGURE 1 Scanning electron microscopy of 3T6 cell line infected with M. fermentans. Arrows licutes, Mycoplasma orale and Myco- indicate the mycoplasmas adsorbed on the cell surface. plasma fermentans; and a porcine molli- cute, Mycoplasma hyorhinis. (1~ Figure 1 shows a fibroblastic cell line contami- cleic acid and amino acid metabolism, ers or characteristics associated with nated with M. fermentans detected by and production of virus and biologic mollicutes, including DNA fluoro- scanning electron microscopy.