2012-2013 West-Champaran, Bihar
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

India: Patna (Bihar) Hospital PPP
Public-Private Partnership Impact Stories India: Patna (Bihar) Hospital PPP Located in eastern India, Bihar is a low income state (LIS) with around 104 million people. According to the Government of India (GoI), over half the population is Below Poverty Line (BPL). In addition, the public health services in Bihar face severe constraints, especially lack of affordable specialty/tertiary care services. There are substantial gaps in health sector infrastructure and essential health requirements, including qualified staff, equipment, drugs, and consumables. As a result, people in the state have to travel to other states for their treatment. To help the state govern- ment improve access to, and availability of, advanced and affordable healthcare, IFC provided advisory assistance to the Government of Bihar and the state’s Infrastructure Development Authority (IDA), to structure and implement a public-private partner- ship (PPP) aimed at building, operating, and maintaining a greenfield super-specialty hospital in Patna, the capital city of the State of Bihar. The project was awarded on a competitive bid process to Global Health Patliputra Private Limited (GHPPL), a unit of Medanta the Medicity, one of India’s largest multi- super specialty hospitals. The concession agreement was signed with GHPPL on 22nd August 2015. The developer will develop the 500 bed super specialty hospital on Design, Build, Finance, Operate, & Transfer (DBFOT)) basis for a concession period of 33 years. This series provides an overview of public-private partnership stories in various infrastructure sectors, where IFC was the lead advisor. IFC’s advisory work was undertaken with financial support from the IFC Advisory Services in Public-Private Partnerships HANSHEP Health PPP facility funded by the UK’s Department for In- 2121 Pennsylvania Ave. -

Constituency-Wise Information on Inclusion and Deletions in Current Electoral Over Previous Roll
ELECTION COMMISSION OF INDIA Format 4B Format 4B (With CEO) Constituency-wise Information on Inclusion and Deletions in Current Electoral Over Previous Roll Name of State: BIHAR Net % Total claims lodged in Total Objections Lodged in Suo-moto Deletion Electors as per proposed Final change Change Electors as per Draft Roll w.r.t. Total Deletions subsequent Assembly Constituency Form 6 after draft Total Claims admitted Form 7 after draft publication Total Objections admitted subsenquent to last Number of Deletions Due to Roll w.r.t. 01.01.2021 as the over over 01.01.2021 as the qualifying date to last publication of roll publication of roll of roll pulication of roll qualifying date previous previuos Final roll Final roll Third Third Third Third Third Third Third Third No Name Male Female Male Female Male Female Male Female Male Female Male Female Male Female Expired Shifted Repeated Male Female (+/-) (+/-) Gender Gender Gender Gender Gender Gender Gender Gender 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 1 Valmiki Nagar 178264 153489 34 6317 5476 3 85 60 0 0 0 0 85 60 0 85 60 0 184499 158902 37 11651 3.39 2 Ramnagar (SC) 155977 139899 10 3372 2676 0 46 28 0 0 0 0 46 28 0 0 1 62 159305 142545 10 5974 1.98 3 Narkatiaganj 141813 123638 16 3340 2798 1 345 296 0 0 0 0 345 296 0 468 80 70 144815 126133 17 5498 2.03 4 Bagaha 162404 142895 15 4055 3721 1 142 155 0 0 0 0 142 155 0 147 25 121 166316 146462 16 7480 2.39 5 Lauriya 137451 118586 11 1999 1647 0 87 68 0 0 0 0 87 68 0 96 28 29 139363 120165 11 3491 -

Ground Water Year Book, Bihar (2015 - 2016)
का셍ााल셍 उप셍ोग हेतू For Official Use GOVT. OF INDIA जल ल MINISTRY OF WATER RESOURCES CENTRAL GROUND WATER BOARD जल ,, (2015-2016) GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) म鵍य पूर्वी क्षेत्र, पटना सितंबर 2016 MID-EASTERN REGION, PATNA September 2016 ` GOVT. OF INDIA जल ल MINISTRY OF WATER RESOURCES जल CENTRAL GROUND WATER BOARD ,, (2015-2016) GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) म鵍य पर्वू ी क्षेत्र, पटना MID-EASTERN REGION, PATNA सितंबर 2016 September 2016 GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) CONTENTS CONTENTS Page No. List of Tables i List of Figures ii List of Annexures ii List of Contributors iii Abstract iv 1. INTRODUCTION.............................................................................................................1 2. HYDROGEOLOGY..........................................................................................................1 3. GROUND WATER SCENARIO......................................................................................4 3.1 DEPTH TO WATER LEVEL........................................................................................8 3.1.1 MAY 2015.....................................................................................................................8 3.1.2 AUGUST 2015..............................................................................................................10 3.1.3 NOVEMBER 2015........................................................................................................12 3.1.4 JANUARY 2016...........................................................................................................14 -

