Methicillin Resistant Staphylococcus Aureus Beta-Lactam Drugs, but Not Others
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Family Practice
THE JOURNAL OF FAMILY ONLINE EXCLUSIVE PRACTICE Paul K. Carlton, Jr, MD, Brown recluse spider bite? FACS The Texas A&M University Consider this uniquely Health Science Center College Station, Tex conservative treatment [email protected] An antihistamine and observation work as well— and often better—than more intensive therapies. Practice recommendations oped it in 4 phases, which I describe in • Be concerned about brown recluse this article. Not only does this conser- envenomation when a patient vative approach consistently heal con- reports intensifying localized firmed brown recluse bite wounds, but pain disproportionate to physical should a bite be mistakenly attributed findings after a “bite” (C). to the brown recluse (or one of its rela- tives in the Loxosceles genus of spider), • Prescribe an oral antihistamine there is no harm to the patient, nor any alone to control symptoms, even big expense. with a necrotic wound, and mark the IN THIS ARTICLE patient’s progress over 24 hours (C). z Spider bite z Is a brown recluse • If the patient improves dramatically, to blame? or MRSA? continue the antihistamine; with little Due to limited experience among the Page E6 or no improvement, consider giving an wider medical community in identifying antibiotic with the antihistamine (C). spider envenomation,1-4 bite recognition and selection of appropriate therapy can Strength of recommendation (SOR) be difficult. A Good-quality patient-oriented evidence Early findings can be confusing. B Inconsistent or limited-quality patient-oriented evidence C Consensus, usual practice, opinion, disease-oriented Brown recluse bites typically feel like a evidence, case series pin prick. -

Drug-Resistant Streptococcus Pneumoniae and Methicillin
NEWS & NOTES Conference Summary pneumoniae can vary among popula- conference sessions was that statically tions and is influenced by local pre- sound methods of data collection that Drug-resistant scribing practices and the prevalence capture valid, meaningful, and useful of resistant clones. Conference pre- data and meet the financial restric- Streptococcus senters discussed the role of surveil- tions of state budgets are indicated. pneumoniae and lance in raising awareness of the Active, population-based surveil- Methicillin- resistance problem and in monitoring lance for collecting relevant isolates is the effectiveness of prevention and considered the standard criterion. resistant control programs. National- and state- Unfortunately, this type of surveil- Staphylococcus level epidemiologists discussed the lance is labor-intensive and costly, aureus benefits of including state-level sur- making it an impractical choice for 1 veillance data with appropriate antibi- many states. The challenges of isolate Surveillance otic use programs designed to address collection, packaging and transport, The Centers for Disease Control the antibiotic prescribing practices of data collection, and analysis may and Prevention (CDC) convened a clinicians. The potential for local sur- place an unacceptable workload on conference on March 12–13, 2003, in veillance to provide information on laboratory and epidemiology person- Atlanta, Georgia, to discuss improv- the impact of a new pneumococcal nel. ing state-based surveillance of drug- vaccine for children was also exam- Epidemiologists from several state resistant Streptococcus pneumoniae ined; the vaccine has been shown to health departments that have elected (DRSP) and methicillin-resistant reduce infections caused by resistance to implement enhanced antimicrobial Staphylococcus aureus (MRSA). -

Detection of the Meca Gene and Identification of Staphylococcus
