New Concepts of Mycoplasma Pneumoniae Infections in Children
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antimicrobial Resistance and Disinfectants Susceptibility of Persistent Bacteria in a Tertiary Care Hospital
Journal of Microbiology and Antimicrobials Vol. 2(7), pp. xx-xx, October 2010 Available online http://www.academicjournals.org/JMA ISSN 2141-2308 ©2010 Academic Journals Full Length Research Paper Antimicrobial resistance and disinfectants susceptibility of persistent bacteria in a tertiary care hospital Maria Lucia Morcerf Bouzada1, Vania Lucia Silva1, Felipe Augusto Sa Moreira1, Girlene Alves Silva2 and Claudio Galuppo Diniz1* 1Department of Parasitology, Microbiology and Immunology, Laboratory of Bacterial Physiology and Molecular Genetics, Institute of Biological Sciences, Federal University of Juiz de Fora, Juiz de Fora/MG,36036-900, Brazil. 2Department of Applied Nursing, School of Nursing, Federal University of Juiz de Fora, Juiz de Fora/MG, 36036-900, Brazil. Accepted 22 October, 2010 It is well known that putative pathogenic bacteria are ubiquitous and widely distributed in the hospital environment. This study aimed to detect bacterial persistence in the nosocomial environment (different critical areas of the hospital) after mopping by the cleaning staff. Susceptibility patterns to antimicrobial drugs and disinfectants commonly used in health services were also investigated by disk diffusion and agar dilution tests. Rinse water from mops was processed for isolation of Enterobacteriaceae (GNR), non-fermenting Gram-negative rods (NFGNR), coagulase-negative staphylococci (CNS) and enterococci (ENT). Microorganisms were biochemically characterized and 547 strains were recovered. Only CNS and NFGNR were isolated in all critical areas. Overall 67% of the isolated bacteria were resistant to more than three drugs, being considered as multiresistant. Disinfectants were effective in concentrations ranging from 0.125 to 1%. Hospitals provide reservoirs of multiresistant microorganisms borne by patients and staff, but the hospital environment may be an important repository. -

Identification of Genes Involved in Acid Tolerance, Antimicrobial Resistance and Virulence of Enterococcus Faecium
Identification of genes involved in acid tolerance, antimicrobial resistance and virulence of Enterococcus faecium Thesis submitted by Hashimatul Fatma binti Hashim For the degree of DOCTOR OF PHILOSOPHY in the Faculty of Medical Sciences University College London Division of Microbial Diseases UCL Eastman Dental Institute 256 Gray’s Inn Road London WC1X 8LD UK 2016 Declaration I hereby certify that the work embodied in this thesis is the result of my own investigation, except where otherwise stated. 2 Abstract Enterococcus faecium is an opportunistic human nosocomial pathogen that has developed resistance to many existing antimicrobial therapies. Treatment of enterococcal infections is becoming increasingly challenging and there are limited therapeutic options against multidrug-resistant enterococci. The work described in this thesis aimed to identify genes involved in resistance to host stresses and virulence as these could potentially be future therapeutic targets. An E. faecium transposon mutant library was screened for altered resistance to lysozyme and to nisin as a model antimicrobial peptide. This approach led to the identification of several genes that contribute to lysozyme and nisin resistance. A number of mutants that were sensitive to nisin had a transposon insertion in a gene predicted to encode a tyrosine decarboxylase. It was shown that the tyrosine decarboxylase plays a role in acid tolerance and mediates virulence of E. faecium in a Galleria mellonella larvae infection model. A targeted genetic approach was used to examine the role of an E. faecium serine threonine protein kinase (Stk1) in antimicrobials resistance, host cell stresses and virulence. Disruption of the stk1 gene led to higher sensitivity to antibiotics that target the penicillin- binding proteins and bile salts compared to the wild type. -