2011-2012 West-Champaran, Bihar
Ch F-X ang PD e w w m w Click to buy NOW! o . .c tr e ac ar DISTRICT HEALTH ACTION PLAN ker-softw 2011-2012 DISTRICT HEALTH SOCIETY West-Champaran, Bihar 1 Ch F-X ang PD e w w m PREFACE w o Click to buy NOW! . .c tr e ac ar ker-softw National Rural Health Mission (NRHM) is one of the major health schemes run by Ministry of health and family welfare, GoI. The basic concept of the mission is to enhance the access of Quality health services to the poorest of the poor of the society and improve the health status of the community. It envisages to improve the health status of the rural mass through various programmes. All the health services should be provided to the pregnant women such as ANC checkups, Post Natal Care, IFA tablets for restricting the enemia cases and other reproductive child health releted services. It also focuses on promotion of institutional delivery for restricting the infant and as well as maternal deaths. Immunization is also a very important component which plays a vital role in child and mother health. Family planning and control of other diseases are also other focus areas. The NRHM has a strong realization that it is important to involve community for the improvement of health status of the community through various stake holders such as ASHA, AWWs, PRI, NGOs etc. ASHA is a link worker between the client and the health service providers. The skill of the health functionaries such as ANMs LHVs should be upgraded through proper orientation to ensure quality of care in health services . -