braz j infect dis 2 0 1 8;2 2(2):99–105 The Brazilian Journal of INFECTIOUS DISEASES www.elsevier.com/locate/bjid Original article Detection of the mecA gene and identification of Staphylococcus directly from blood culture bottles by multiplex polymerase chain reaction a,b,∗ a Taisa Trevizani Rocchetti , Katheryne Benini Martins , a c Patricia Yoshida Faccioli Martins , Rogério Antonio de Oliveira , d b Alessandro Lia Mondelli , Carlos Magno Castelo Branco Fortaleza , a Maria de Lourdes Ribeiro de Souza da Cunha a UNESP - Univ Estadual Paulista, Instituto de Biociências de Botucatu, Departamento de Microbiologia e Imunologia, Botucatu, SP, Brazil b UNESP - Univ Estadual Paulista, Faculdade de Medicina de Botucatu, Hospital Universitário, Departamento de Doenc¸as Tropicais, Botucatu, SP, Brazil c UNESP - Univ Estadual Paulista, Instituto de Biociências de Botucatu, Departamento de Biociência, Botucatu, SP, Brazil d UNESP - Univ Estadual Paulista, Faculdade de Medicina de Botucatu, Hospital Universitário, Departamento de Medicina Interna, Botucatu, SP, Brazil a r t i c l e i n f o a b s t r a c t Article history: Introduction: Staphylococcus spp. – both S. aureus, including methicillin-resistant strains Received 3 November 2017 (MRSA) and coagulase negative staphylococci (CoNS) – are relevant agents of healthcare- Accepted 18 February 2018 associated infections. Therefore, the rapid recognition of MRSA and methicillin-resistant Available online 13 March 2018 CoNS from blood stream infections is critically important for patient management. It is worth noting that inappropriate empiric therapy has been associated with higher in-hospital Keywords: mortality. Material and methods: In this study we evaluated a multiplex polymerase chain reaction (mul- Staphylococcus spp. -

The Oral and Conjunctival Microbiotas in Cats with and Without Feline
The oral and conjunctival microbiotas in cats with and without feline immunodeficiency virus infection Scott J Weese, Jamieson Nichols, Mohammad Jalali, Annette Litster To cite this version: Scott J Weese, Jamieson Nichols, Mohammad Jalali, Annette Litster. The oral and conjunctival microbiotas in cats with and without feline immunodeficiency virus infection. Veterinary Research, BioMed Central, 2015, 46 (1), pp.21. 10.1186/s13567-014-0140-5. hal-01290670 HAL Id: hal-01290670 https://hal.archives-ouvertes.fr/hal-01290670 Submitted on 18 Mar 2016 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Weese et al. Veterinary Research (2015) 46:21 DOI 10.1186/s13567-014-0140-5 VETERINARY RESEARCH RESEARCH Open Access The oral and conjunctival microbiotas in cats with and without feline immunodeficiency virus infection Scott J Weese1*, Jamieson Nichols2, Mohammad Jalali1 and Annette Litster2 Abstract The oral and conjunctival microbiotas likely play important roles in protection from opportunistic infections, while also being the source of potential pathogens. Yet, there has been limited investigation in cats, and the impact of comorbidities such as feline immunodeficiency virus (FIV) infection has not been reported. Oral and conjunctival swabs were collected from cats with FIV infection and FIV-uninfected controls, and subjected to 16S rRNA gene (V4) PCR and next generation sequencing. -

What Is Staphylococcus Aureus (Staph)?
What is Staphylococcus aureus (staph)? Staphylococcus aureus, often referred to simply as "staph," are bacteria commonly carried on the skin or in the nose of healthy people. Approximately 25% to 30% of the population is colonized (when bacteria are present, but not causing an infection) in the nose with staph bacteria. Sometimes, staph can cause an infection. Staph bacteria are one of the most common causes of skin infections in the United States. Most of these skin infections are minor (such as pimples and boils) and can be treated without antibiotics (also known as antimicrobials or antibacterials). However, staph bacteria also can cause serious infections (such as surgical wound infections, bloodstream infections, and pneumonia). What is MRSA (methicillin-resistant Staphylococcus aureus)? Some staph bacteria are resistant to antibiotics. MRSA is a type of staph that is resistant to antibiotics called beta-lactams. Beta-lactam antibiotics include methicillin and other more common antibiotics such as oxacillin, penicillin and amoxicillin. While 25% to 30% of the population is colonized with staph, approximately 1% is colonized with MRSA. Who gets staph or MRSA infections? Staph infections, including MRSA, occur most frequently among persons in hospitals and healthcare facilities (such as nursing homes and dialysis centers) who have weakened immune systems. These healthcare-associated staph infections include surgical wound infections, urinary tract infections, bloodstream infections, and pneumonia. Are people who are positive for the human immune deficiency virus (HIV) at increased risk for MRSA? Should they be taking special precautions? People with weakened immune systems, which include some patients with HIV infection, may be at risk for more severe illness if they get infected with MRSA. -