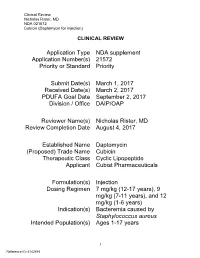
Clinical Review Nicholas Rister, MD NDA 021572 Cubicin (Daptomycin for Injection)
Clinical Review Nicholas Rister, MD NDA 021572 Cubicin (Daptomycin for injection) CLINICAL REVIEW Application Type NDA supplement Application Number(s) 21572 Priority or Standard Priority Submit Date(s) March 1, 2017 Received Date(s) March 2, 2017 PDUFA Goal Date September 2, 2017 Division / Office DAIP/OAP Reviewer Name(s) Nicholas Rister, MD Review Completion Date August 4, 2017 Established Name Daptomycin (Proposed) Trade Name Cubicin Therapeutic Class Cyclic Lipopeptide Applicant Cubist Pharmaceuticals Formulation(s) Injection Dosing Regimen 7 mg/kg (12-17 years), 9 mg/kg (7-11 years), and 12 mg/kg (1-6 years) Indication(s) Bacteremia caused by Staphylococcus aureus Intended Population(s) Ages 1-17 years 1 Reference ID: 4142515 Clinical Review Nicholas Rister, MD NDA 021572 Cubicin (Daptomycin for injection) Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT ......................................... 7 1.1 Recommendation on Regulatory Action ............................................................. 7 1.2 Risk Benefit Assessment .................................................................................... 7 1.3 Recommendations for Postmarket Risk Evaluation and Mitigation Strategies ... 8 1.4 Recommendations for Postmarket Requirements and Commitments ................ 8 2 INTRODUCTION AND REGULATORY BACKGROUND ........................................ 8 2.1 Product Information ............................................................................................ 8 2.2 Tables of Currently Available Treatments -

Calves Infected with Virulent and Attenuated Mycoplasma Bovis Strains Have Upregulated Th17 Inflammatory and Th1 Protective Responses, Respectively
G C A T T A C G G C A T genes Article Calves Infected with Virulent and Attenuated Mycoplasma bovis Strains Have Upregulated Th17 Inflammatory and Th1 Protective Responses, Respectively Jin Chao 1,2,3,4, Xiaoxiao Han 1,2, Kai Liu 1,2, Qingni Li 1,2, Qingjie Peng 5, Siyi Lu 1,2, Gang Zhao 1,2, Xifang Zhu 1,2, Guyue Hu 1,2, Yaqi Dong 1,2, Changmin Hu 2, Yingyu Chen 1,2, Jianguo Chen 2, Farhan Anwar Khan 1, Huanchun Chen 1,2,3,4 and Aizhen Guo 1,2,3,4,* 1 The State Key Laboratory of Agricultural Microbiology, Huazhong Agricultural University, Wuhan 430070, China 2 College of Veterinary Medicine, Huazhong Agricultural University, Wuhan 430070, China 3 Hubei International Scientific and Technological Cooperation Base of Veterinary Epidemiology, Huazhong Agricultural University, Wuhan 430070, China 4 Key Laboratory of Development of Veterinary Diagnostic Products, Ministry of Agriculture, Huazhong Agricultural University, Wuhan 430070, China 5 Wuhan Keqian Biology Ltd., Wuhan 430223, China * Correspondence: [email protected]; Tel.: +86-27-8728-6861 Received: 15 June 2019; Accepted: 27 August 2019; Published: 28 August 2019 Abstract: Mycoplasma bovis is a critical bovine pathogen, but its pathogenesis remains poorly understood. Here, the virulent HB0801 (P1) and attenuated HB0801-P150 (P150) strains of M. bovis were used to explore the potential pathogenesis and effect of induced immunity from calves’ differential transcriptomes post infection. Nine one-month-old male calves were infected with P1, P150, or mock-infected with medium and euthanized at 60 days post-infection. -