List of Shortlisted Candidates
Provisionally shortlisted candidates for Zoom Interview for the position of Staff Nurse under NHM, Assam Date of Roll No. Regd. ID Candidate's Name Permanent Address Interview NHM/SNC/2 C/o-Hemen Sarma, H.No.-11, Vill/Town-Forestgate yubnagar narengi, P.O.- 0001 Abhisikha Devi 27.08.2020 413 Narengi, P.S.-Noonmati, Dist.-Kamrup Metro, State-Assam, Pin-781026 NHM/SNC/1 C/o-SAHABUDDIN AHMED, H.No.-115, Vill/Town-RAHDHALA, P.O.- 0002 AFTARA BEGUM 27.08.2020 249 TAKUNABORI, P.S.-MIKIRBHETA, Dist.-Morigaon, State-ASSAM, Pin-782104 C/o-SULTAN SALEH AHMED, H.No.-1107, Vill/Town-WARD NO 5, NHM/SNC/1 0003 AKLIMA KHATUN GANDHINAGAR, P.O.-BARPETA, P.S.-BARPETA, Dist.-Barpeta, State- 27.08.2020 195 ASSAM, Pin-781301 C/o-MR ARUP KUMAR HANDIQUE, H.No.-0, Vill/Town-2 NO MORAN NHM/SNC/1 0004 ALEE HANDIQUE GAON, P.O.-MORAN GAON, P.S.-TITABOR, Dist.-Jorhat, State-ASSAM, Pin- 27.08.2020 489 785630 NHM/SNC/2 C/o-Subodh Bhengra, H.No.-Beesakopie central hospital, Vill/Town-Doomdooma, 0005 Alice Bhengra 27.08.2020 364 P.O.-Doomdooma, P.S.-Doomdooma, Dist.-Tinsukia, State-Assam, Pin-786151 NHM/SNC/2 C/o-Aftab Hoque, H.No.-106, Vill/Town-Puranigudam, P.O.-Puranigudam, P.S.- 0006 Alisha hoque 27.08.2020 478 Samaguri, Dist.-Nagaon, State-Assam, Pin-782141 NHM/SNC/1 C/o-Amrit Daimari, H.No.-126, Vill/Town-Miripara, P.O.-Sastrapara, P.S.- 0007 Alongbar Daimari 27.08.2020 679 Harisinga, Dist.-Udalguri, State-Assam, Pin-784510 NHM/SNC/1 C/o-Benedict Indwar, H.No.-117, Vill/Town-Boiragimath, P.O.-Dibrugarh, P.S.- 0008 ALVIN INDWAR 27.08.2020 928 Dibrugarh, Dist.-Dibrugarh, -
MAPPING of INFORMAL SETTLEMENTS in Muzaffarpur, Bihar
Study Report Study Report MAPPING OF INFORMAL SETTLEMENTS IN Muzaffarpur, Bihar Participatory Research in Asia Content Content Page A General Profile of Muzaffarpur City 2 A General Poverty Profile of Muzaffarpur City 3 Methodology for Listing of Informal Settlements 5 Status of Informal Settlements in Muzaffarpur 5 Challenges and Lessons Learned 12 Annexures Annex.1: Format for Listing of Informal Settlements 14 Annex. 2: List of informal Settlements 16 List of Charts and Figures Chart 1: Decadal Population Growth of Muzaffarpur City 2 Chart 2: Status of Informal Settlements in Muzaffarpur 6 Chart 3: Ownership of Informal Settlement Lands in Muzaffarpur 6 Chart 4: Surrounding Areas of Informal Settlements in Muzaffarpur 7 Chart 5: Type of Physical Location of Informal Settlements in Muzaffarpur 7 Chart 6: Locational Characteristics of Informal Settlements in Muzaffarpur 8 Chart 7: Type of Structures for Majority of Houses in Informal Settlements of Muzaffarpur 8 Chart 8: Approach Road to the Informal Settlements in Muzaffarpur 9 Chart 9: Type of Internal Roads in the Informal Settlements of Muzaffarpur 9 Chart 10: Distance from Nearest Motorable Road for Informal Settlements in Muzaffarpur 10 Chart 11: Presence of Public Institutions in the Informal Settlements of Muzaffarpur 11 Chart 12: Presence of CBOs in the Informal Settlements of Muzaffarpur 11 Chart 13: Presence of NGO Projects in the Informal Settlements of Muzaffarpur 12 Figure 1: Map of Muzaffarpur City Showing All the Wards 3 Figure 2: Map of Muzaffarpur City Showing the Locations of Informal Settlements 4 1 Study Report A General Profile of Muzaffarpur City Muzaffarpur, “the Land of Leechi” was created in 1860s for administrative convenience by splitting up the erstwhile district of Tirhut. -
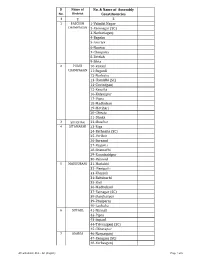
AC with District Dist
Sl Name of No. & Name of Assembly No. District Constituencies 1 2 3 1 PASCHIM 1-Valmiki Nagar CHAMPARAN 2-Ramnagar (SC) 3-Narkatiaganj 4-Bagaha 5-Lauriya 6-Nautan 7-Chanpatia 8-Bettiah 9-Sikta 2 PURVI 10-Raxaul CHAMPARAN 11-Sugauli 12-Narkatia 13-Harsidhi (SC) 14-Govindganj 15-Kesaria 16-Kalyanpur 17-Pipra 18-Madhuban 19-Motihari 20-Chiraia 21-Dhaka 3 SHEOHAR 22-Sheohar 4 SITAMARHI 23-Riga 24-Bathnaha (SC) 25-Parihar 26-Sursand 27-Bajpatti 28-Sitamarhi 29-Runnisaidpur 30-Belsand 5 MADHUBANI 31-Harlakhi 32- Benipatti 33-Khajauli 34-Babubarhi 35-Bisfi 36-Madhubani 37-Rajnagar (SC) 38-Jhanjharpur 39-Phulparas 40-Laukaha 6 SUPAUL 41-Nirmali 42-Pipra 43-Supaul 44-Triveniganj (SC) 45-Chhatapur 7 ARARIA 46-Narpatganj 47-Raniganj (SC) 48-Forbesganj AC with district Dist. - AC (English) Page 1 of 6 Sl Name of No. & Name of Assembly No. District Constituencies 1 2 3 49-Araria 50-Jokihat 51-Sikti 8 KISHANGANJ 52-Bahadurganj 53-Thakurganj 54-Kishanganj 55-Kochadhaman 9 PURNIA 56-Amour 57-Baisi 58-Kasba 59-Banmankhi (SC) 60-Rupauli 61-Dhamdaha 62-Purnia 10 KATIHAR 63-Katihar 64-Kadwa 65-Balrampur 66-Pranpur 67-Manihari (ST) 68-Barari 69-Korha (SC) 11 MADHEPURA 70-Alamnagar 71-Bihariganj 72-Singheshwar (SC) 73-Madhepura 12 SAHARSA 74-Sonbarsha (SC) 75-Saharsa 76-Simri Bakhtiarpur 77-Mahishi 13 DARBHANGA 78-Kusheshwar Asthan (SC) 79-Gaura Bauram 80-Benipur 81-Alinagar 82-Darbhanga Rural 83-Darbhanga 84-Hayaghat 85-Bahadurpur 86-Keoti 87-Jale 14 MUZAFFARPUR 88-Gaighat 89-Aurai 90-Minapur 91-Bochaha (SC) 92-Sakra (SC) 93-Kurhani 94-Muzaffarpur 95-Kanti 96-Baruraj AC with district Dist. -