Emergence of Oxacillin-Resistant Staphylococcus Lugdunensis
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Journal of Microbiology, Immunology and Infection (2016) 49, 885e891 Available online at www.sciencedirect.com ScienceDirect journal homepage: www.e-jmii.com ORIGINAL ARTICLE Emergence of oxacillin-resistant Staphylococcus lugdunensis carrying staphylococcal cassette chromosome mec type V in central Taiwan Ting-Yu Yen a,b,g, Yun-Ju Sung c,g, Hsiao-Chuan Lin a,b, Ching-Tien Peng a,b, Ni Tien c, Kao-Pin Hwang a,b, Jang-Jih Lu d,e,f,* a Department of Pediatrics, Children’s Hospital, China Medical University Hospital, Taichung, Taiwan b School of Medicine, China Medical University, Taichung, Taiwan c Department of Laboratory Medicine, China Medical University Hospital, Taichung, Taiwan d Department of Medical Research, China Medical University Hospital, Taichung, Taiwan e Department of Laboratory Medicine, Chang Gung Memorial Hospital at Linkou, Taoyuan, Taiwan f Department of Medical Biotechnology and Laboratory Science, Chang Gung University, Kwei-Shan, Taoyuan, Taiwan Received 5 August 2014; received in revised form 12 November 2014; accepted 29 November 2014 Available online 11 December 2014 KEYWORDS Background: Staphylococcus lugdunensis has emerged as a key pathogen for clinical infection. coagulase-negative It is sensitive to most antistaphylococcal agents, but it is increasingly resistant to b-lactam an- staphylococcus; tibiotics. Oxacillin-resistant S. lugdunensis isolates carrying the mecA gene pose a major oxacillin resistance; concern for therapy failure. SCCmec gene; Methods: To assess the epidemiology and presence of mecA in S. lugdunensis, we gauged the Staphylococcus prevalence and antibiotic resistance of S. -
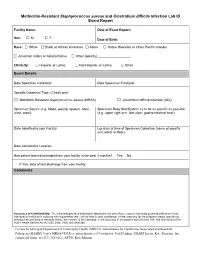
Methicillin-Resistant Staphylococcus Aureus and Clostridium Difficile Infection Lab ID Event Report
Methicillin-Resistant Staphylococcus aureus and Clostridium difficile Infection Lab ID Event Report Facility Name: Date of Event Report: Sex: M F □ □ Date of Birth: Race: □ White □ Black or African American □ Asian □ Native Hawaiian or Other Pacific Islander □ American Indian or Alaska Native □ Other [specify] __________________ Ethnicity: □ Hispanic or Latino □ Not Hispanic or Latino □ Other Event Details Date Specimen Collected: Date Specimen Finalized: Specific Organism Type: (Check one) □ Methicillin-Resistant Staphylococcus aureus (MRSA) □ Clostridium difficile Infection (CDI) Specimen Source (e.g. blood, wound, sputum, bone, Specimen Body Site/System try to be as specific as possible urine, stool): (e.g. upper right arm, foot ulcer, gastrointestinal tract): Date Admitted to your Facility: Location at time of Specimen Collection (name of specific unit, ward, or floor): Date Admitted to Location: Has patient been discharged from your facility in the past 3 months? Yes No If Yes, date of last discharge from your facility: Comments Assurance of Confidentiality: The voluntarily provided information obtained in this surveillance system that would permit identification of any individual or institution is collected with a guarantee that it will be held in strict confidence, will be used only for the purposes stated, and will not otherwise be disclosed or released without the consent of the individual, or the institution in accordance with Sections 304, 306 and 308(d) of the Public Health Service Act (42 USC 242b, 242k, and 242m(d)). For use by Michigan Department of Community Health (MDCH), Surveillance for Healthcare-Associated and Resistant Pathogens (SHARP) Unit’s MRSA/CDI Prevention Initiative (Coordinator: Gail Denkins, SHARP Intern: Kate Manton); fax completed forms to (517) 335-8263, ATTN: Kate Manton. -

Biodegradability of Woody Film Produced by Solvent Volatilisation Of