Role of Protein Phosphorylation in Mycoplasma Pneumoniae
Pathogenicity of a minimal organism: Role of protein phosphorylation in Mycoplasma pneumoniae Dissertation zur Erlangung des mathematisch-naturwissenschaftlichen Doktorgrades „Doctor rerum naturalium“ der Georg-August-Universität Göttingen vorgelegt von Sebastian Schmidl aus Bad Hersfeld Göttingen 2010 Mitglieder des Betreuungsausschusses: Referent: Prof. Dr. Jörg Stülke Koreferent: PD Dr. Michael Hoppert Tag der mündlichen Prüfung: 02.11.2010 “Everything should be made as simple as possible, but not simpler.” (Albert Einstein) Danksagung Zunächst möchte ich mich bei Prof. Dr. Jörg Stülke für die Ermöglichung dieser Doktorarbeit bedanken. Nicht zuletzt durch seine freundliche und engagierte Betreuung hat mir die Zeit viel Freude bereitet. Des Weiteren hat er mir alle Freiheiten zur Verwirklichung meiner eigenen Ideen gelassen, was ich sehr zu schätzen weiß. Für die Übernahme des Korreferates danke ich PD Dr. Michael Hoppert sowie Prof. Dr. Heinz Neumann, PD Dr. Boris Görke, PD Dr. Rolf Daniel und Prof. Dr. Botho Bowien für das Mitwirken im Thesis-Komitee. Der Studienstiftung des deutschen Volkes gilt ein besonderer Dank für die finanzielle Unterstützung dieser Arbeit, durch die es mir unter anderem auch möglich war, an Tagungen in fernen Ländern teilzunehmen. Prof. Dr. Michael Hecker und der Gruppe von Dr. Dörte Becher (Universität Greifswald) danke ich für die freundliche Zusammenarbeit bei der Durchführung von zahlreichen Proteomics-Experimenten. Ein ganz besonderer Dank geht dabei an Katrin Gronau, die mich in die Feinheiten der 2D-Gelelektrophorese eingeführt hat. Außerdem möchte ich mich bei Andreas Otto für die zahlreichen Proteinidentifikationen in den letzten Monaten bedanken. Nicht zu vergessen ist auch meine zweite Außenstelle an der Universität in Barcelona. Dr. Maria Lluch-Senar und Dr. -

Mycoplasma Agalactiae MEMBRANE PROTEOME
UNIVERSITÀ DEGLI STUDI DI SASSARI SCUOLA DI DOTTORATO IN SCIENZE BIOMOLECOLARI E BIOTECNOLOGICHE INDIRIZZO MICROBIOLOGIA MOLECOLARE E CLINICA XXIII Ciclo CHARACTERIZATION OF Mycoplasma agalactiae MEMBRANE PROTEOME Direttore: Prof. Bruno Masala Tutor: Dr. Alberto Alberti Tesi di dottorato della Dott.ssa Carla Cacciotto ANNO ACCADEMICO 2009-2010 TABLE OF CONTENTS 1. Abstract 2. Introduction 2.1 Mycoplasmas: taxonomy and main biological features 2.2 Metabolism 2.3 In vitro cultivation 2.4 Mycoplasma lipoproteins 2.5 Invasivity and pathogenicity 2.6 Diagnosis of mycoplasmosis 2.7 Mycoplasma agalactiae and Contagious Agalactia 3. Research objectives 4. Materials and methods 4.1 Media and buffers 4.2 Bacterial strains and culture conditions 4.3 Total DNA extraction and PCR 4.4 Total proteins extraction 4.5 Triton X-114 fractionation 4.6 SDS-PAGE 4.7 Western immunoblotting 4.8 2-D PAGE 4.9 2D DIGE 4.10 Spot picking and in situ tryptic digestion 4.11 GeLC-MS/MS 4.12 MALDI-MS 4.13 LC-MS/MS 4.14 Data analysis Dott.ssa Carla Cacciotto, Characterization of Mycoplasma agalactiae membrane proteome. Tesi di Dottorato in Scienze Biomolecolari e Biotecnologiche, Università degli Studi di Sassari. 5. Results 5.1 Species identification 5.2 Extraction of bacterial proteins and isolation of liposoluble proteins 5.3 2-D PAGE/MS of M. agalactiae PG2T liposoluble proteins 5.4 2D DIGE of liposoluble proteins among the type strain and two field isolates of M. agalactiae 5.5 GeLC-MS/MS of M. agalactiae PG2T liposoluble proteins 5.6 Data analysis and classification 6. Discussion 7. -

Mycoplasma Orale “Types” 2 and 3, Respectively E