Bangladesh: Urdu-Speaking “Biharis” Seek Recognition, Respect and Rights Bangladesh: Urdu-Speaking “Biharis” Seek Recognition, Respect and Rights
BANGLADESH: URDU-SPEAKING “BIHARIS” SEEK RECOGNITION, RESPECT AND RIGHTS BANGLADESH: URDU-SPEAKING “BIHARIS” SEEK RECOGNITION, RESPECT AND RIGHTS International Republican Institute IRI.org @IRIglobal © 2020 All Rights Reserved Bangladesh: Urdu-Speaking “Biharis” Seek Recognition, Respect and Rights Copyright © 2020 International Republican Institute. All rights reserved. Permission Statement: No part of this work may be reproduced in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system without the written permission of the International Republican Institute. Requests for permission should include the following information: • The title of the document for which permission to copy material is desired. • A description of the material for which permission to copy is desired. • The purpose for which the copied material will be used and the manner in which it will be used. • Your name, title, company or organization name, telephone number, fax number, e-mail address and mailing address. Please send all requests for permission to: Attn: Department of External Affairs International Republican Institute 1225 Eye Street NW, Suite 800 Washington, DC 20005 [email protected] Cover Image Description: Aerial view of the Biharis Relief Camp, known as the “Geneva Camp.” IRI | BANGLADESH • Urdu-Speaking “Biharis” 3 OVERVIEW In early 2020, the International Republican Institute (IRI) conducted a qualitative research study of the Bihari community in Bangladesh — an Urdu-speaking linguistic minority group in the South Asian nation. The study examined the challenges and needs of Biharis in different locations around Bangladesh. The term “Bihari” refers to approximately 300,000 non-Bengali, Urdu-speaking citizens of Bangladesh who came to what was then East Pakistan mostly from the Indian states of Bihar and West Bengal after the Partition of India in 1947. -

Thursday, July 11, 2019 / Ashadha 20, 1941 (Saka) ______
LOK SABHA ___ SYNOPSIS OF DEBATES* (Proceedings other than Questions & Answers) ______ Thursday, July 11, 2019 / Ashadha 20, 1941 (Saka) ______ SUBMISSION BY MEMBERS Re: Farmers facing severe distress in Kerala. THE MINISTER OF DEFENCE (SHRI RAJ NATH SINGH) responding to the issue raised by several hon. Members, said: It is not that the farmers have been pushed to the pitiable condition over the past four to five years alone. The miserable condition of the farmers is largely attributed to those who have been in power for long. I, however, want to place on record that our Government has been making every effort to double the farmers' income. We have enhanced the Minimum Support Price and did take a decision to provide an amount of Rs.6000/- to each and every farmer under Kisan Maan Dhan Yojana irrespective of the parcel of land under his possession and have brought it into force. This * Hon. Members may kindly let us know immediately the choice of language (Hindi or English) for obtaining Synopsis of Lok Sabha Debates. initiative has led to increase in farmers' income by 20 to 25 per cent. The incidence of farmers' suicide has come down during the last five years. _____ *MATTERS UNDER RULE 377 1. SHRI JUGAL KISHORE SHARMA laid a statement regarding need to establish Kendriya Vidyalayas in Jammu parliamentary constituency, J&K. 2. DR. SANJAY JAISWAL laid a statement regarding need to set up extension centre of Mahatma Gandhi Central University, Motihari (Bihar) at Bettiah in West Champaran district of the State. 3. SHRI JAGDAMBIKA PAL laid a statement regarding need to include Bhojpuri language in Eighth Schedule to the Constitution. -