www.nature.com/scientificreports OPEN Biodegradability of woody flm produced by solvent volatilisation of Japanese Beech solution Yuri Nishiwaki-Akine1*, Sui Kanazawa2, Norihisa Matsuura3 & Ryoko Yamamoto-Ikemoto3 To address the problem of marine pollution from discarded plastics, we developed a highly biodegradable woody flm, with almost the same components as wood, from the formic acid solution of ball-milled wood. We found that the woody flm was not easily degraded by cultured solution of hand bacteria (phylum Proteobacteria was dominant). However, the flm was easily biodegraded when in cultured solution of soil (Firmicutes, especially class Bacilli, was dominant) for 4 weeks at 37 °C, or when buried in the soil itself, both under aerobic conditions (Acidobacteria and Proteobacteria were dominant) for 40 days at room temperature and under anaerobic conditions (Firmicutes, especially family Ruminococcaceae, was dominant) for 5 weeks at 37 °C. Moreover, when flm was buried in the soil, more carbon dioxide was generated than from soil alone. Therefore, the flm was not only brittle but formed of decomposable organic matter. We showed that the flm does not decompose at the time of use when touched by the hand, but it decomposes easily when buried in the soil after use. We suggest that this biodegradable woody flm can be used as a sustainable raw material in the future. In recent years, plastics dumped as garbage afer use have ofen been released into the sea, leading to frequent ingestion of microplastics by marine organisms. Terefore, the low biodegradability of plastics has become a major social problem. Development of materials with high biodegradability is an important approach to help solve this problem. -
Staphylococcus Aureus (Staph Infection)
Staphylococcus aureus (Staph Infection) This sheet talks about exposure to Staphylococcus aureus and Staph infections in a pregnancy and while breastfeeding. This information should not take the place of medical care and advice from your healthcare provider. What is Staphylococcus aureus / a Staph infection? Staphylococcus aureus (Staph) are a type of bacteria (germ). Staph bacteria are commonly found on the skin or in the nose. Most of the time, people will not have problems with these bacteria. However, if Staph gets inside the body through a cut or sore, this could lead to a Staph infection. Staph infection can cause boils or blisters on the skin; or infections in the lungs (pneumonia), bloodstream (sepsis), or in a wound. People with a higher chance of getting a Staph infection include sick people in hospitals, people recovering from surgeries or other medical procedures, people living in over-crowded conditions (shelters or prisons), children in daycare, intravenous (IV) drug users, people with weakened immune systems, people with chronic health conditions (like diabetes or cancer), athletes, and military personnel. Eating food that has been contaminated with Staph bacteria can also cause food poisoning. Symptoms can be severe vomiting and diarrhea with stomach pain that will start within a few hours after exposure. This type of infection with Staph bacteria usually is not serious and generally does not last for more than a day. I am pregnant. If my partner, other family member, or friend has a confirmed Staph skin infection, what can I do to reduce my chances of getting the infection? Do not touch the person’s sores, cuts, or bandages. -

Methicillin-Resistant Staphylococcus Aureus Infections in County Jails
Prevention, Treatment, and Containment of Methicillin-Resistant Staphylococcus aureus Infections in County Jails Texas Department of State Health Services and Correctional Facilities Workgroup September 2006 2 Clinical guidelines are being made available to the public for informational purposes only. Texas Department of State Health Services (DSHS) does not warrant these guidelines for any other purpose and assumes no responsibility for any injury or damage resulting from the reliance thereof. Proper medical practice necessitates that all cases are evaluated on an individual basis and that treatment decisions are patient-specific. 3 We acknowledge the Federal Bureau of Prisons Clinical Practice Guidelines for the Management Of Methicillin-Resistant Staphylococcus Aureus (MRSA) Infections, August 2005 for general organization and content of this document. 4 Table of Contents Introduction ......................................................................................................................... 6 Colonization ......................................................................................................................... 6 Transmission........................................................................................................................ 7 Screening and Surveillance ................................................................................................ 7 Diagnosis .............................................................................................................................. 8 -
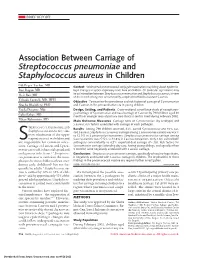
Association Between Carriage of Streptococcus Pneumoniae and Staphylococcus Aureus in Children
BRIEF REPORT Association Between Carriage of Streptococcus pneumoniae and Staphylococcus aureus in Children Gili Regev-Yochay, MD Context Widespread pneumococcal conjugate vaccination may bring about epidemio- Ron Dagan, MD logic changes in upper respiratory tract flora of children. Of particular significance may Meir Raz, MD be an interaction between Streptococcus pneumoniae and Staphylococcus aureus, in view of the recent emergence of community-acquired methicillin-resistant S aureus. Yehuda Carmeli, MD, MPH Objective To examine the prevalence and risk factors of carriage of S pneumoniae Bracha Shainberg, PhD and S aureus in the prevaccination era in young children. Estela Derazne, MSc Design, Setting, and Patients Cross-sectional surveillance study of nasopharyn- geal carriage of S pneumoniae and nasal carriage of S aureus by 790 children aged 40 Galia Rahav, MD months or younger seen at primary care clinics in central Israel during February 2002. Ethan Rubinstein, MD Main Outcome Measures Carriage rates of S pneumoniae (by serotype) and S aureus; risk factors associated with carriage of each pathogen. TREPTOCOCCUS PNEUMONIAE AND Results Among 790 children screened, 43% carried S pneumoniae and 10% car- Staphylococcus aureus are com- ried S aureus. Staphylococcus aureus carriage among S pneumoniae carriers was 6.5% mon inhabitants of the upper vs 12.9% in S pneumoniae noncarriers. Streptococcus pneumoniae carriage among respiratory tract in children and S aureus carriers was 27.5% vs 44.8% in S aureus noncarriers. Only 2.8% carried both Sare responsible for common infec- pathogens concomitantly vs 4.3% expected dual carriage (P=.03). Risk factors for tions. Carriage of S aureus and S pneu- S pneumoniae carriage (attending day care, having young siblings, and age older than moniae can result in bacterial spread and 3 months) were negatively associated with S aureus carriage. -

Insight Into the Genome of Staphylococcus Xylosus, a Ubiquitous Species Well Adapted to Meat Products Sabine Leroy, Aurore Vermassen, Geoffrey Ras, Régine Talon
Insight into the genome of staphylococcus xylosus, a ubiquitous species well adapted to meat products Sabine Leroy, Aurore Vermassen, Geoffrey Ras, Régine Talon To cite this version: Sabine Leroy, Aurore Vermassen, Geoffrey Ras, Régine Talon. Insight into the genome of staphylo- coccus xylosus, a ubiquitous species well adapted to meat products. Microorganisms, MDPI, 2017, 5 (3), 10.3390/microorganisms5030052. hal-01607624 HAL Id: hal-01607624 https://hal.archives-ouvertes.fr/hal-01607624 Submitted on 25 May 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Distributed under a Creative Commons Attribution - ShareAlike| 4.0 International License microorganisms Review Insight into the Genome of Staphylococcus xylosus, a Ubiquitous Species Well Adapted to Meat Products Sabine Leroy, Aurore Vermassen, Geoffrey Ras and Régine Talon * Université Clermont-Auvergne, INRA, MEDIS, F-63000 Clermont-Ferrand, France; [email protected] (S.L.); [email protected] (A.V.); [email protected] (G.R.) * Correspondence: [email protected]; Tel.: +33-473-624-170 Received: 29 June 2017; Accepted: 25 August 2017; Published: 29 August 2017 Abstract: Staphylococcus xylosus belongs to the vast group of coagulase-negative staphylococci. It is frequently isolated from meat products, either fermented or salted and dried, and is commonly used as starter cultures in sausage manufacturing.