INTERNATIONAL JOURNAL of SYSTEMATIC BACTERIOLOGY Vol. 24, No. 2 April 1974, p. 252-255 Printed in U.S.A. Copyright 0 1974 International Association of Microbiological Societies Proposal of Mycoplasma buccale nom. nov. and Mycoplasmafaucium nom. nov. for Mycoplasma orale “Types” 2 and 3, Respectively E. A. FREUNDT, D. TAYLOR-ROBINSON, R. H. PURCELL, R. M. CHANOCK, and F. T. BLACK Institute of Medical Microbiology, University of Aarhus, Aarhus, Denmark; MRC Clinical Research Centre, Harrow, Middlesex, England; and Laboratory of Infectious Diseases, National Institute of Allergy and Infectious Diseases, Bethesda, Maryland 20014 Following recommendations made by the Subcommittee on the Taxonomy of Mycoplasrnatales of the International Committee on Systematic Bacteriology, it is proposed that Mycoplasma orale 2 and Mycoplasrna orale 3 be recognized as two separate species, Mycoplasrna buccale nom. nov. (type strain: CH20247; ATCC 23636) and Mycoplasrna fauciurn nom. nov. (type strain: DC-333; ATCC 25293), respectively. The general properties and distinctive characteristics of the newly named species are summarized. At present, three “types” of Mycoplasrna (22) be recognized as a species under the new orale are recognized: M. orale 1 Taylor- name Mycoplasrna buccale (L. adj. buccalis Robinson et al. 1964 (21), M. orale 2 Taylor- buccal), and (ii) Mycoplasrna orale 3 Fox et al. Robinson et al. 1965 (22), and M. orale 3 Fox 1969 (7) be recognized as a species under the et al. 1969 (7). However, the authors who new name Mycoplasma fauciurn (L. noun described the latter two “types” or “serotypes” fauces the throat; L. gen. pl. noun fauciurn of did, in fact, regard them as distinct new species throats). -

(12) United States Patent (10) Patent No.: US 8,835,117 B2 Mitchell Et Al
US008835117B2 (12) United States Patent (10) Patent No.: US 8,835,117 B2 Mitchell et al. (45) Date of Patent: Sep. 16, 2014 (54) NUCLEICACIDS FOR DETECTION AND OTHER PUBLICATIONS DISCRIMINATION OF GENOTYPES OF CHLAMYDOPHILA PSITTAC Nazarenko, I. Methods in Molecular Biology (2006) 335: 95-114.* Jeffrey et al. Microbiology (2007) 153: 2679-2688.* 75) Inventors: Stephaniep L. Mitchell, Somerville, MA Geens et al. Journal of Clinical Microbiology (2005) 43(5): 2456 (US); Jonas M. Winchell, Lilburn, GA 2461. (US) Geens et al., “Development of a Chlamydophila psittaci species specific and genotype-specific real-time PCR.” Vet. Res., 36: 787 (73) Assignee: The United States of America as 797, 2005. represented by the Secretary of the Geens et al., “Sequencing of the Chlamydophila psittaci OmpA Gene Department of Health and Human Reveals a New Genotype, E/B, and the Need for a Rapid Discrimi Services, Centers for Disease Control natory Genotyping Method.” J. Clin. Microbiol. 43(5): 2456-2461, and Prevention, Washington, DC (US) 2005. Heddema, “Genotyping of Chlamydophila psittaci in Human (*) Notice: Subject to any disclaimer, the term of this Samples.” Emerging Infectious Diseases, 12(12): 1989-1990, 2006. patent is extended or adjusted under 35 Menard, “Development of a real-time PCR for the detection of U.S.C. 154(b) by 82 days. Chlamydia psittaci,” J. Med. Microbiol. 55(Pt. 4): 471-473, 2006. Mitchellet al., “Genotyping of Chlamydophilapsittaci by Real-Time (21) Appl. No.: 13/322,787 PCR and High-Resolution Melt Analysis,” Journal of Clinical Microbiology, 47(1): 175-181, 2009. (22) PCT Filed: May 28, 2010 Sachse et al., “Genotyping of Chlamydophila psittaci using a new DNA microarray assay based on sequence analysis of ompA genes.” (86). -

Mycoplasma Pneumoniae Terminal Organelle
MYCOPLASMA PNEUMONIAE TERMINAL ORGANELLE DEVELOPMENT AND GLIDING MOTILITY by BENJAMIN MICHAEL HASSELBRING (Under the Direction of Duncan Charles Krause) ABSTRACT With a minimal genome containing less than 700 open reading frames and a cell volume < 10% of that of model prokaryotes, Mycoplasma pneumoniae is considered among the smallest and simplest organisms capable of self-replication. And yet, this unique wall-less bacterium exhibits a remarkable level of cellular complexity with a dynamic cytoskeleton and a morphological asymmetry highlighted by a polar, membrane-bound terminal organelle containing an elaborate macromolecular core. The M. pneumoniae terminal organelle functions in distinct, and seemingly disparate cellular processes that include cytadherence, cell division, and presumably gliding motility, as individual cells translocate over surfaces with the cell pole harboring the structure engaged as the leading end. While recent years have witnessed a dramatic increase in the knowledge of protein interactions required for core stability and adhesin trafficking, the mechanism of M. pneumoniae gliding has not been defined nor have interdependencies between the various terminal organelle functions been assessed. The studies presented in the current volume describe the first genetic and molecular investigations into the location, components, architecture, and regulation of the M. pneumoniae gliding machinery. The data indicate that cytadherence and gliding motility are separable properties, and identify a subset of M. pneumoniae proteins contributing directly to the latter process. Characterizations of novel gliding-deficient mutants confirm that the terminal organelle contains the molecular gliding machinery, revealing that with the loss of a single terminal organelle cytoskeletal element, protein P41, terminal organelles detach from the cell body but retain gliding function. -

Comparison of the Effectiveness of Penicillin and Broad-Spectrum Β-Lactam Antibiotics in the Treatment of Community-Acquired Pneumonia in Children
Clinical research Comparison of the effectiveness of penicillin and broad-spectrum β-lactam antibiotics in the treatment of community-acquired pneumonia in children Vojko Berce1, Maja Tomazin1, Erika Jerele2, Maša Cugmas2, Maša Berce3, Mario Gorenjak2 1Department of Pediatrics, University Medical Centre, Maribor, Slovenia Corresponding author: 2Department of Pediatrics, Faculty of Medicine, University of Maribor, Maribor, Slovenia Assist. Prof. Vojko Berce MD, 3 Section of Dental Medicine, Faculty of Medicine, University of Ljubljana, Ljubljana, PhD Slovenia Department of Pediatrics University Medical Centre Submitted: 5 April 2020 Maribor, Slovenia Accepted: 16 July 2020 Phone: +38 631870834 E-mail: vojko.berce@guest. Arch Med Sci arnes.si DOI: https://doi.org/10.5114/aoms.2020.98198 Copyright © 2020 Termedia & Banach Abstract Introduction: Bacterial community-acquired pneumonia (CAP) in children is caused mostly by Streptococcus pneumoniae. The resistance of pneumococci to penicillin is increasing. However, most guidelines still prefer treatment with narrow-spectrum antibiotics. Therefore, we compared the effect of in- travenous treatment with penicillin and broad-spectrum β-lactam antibiot- ics in children with CAP. The objective of our study was to assess the eligi- bility of treatment of bacterial CAP with intravenous penicillin. Material and methods: We performed a prospective study and included 136 children hospitalised because of bacterial CAP. Patients were treated in- travenously with either penicillin G or broad-spectrum β-lactam antibiotic monotherapy. Lung ultrasound and blood tests were performed at admis- sion and after 2 days of treatment. The time interval from the application of antibiotics to permanent defervescence was recorded. Results: Eighty-seven (64.0%) patients were treated with penicillin G, and 49 (36.0%) were treated with broad-spectrum β-lactam antibiotics. -

Chlamydia Trachomatis and Genital Mycoplasmas: Pathogens with an Impact on Human Reproductive Health
Hindawi Publishing Corporation Journal of Pathogens Volume 2014, Article ID 183167, 15 pages http://dx.doi.org/10.1155/2014/183167 Review Article Chlamydia trachomatis and Genital Mycoplasmas: Pathogens with an Impact on Human Reproductive Health SunIanica Ljubin-Sternak1 and Tomislav MeštroviT2 1 Teaching Institute of Public Health “Dr Andrija Stampar”ˇ and School of Medicine, University of Zagreb, Salataˇ 3b, 10000 Zagreb, Croatia 2Clinical Microbiology and Parasitology Unit, Polyclinic “Dr Zora Profozi´c”, Bosutska 19, 10000 Zagreb, Croatia Correspondence should be addressed to Suncanicaˇ Ljubin-Sternak; [email protected] Received 29 September 2014; Revised 9 December 2014; Accepted 11 December 2014; Published 31 December 2014 Academic Editor: Nongnuch Vanittanakom Copyright © 2014 S. Ljubin-Sternak and T. Meˇstrovic.´ This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The most prevalent, curable sexually important diseases are those caused by Chlamydia trachomatis (C. trachomatis) and genital mycoplasmas. An important characteristic of these infections is their ability to cause long-term sequels in upper genital tract, thus potentially affecting the reproductive health in both sexes. Pelvic inflammatory disease (PID), tubal factor infertility (TFI), and ectopic pregnancy (EP) are well documented complications of C. trachomatis infection in women. The role of genital mycoplasmas in development of PID, TFI, and EP requires further evaluation, but growing evidence supports a significant role for these in the pathogenesis of chorioamnionitis, premature membrane rupture, and preterm labor in pregnant woman. Both C. trachomatis and genital mycoplasmas can affect the quality of sperm and possibly influence the fertility of men. -

Comparative Radiographic Features of Community Acquired Legionnaires' Disease, Pneumococcal Pneumonia, Mycoplasma Pneumonia, and Psittacosis
Thorax: first published as 10.1136/thx.39.1.28 on 1 January 1984. Downloaded from Thorax 1984;39:28-33 Comparative radiographic features of community acquired legionnaires' disease, pneumococcal pneumonia, mycoplasma pneumonia, and psittacosis JT MACFARLANE, AC MILLER, WH RODERICK SMITH, AH MORRIS, DH ROSE From the Departments of Thoracic Medicine and Radiology, City Hospital, Nottingham ABSTRACT The features of the chest radiographs of 49 adults with legionnaires' disease were compared with those of 91 adults with pneumococcal pneumonia (31 of whom had bacteraemia or antigenaemia), 46 with mycoplasma pneumonia, and 10 with psittacosis pneumonia. No distinctive pattern was seen for any group. Homogeneous shadowing was more frequent in legionnaires' disease (40/49 cases) (p < 0.005), bacteraemic pneumococcal pneumonia (25/31) (p < 0.01) and non-bacteraemic pneumococcal pneumonia (42/60) (p < 0.05) than in myco- plasma pneumonia (23/46). Multilobe disease at presentation was commoner in bacteraemic pneumococcal pneumonia (20/31) than in non-bacteraemic pneumococcal pneumonia (15/60) (p < 0.001) or legionnaires' disease (19/49) (p < 0.025). In bacteraemic pneumococcal pneumonia multilobe disease at presentation was associated with increased mortality. Pleural effusions and some degree of lung collapse were seen in all groups, although effusions were commoner in bacteraemic pneumococcal pneumonia. Cavitation was unusual. Lymphadenopathy occurred only in mycoplasma pneumonia (10/46). Radiographic deterioration was particularly a feature of legionnaires' disease (30/46) and bacteraemic pneumococcal pneumonia (14/27), and these groups also showed slow radiographic resolution in survivors. Radiographic resolution was fastest with mycoplasma pneumonia; psittacosis and non-bacteraemic pneumococcal pneumonia http://thorax.bmj.com/ cleared at an intermediate rate.