International Journal of Multidisciplinary Approach and Studies Prognosis of Human Rights and Child Trafficking in Bihar
International Journal of Multidisciplinary Approach and Studies ISSN NO:: 2348 – 537X Prognosis of Human Rights and Child Trafficking in Bihar: A Sociometric Analysis Nikhat Shama Research Scholar, Department of Political Science Jamia Millia Islamia , New Delhi ABSTRACT: Human trafficking, or trafficking in persons, is a form of modern-day slavery and millions of people around the world, including children are victims of this crime (DeStefano, 2007).Violations of human rights are both a cause and a consequence of human trafficking (Robinson, 2002). Every country in the world is affected by human trafficking, whether as a country of origin, transit, or destination, and commonly, as all three. Human trafficking is not just a problem in other countries; cases of human trafficking have also been reported in India, which shares a large border with Nepal and Bangladesh. Under the garb of migration, the traffickers have become active and a large number of young girls are being trafficked from both Bangladesh and Nepal to various places in India, especially to Kolkata, Mumbai and Delhi. Despite increased attention and response to the topic of human trafficking, the empirical state of the literature has seen only marginal developments over time, leaving the magnitude of the problem unknown.The literature on trafficking reflects the dilemma of writing on a subject that is not easy to research and document and yet is too grave an issue to ignore. Considering the hidden and criminal nature of the problem, the data presented by most reports is valuable in face of this scarcity. While the adopted definitions, perspectives and approaches to the problem of trafficking may vary the concern with finding effective solutions is common to these studies. -

The End of Bihari Statelessness Khalid Hussain
30 STATELESSNESS FMR32 The end of Bihari statelessness Khalid Hussain Approximately 160,000 stateless Biharis live in 116 for Bangladeshi citizens – giving makeshift settlements in Bangladesh. Despite recent access to 22 basic services. developments in voter and ID registration, they continue to A three-member delegation from the live in slum-like conditions, facing regular discrimination. camps, including a member of the Association of Young Generation The people known in Bangladesh education and health-care facilities of Urdu-Speaking Community, as ‘Biharis’ or ‘stranded Pakistanis’ hampers community development.1 Geneva Camp, met the Chief Election are the Urdu-speaking descendants Commissioner of Bangladesh in July of Muslims who lived in different Some of the camp residents, 2007 and submitted a petition for the Indian provinces but mostly in Bihar particularly the younger ones, have inclusion of camp residents in the and who, at India’s partition in 1947, been struggling for years to be new list of voters. On 6 September 2007, the government agreed to give citizenship to those Urdu- speaking Biharis born after 1971 or who were under 18 years at the date of the creation of Bangladesh. In November 2007, twenty-three eminent academics, journalists, lawyers and human rights activists, in a joint statement, urged the government to offer citizenship rights, in line with the country’s constitution, to all Urdu-speaking people in camps in Bangladesh. In August 2008, the Election Commission began a drive to register the Urdu-speaking communities in the settlements around Bangladesh. This was an important first step towards integrating these minority communities into Bangladeshi society. -

Annexure-V State/Circle Wise List of Post Offices Modernised/Upgraded
State/Circle wise list of Post Offices modernised/upgraded for Automatic Teller Machine (ATM) Annexure-V Sl No. State/UT Circle Office Regional Office Divisional Office Name of Operational Post Office ATMs Pin 1 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA PRAKASAM Addanki SO 523201 2 Andhra Pradesh ANDHRA PRADESH KURNOOL KURNOOL Adoni H.O 518301 3 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM AMALAPURAM Amalapuram H.O 533201 4 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Anantapur H.O 515001 5 Andhra Pradesh ANDHRA PRADESH Vijayawada Machilipatnam Avanigadda H.O 521121 6 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA TENALI Bapatla H.O 522101 7 Andhra Pradesh ANDHRA PRADESH Vijayawada Bhimavaram Bhimavaram H.O 534201 8 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA VIJAYAWADA Buckinghampet H.O 520002 9 Andhra Pradesh ANDHRA PRADESH KURNOOL TIRUPATI Chandragiri H.O 517101 10 Andhra Pradesh ANDHRA PRADESH Vijayawada Prakasam Chirala H.O 523155 11 Andhra Pradesh ANDHRA PRADESH KURNOOL CHITTOOR Chittoor H.O 517001 12 Andhra Pradesh ANDHRA PRADESH KURNOOL CUDDAPAH Cuddapah H.O 516001 13 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM VISAKHAPATNAM Dabagardens S.O 530020 14 Andhra Pradesh ANDHRA PRADESH KURNOOL HINDUPUR Dharmavaram H.O 515671 15 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA ELURU Eluru H.O 534001 16 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudivada Gudivada H.O 521301 17 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudur Gudur H.O 524101 18 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Guntakal H.O 515801 19 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA